12
Application of 3D TMJ Imaging to TMJDs, TMJ Functional Analyses, and Orthodontic Treatment Outcomes
Introduction
The temporomandibular joint (TMJ) is a structure of substantial importance in clinical orthodontics. During growth, the joint components influence the development of the relationships between the upper and lower jaws, the occlusion, and the functioning masticatory system. In adults, the health of the TMJ and masticatory system depends on the capacity of these joint components to adapt to normal or abnormal function. TMJ pathologies that result in alterations to the size, form, and spatial and functional relationships of the joint components can lead to progressive changes and compensations that ultimately may affect jaw and tooth positions and occlusion. Such pathological TMJ conditions include temporomandibular joint disorders (TMJDs; also referred to as temoporomandibular disorders or TMD) and developmental disorders such as condylar hyperplasia, hypoplasia, or aplasia. TMJDs in turn include internal derangement or disc displacement, arthralgia, osteoarthritis (OA), and osteoarthrosis. Occlusal and functional changes associated with these pathological conditions include progressive anterior openbite and limitation or deviation of jaw movements (Helenius et al., 2005; Koyama et al., 2007; Alexiou et al., 2009; Yura et al., 2010).
The current diagnoses of TMJDs are based largely on signs and symptoms of the disease. However, it is acknowledged widely that an ideal diagnostic classification system for any disease or disorder including TMJDs should be based on etiology (National Institues of Health Technology Assessment Conference Statement on the Diagnosis and Management of TMDs, 1996). The first step toward an etiology-based system was introduced in 1992 (Dworkin & LeResche, 1992) and was known as the Research Diagnostic Criteria for temporomandibular disorders (RDC/TMD). The RDC/TMD index includes two axes: Axis I is related to physical diagnoses, primarily based on clinical signs and symptoms; Axis II incorporates the psychological status of the patient and pain-related disability. This system has been used in many studies to date and is the basis of ongoing large-scale multisite epidemiological studies (Maixner et al., 2011). The results of projects that validate the RDC/TMD have been reported recently (Anderson et al., 2010; Ohrbach et al., 2010; Truelove et al., 2010; Look et al., 2010a; Schiffman et al., 2010a, 2010b) and the scientific evidence for clinical treatment of TMJDs has been reviewed (Cairns, 2010; List & Axelsson, 2010; Michelotti & Iodice, 2010; Ohrbach, 2010), setting the stage for improved approaches for diagnosing (Zhao et al., 2011; Gonzalez et al., 2011b) and treatment of TMJDs (Greene, 2010).
Imaging data currently are recommended to help differentiate the diagnosis of disc displacement diagnoses and arthralgia, OA, and osteoarthrosis (Look et al., 2010b). Indeed, the RDC/TMD validation project supports the use of imaging to enhance the Axis I physical diagnoses protocol. Hence, the recommended TMJ imaging has evolved to include computed tomography (CT) and cone beam CT (CBCT) for diagnosis of osseous degenerative changes, and magnetic resonance imaging (MRI) for detecting disc displacements and effusion (Ahmad et al., 2009). Comprehensive imaging criteria for TMJ diagnoses have been validated for image acquisition and analysis using CT (and by extension CBCT), MRI, and panoramic radiographs (Ahmad et al., 2009). Furthermore, the validated combination of multidimensional imaging with computer-aided numerical modeling has produced novel insights and enhanced our understanding of the normal function and pathomechanics of the human masticatory apparatus. The increased use of CBCT, MRI, and joint kinematics methods allow us to understand better TMJ tissue dynamics during growth and aging that include adaptive and therapeutic remodeling as well as pathologic degradation and proliferation. However, despite the importance of TMJ morphologic assessment derived from imaging, treatment evaluations and risk assessments of TMJDs also must take into consideration function, pain and biological perspectives for the full clinical value of diagnostics to be realized. For this reason, in addition to providing an in-depth background on the applications of three-dimensional (3D) imaging to TMJD diagnostics and therapeutics, this chapter highlights clinical and biological data that are essential to attain comprehensive insights on the causes and pathogenesis of these disorders. A discussion on the known changes within the TMJ in response to growth modification orthodontic therapies also is included. Finally, since the applications of CBCT in the clinical assessment of the TMJs are still under study and development, we also have incorporated an overview of recent advances in methodologies and technologies that eventually will help in moving the diagnostic uses of 3D imaging into the clinical arena.
Imaging of the TMJ
TMJDs include developmental and acquired disorders of the TMJ. Acquired disorders of the TMJ comprise arthralgia and inflammatory disorders such as rheumatoid arthritis (RA) and OA, disc dislocation or internal derangement, ankylosis, and fracture (Leeuw, 2008). While these diagnostic classifications are based primarily on clinical signs and symptoms, clinical examination alone is insufficient to describe fully the disease status and aid in the development of protocols for the management of hard tissue pathologies of the TMJ. Imaging is a necessary element in the diagnostic process (Petersson, 2010), but also is insufficient on its own for the management of disease (Wiese et al., 2011).
Conventional radiographic imaging of the TMJ using panoramic radiographs and cephalograms results in disorted images with superimposed structures. Given that imaging with panoramic radiographs is unreliable and has a low sensitivity, analysis for structural changes using this imaging modality generally has been limited to evaluating gross changes in joint anatomy (Ahmad et al., 2009; Shintaku et al., 2009). Advancements in CT technologies and the introduction of CBCT with reduced radiation doses and costs relative to CTs have resulted in its increased utilization as the primary diagnostic imaging method for assessing TMJ bone morphology. CBCT is at least as reliable as conventional CT in detection of TMJ bone tissue changes and has superior reliability and greater accuracy than conventional tomograms in detecting TMJ erosions (Honda et al., 2006; Honey et al., 2007).
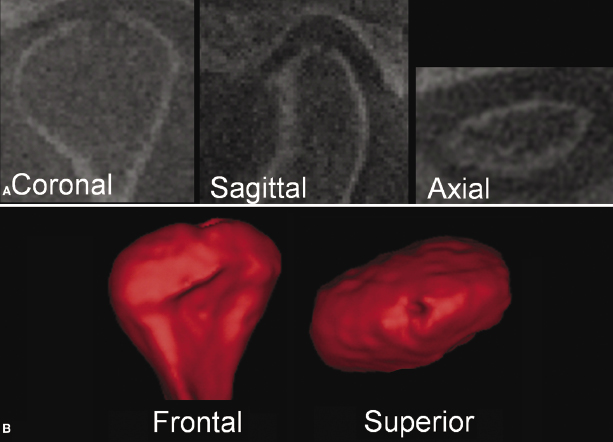
CBCT allows evaluation of TMJ hard tissue morphology and enables visualization of a wide spectrum of minor to overt osseous changes resulting from pathology, growth, and adaptive processes. A radiographic examination of the TMJ is an essential part in the diagnosis and management of TMJ diseases involving the bone that supports the articulating tissues. CBCT also allows for accurate detection and evaluation of pathological changes (Honda et al., 2006; Honey et al., 2007). Relative to conventional 2D radiography, the precise rendering of virtual 3D surface models of the TMJ bone anatomy enables practitioners to provide earlier and accurate identification of aberrations in the bone morphology (Figure 12.1) and in the congruency of bone surfaces that define the joint space (Crow et al., 2005) in 3D. The following sections describe how CBCT can be utilized for (1) the diagnosis of different types of TMJ arthritides, (2) better understanding of TMJ bone remodeling, (3) specific applications of TMJ evaluations in orthodontic patients, and (4) 3D superimpositions for evaluating four-dimensional (4D) changes in TMJ bone architecture.
Arthritides and Degenerative Joint Diseases
3D imaging of the TMJ provides essential information for detecting inflammatory and degenerative conditions of the TMJ bony tissues and to determine accurate intervention by longitudinally monitoring progression and responses to treatment (Okeson, 1996). The utility of 3D imaging applies to conditions such as OA, RA, juvenile idiopathic arthritis, psoriatic arthritis, gout, ankylosing spondylitis, idiopathic condylar resorption, and other less common diseases. Radiographic features of arthritides in the TMJ are similar regardless of whether the condition is local, such as for OA, or systemic, as in RA. Progression of OA, however, can be slower than that of RA, making radiographic signs less evident in OA compared with RA. Radiographic signs of bony changes associated with TMJ arthritides include irregular and possibly thickened cortical outlines (sclerosis), erosions, osteophyte formation, subchondral cysts, and flattening and narrowing of the joint space (Gynther et al., 1996; Ahmad et al., 2009; Alexiou et al., 2009). In RA, when erosions are detected early, they also may predict progression and severity (van der Heijde et al., 1992; van der Heijde, 1995; Forslind et al., 2009).
CBCT images allow reliable detection and localization of hard tissue structural changes. The efficacy of CBCT for detecting osseous changes is superior to that of plane tomography and MRI (Honey et al., 2007; Alkhader et al., 2010). Possible indications for imaging of the TMJs with CBCTs include detection of bone abnormalities, characterization of the condylar and articular fossa bone morphology, diagnosis of the stage of bone morphologic changes, assessment of the progression of bony changes over time, or the response to a specific treatment (Ahmad et al., 2009; De Vos et al., 2009). The use of CBCT for orthodontic reasons also may increase the possibility for early detection of TMJ degenerative processes in an otherwise asymptomatic patient.
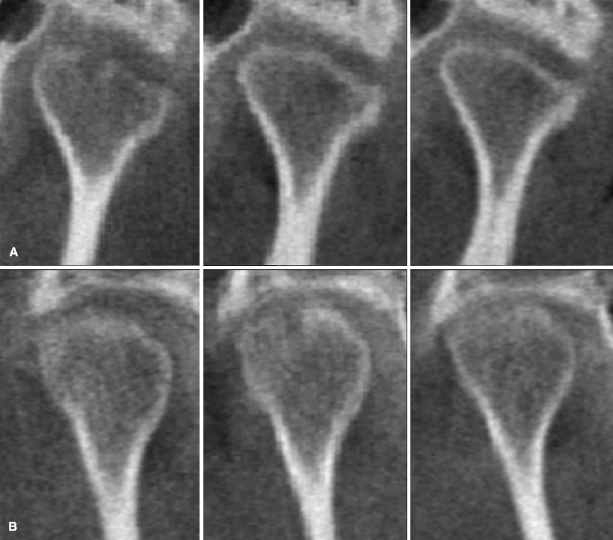
Upon diagnosis of initial signs of active TMJ destruction in a CBCT scan, it is essential to monitor active disease, either localized to the TMJ or systemic, before loading the joints with orthodontic/orthopedic forces or undertaking jaw surgery. Interpretation of CBCT findings, therefore, should be part of a complete analysis of the dental and medical history, as well as charting of the TMJ clinical signs and symptoms prior to the start of the orthodontic treatment. If a systemic inflammatory condition is suspected at the clinical examination, the patient should be referred for a medical evaluation, including necessary serological evaluation. It is important to keep in mind that structural bony changes of the TMJ alone do not reveal whether or not the disease is active, since there is no direct correlation between TMJ morphological changes and clinical findings in OA or RA (Celiker et al., 1995; Hajati et al., 2009). Early diagnosis and treatment of destructive inflammatory conditions is important to further control bone destruction successfully (Allaart et al., 2006). As demonstrated in Figure 12.2 and as validated by studies regarding other joints, controlling the inflammation in patients with RA leads to repair of bone through formation of new bone at the base of deep erosions (Finzel et al., 2011). Control of local inflammation, therefore, should be an important clinical goal for these patients.
Besides the radiographic signs of joint destruction in RA, there are several common risk factors for disease progression including systemic inflammatory markers, the shared epitope (SE) allele for the human leukocyte antigen (HLA), the presence of rheumatoid factor (RF), estrogen deficiency, and being female. A promising marker with high diagnostic specificity for RA is an antibody to cyclic citrullinated peptides (anti-CCP; Pfeilschifter et al., 2002; van Venrooij et al., 2003; Vittecoq et al., 2004; Sanmartí et al., 2007; Syversen et al., 2008). Anti-CCP has been shown to predict RA more than 10 years before disease onset and to be a strong predictor of progression of joint destruction (Aho et al., 1991, 1993; Rantapää-Dahlqvist et al., 2003; Forslind et al., 2004). It still is unknown whether appropriate markers or predictors may be detectable in other arthritides, such as idiopathic condylar resorption, in otherwise clinically and radiographically healthy individuals.
3D quantification of bony changes in TMJ condylar surface models constructed from CBCT volumes has been performed recently using shape correspondence analysis (Cevidanes et al., 2010). Condylar resorption and apposition was localized and quantified in patients with TMJ OA, and the morphology was compared with a group of healthy controls. This method measures defects within 0.5 mm of the true defect size in simulation studies and in longitudinal follow-up of disease progression (Paniagua et al., 2011). Software tools for comparing TMJ structural abnormalities across patients that will aid in developing a 3D diagnostic index of morphological variability currently are under development. The biggest challenge toward achieving this goal is deriving a dataset of a 3D population reference standard of normal TMJ morphologies when considerable individual variability exists in TMJ form and size among individuals and age groups.
As with CBCT, MRI is a noninvasive tomographic imaging technique that can produce cross-sectional images in any plane without morphologic distortion or magnification. In addition, MRI enables visualization of joint abnormalities not seen with any other imaging method and, thus, is considered to be the best method for diagnostic assessment of the TMJ status (Larheim, 2005). MRI is the only technique that allows simultaneous examination of all components of the TMJ, including soft tissues, articular cartilage, and bone, without ionizing radiation and its adverse effects. The value of MRI for the detection of TMJ osseous abnormalities, however, is considered to be limited in comparison to CBCT (Alkhader et al., 2010). Changes in TMJ bone marrow signals can be demonstrated with MRI revealing edema and osteonecrosis (Lieberman et al., 1996; Larheim et al., 1999). Since bone marrow changes on MRIs from hands and feet in early RA are an indicator for development of joint destruction (Conaghan et al., 2003; McQueen et al., 2003), similar findings for the TMJ may offer early indicators of future destructive changes.
Internal Derangements of the TMJ
Ultrasound and MRI have been used to monitor synovitis and cartilage degradation in the knee (Peterfy et al., 2008) and the TMJ (van Dijke et al., 1997). Unlike the knee joint in which the bone is covered with hyaline cartilage, the mandibular condyle and eminence of the TMJ are lined by a thin layer of fibrocartilage. In addition, the TMJ disc that normally lies between the bony components also is comprised of fibrocartilage. The normal TMJ, as seen by MRI, is characterized differently in each cross-sectional view and jaw position. In the sagittal plane closed-mouth view, the disc clearly is depicted as a low-signal intensity band of biconcave-lens-like configuration. The posterior band lies approximately at the 12 o’clock position relative to the condylar head (Figure 12.3A). In the sagittal plane open-mouth view, the disc has a “bow tie” configuration and maintains its position between the condyle and the articular eminence (Figure 12.3B). The posterior disc attachment has a bright signal relative to the posterior band of the disc due to its rich network of fatty tissue. In the coronal plane, the disc has an arc-shaped configuration with the medial margin of the disc attaching to the medial pole of the condyle and with the lateral margin attaching to the lateral pole of the condyle.
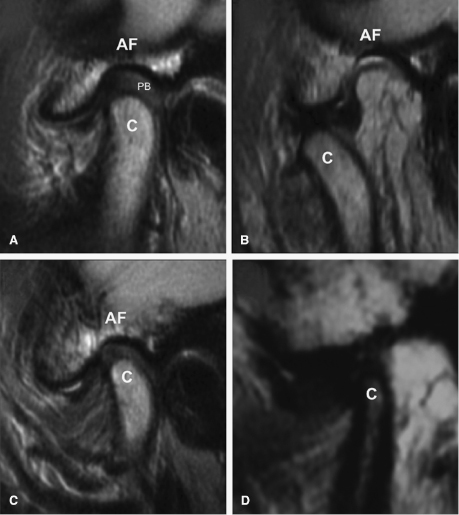
Because of its ability to visualize the nonmineralized “soft tissues” of the disc and articular fibrocartilage in the TMJ, MRI is a preferable and proven method for the assessment of changes in morphology and/or spatial relationships that these tissues undergo during internal derangements of the TMJ, including joint effusion and disc displacements (Katzberg, 1990). Articular disc derangements may involve disc displacements and deformation. Displacements from the normal disc position may be partial or complete displacements of the disc away from the condylar head (Figure 12.3C). In open-mouth position, the disc may or may not be recaptured over the condylar head (Figure 12.3D). Coronal cross-sections can reveal medio-lateral disc displacements. Disc displacement is found in approximately 80% of patients with TMJ symptoms (Tasaki et al., 1996). Additionally, Larheim and colleagues (2001) have reported that asymptomatic volunteers also may present early-stage disc displacement. More specifically, they found that while complete disc displacement is present in 40% of symptomatic joints compared with 2.4% of asymptomatic joints, partial disc displacement occurred in 22.6% and 21.8% of symptomatic and asymptomatic joints, respectively.
Large accumulations of joint fluid are seen only in symptomatic patients (Larheim et al., 2001). Joint effusion is defined as the presence of increased intra-articular fluid and is seen best in T2-weighted closed-mouth MRI as an increased signal area (hyperintense signal) in the joint space. On opening the mouth, the accumulation is displaced within the joint space.
TMJ Bone Tissue Remodeling
Continuous remodeling of the TMJ bony structures is a physiologic process aimed at adapting the articular surfaces to mechanical forces applied to the joint. This process continues during growth through late adulthood and is an essential biological response to normal functional demands, thereby ensuring homeostasis of joint form and function and maintenance of occlusal relationships (Smartt et al., 2005). Bone tissue remodeling is accomplished by coordinated intercellular signals between the bone-forming osteoblasts and bone-resorbing osteoclasts, which, in turn, are thought to be induced by mechanical loading and controlled by locally produced cytokines, growth factors, hormones, and neuroregulators (Abe et al., 1988; Lacey et al., 1998; Shevde et al., 2000; Michael et al., 2005; Lerner, 2006a; Galal et al., 2008). The pathogenic mechanisms that cause a predominance of bone tissue resorption under these circumstances might share several pathways in common with RA and periodontitis, two distinct conditions that are characterized with an overreactive inflammatory response (Lerner, 2006b).
The TMJ is subject to mechanical loading by normal- and para-function and orthopedic interventions; therefore, mechanical loading is a risk factor for articular bone resorption in individuals who have enhanced inflammatory response (i.e., Juvenile Idiopathic Arthritis [JIA] and RA). Interestingly, idiopathic articular bone tissue resorption may occur spontaneously without any diagnosis of general inflammatory disease or clinical signs and symptoms (Figure 12.4).
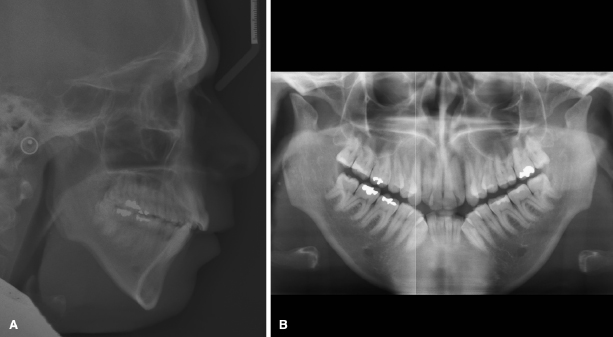
Image-Assisted Evaluation of the TMJ in Orthodontic Treatment
CBCT scans are indicated as part of the diagnostic records for specific clinical situations and may provide information regarding the TMJ’s adaptive capacity in response to orthodontic treatment. One important example of the latter includes the longitudinal assessment of TMJ bone tissue adaptation to mandibular advancement strategies. Earlier studies using CT have shown that orthopedic mandibular advancements with Herbst appliance result in condylar bone apposition and remodeling of the glenoid fossa in children and adolescents. Further studies using MRI have demonstrated that even nongrowing individuals can respond to orthopedic loading of the TMJ with resultant condylar bone apposition (Ruf & Pancherz, 1998, 1999). Finally, 3D CBCT imaging has been used to visualize successful treatment effects of distraction splint therapy during growth on mandibular asymmetry in unilateral manifestation of JIA (Stoustrup et al., 2011).
Although previous work has assessed morphologic changes qualitatively in response to growth modification appliances, newer methodologies are becoming available that might provide better insights into these changes. Thus, the assessment of responses of the TMJ during therapies aimed at growth adaptation or therapeutic remodeling is an area in which 3D data acquisition from CBCT may be a valuable tool in enhancing our understanding and knowledge of the precise localization of treatment effects as well as the quantity of the changes achieved. Careful registration of 3D images is required to improve our current knowledge of TMJ bone tissue remodeling and displacements, evaluation of progress of orthodontic therapies or arthritis treatments, as well as risk assessments for disease. Additionally, CBCT scans and 3D models may enable the localization and quantification of previously unidentified bone tissue growth, remodeling, and degenerative patterns. However, in addition to using contemporary quantitative TMJ imaging approaches, it is essential to have a deeper understanding of its biological and functional attributes to better comprehend TMJ 3D morphology and the dynamics of its changes with orthodontic treatment and disease.
3D Superimpositions for Evaluation of 4D Changes in the TMJ Bone
CBCT has been utilized to assess condylar remodeling longitudinally in treatment outcomes of surgery for almost a decade and, more recently, for determining changes during TMJ arthritides. The use of validated surface modeling and shape analysis quantification techniques for quantifying and localizing bone defects during progression and treatment of arthritis is illustrated in Figure 12.5 (Paniagua et al., 2011). These models demonstrate the longitudinal development and partial repair of TMJ erosion. The patient was diagnosed with RA shortly before the first CBCT acquisition and a 3D model was processed (Figure 12.5B, left). There were no signs or symptoms in the TMJ disease at the time of the initial records or at the follow-ups. When active TMJ bone tissue resorption was discovered at the 1-year follow-up (Figure 12.5B, middle), local corticosteroid treatment was administered to suppress the pathologic inflammation. At the 2-year follow-up, the resorbed bone was rebuilt partially (Figure 12.5B, right). The magnitude and location of changes in bone contours between any two pairs of time points are depicted in Figure 12.5C.
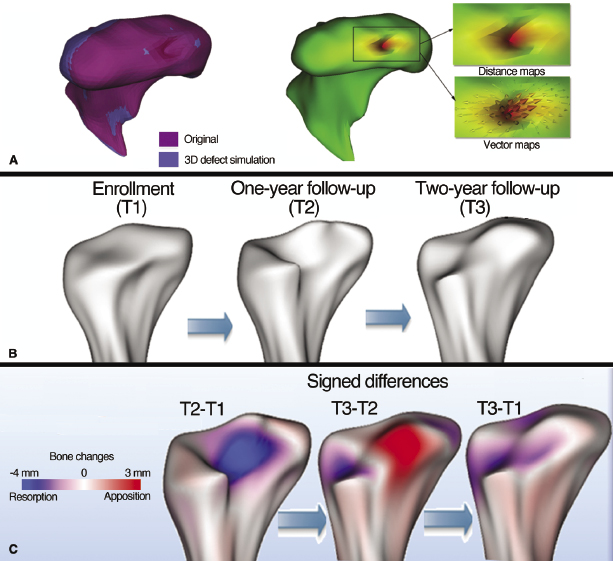
Currently, superimposition of 3D surface models and shape analysis still is too time-consuming and computing-intensive to apply to routine clinical use. Several barriers including radiation doses (see Chapters 2 and 3), construction of CBCT surface models, image registration, and optimal methods for quantitation of the changes need to be overcome prior to more widespread use of CBCT for diagnostic or therapeutic imaging for longitudinal quantitative assessment of changes in the TMJ being performed routinely. Several of these challenges and their potential solutions toward a wider use of TMJ CBCT imaging are detailed below.
Construction of 3D Surface Models and Image Registration
Longitudinal quantitative assessment of bony changes requires construction of 3D surface models. Segmentation—the process of constructing 3D models by examining cross-sections of a volumetric data set to outline the shape of structures—remains a challenge (Adams & Bischof, 1994; Lie, 1995; Ma & Manjunath, 2000; Moon et al., 2002), particularly when applied to physiologic or pathologic bone resorption and apposition of thin cortical bone areas in the TMJ condyles. The methods described by Gerig and coworkers (2003) addressing these technical difficulties, have been adapted by Cevidanes and associates (2005) to construct 3D craniofacial models, and more recently, have been applied to the TMJ.
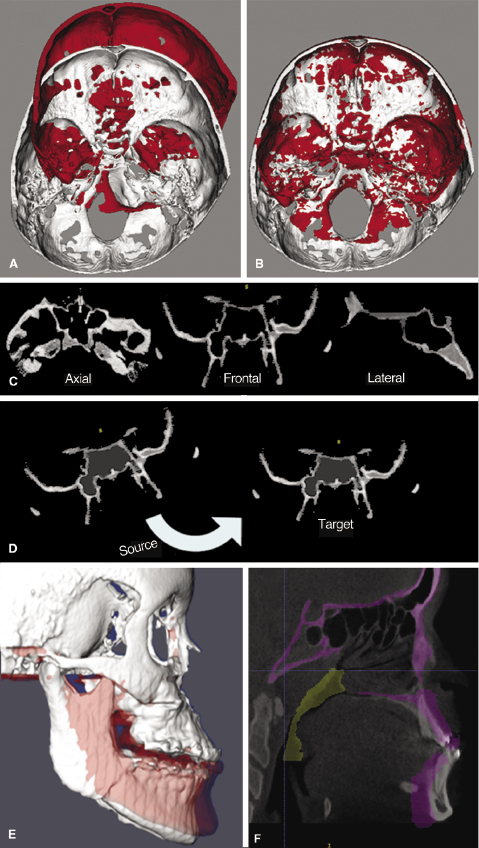
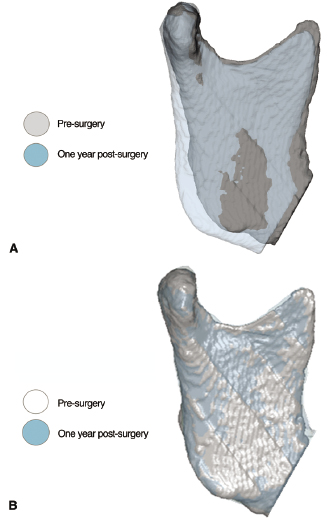
Image registration is a core technology for many imaging tasks. The two most commonly used approaches for CBCT image registration applicable to the TMJ include cranial base superimpositions and regional superimpositions. Such superimpositions can be based on landmarks of reference or surfaces or the gray-level voxels of the CBCT volume. The methodology of choice for cranial base superimpositions has been developed into a sequence of fully automated volume-based registration (Figure 12.6). The major strength of these methods is that registration does not depend on the precision of the 3D surface models. The cranial base models are used only to mask anatomic structures that change with growth and treatment. The registration procedures actually compare the gray-level CBCT images containing only the cranial base voxel-by-voxel to calculate rotation and translation parameters between the two images and to register them on stable anatomic sites in 3D. As with 2D cephalometrics, cranial base superimpositions of 3D CBCT images assess longitudinal displacements of the condyle relative to the cranial fossa (Carvalho Fde et al., 2010; Motta et al., 2011), but do not separate these displacements from bone remodeling. Such an analysis to determine longitudinal changes in condylar remodeling (Figure 12.7A) and comparisons of condylar morphology across subjects requires regional superimpositions using surface-to-surface rigid registration on areas of the condylar neck and ramus (Figure 12.7B; Cevidanes et al., 2010).
Quantitative Measurements
Precise quantitative measurements are required for characterization of TMJ arthritides and longitudinal assessments of individual responses to diverse clinical protocols in order to support clinical decisions and to translate this knowledge to the needs of indivi/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


