Additional Conservative Esthetic Procedures
Significant improvements in tooth-colored restorative materials and adhesive techniques have resulted in numerous conservative esthetic treatment possibilities. Although restorative dentistry is a blend of art and science, conservative esthetic dentistry truly emphasizes the artistic component. As Goldstein stated, “Esthetic dentistry is the art of dentistry in its purest form.”1 As with many forms of art, conservative esthetic dentistry provides a means of artistic expression that feeds on creativity and imagination. Dentists find performing conservative esthetic procedures enjoyable, and patients appreciate the immediate esthetic improvements rendered, often without the need for local anesthesia.
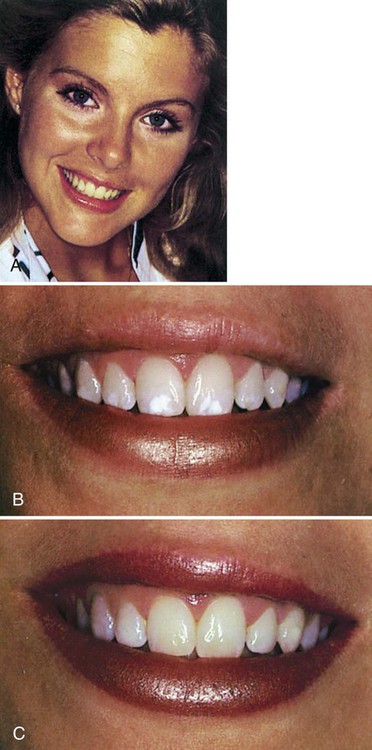
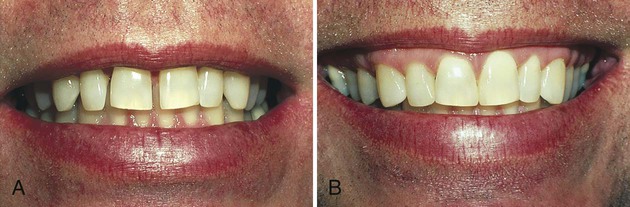
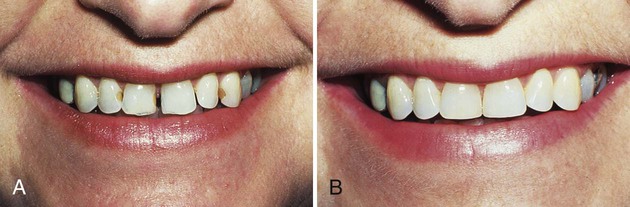
One of the greatest assets a person can have is a smile that shows beautiful, natural teeth (Fig. 12-1). Children and teenagers are especially sensitive about unattractive teeth. When teeth are discolored, malformed, crooked, or missing, often the person makes a conscious effort to avoid smiling and tries to “cover up” his or her teeth. Correction of these types of dental problems can produce dramatic changes in appearance, which often result in improved confidence, personality, and social life. The restoration of a smile is one of the most appreciated and gratifying services a dentist can render. The positive psychological effects of improving a patient’s smile often contribute to an improved self-image and enhanced self-esteem. These improvements make conservative esthetic dentistry particularly gratifying for the dentist and represent a new dimension of dental treatment for patients.
This chapter presents conservative esthetic procedures in the context of their clinical applications. The principles and clinical steps involved in adhesive bonding for the treatment alternatives discussed in this chapter are similar to those described in Chapters 8 to 10. Only specific conservative esthetic clinical procedures or variations from previously described techniques are presented in this chapter.
Artistic Elements
Shape or Form
When viewing the clinical crown of an incisor from a facial (or lingual) position, the crown outline is trapezoidal. Subtle variations in shape and contour produce very different appearances, however. Rounded incisal angles, open incisal and facial embrasures, and softened facial line angles typically characterize a youthful smile. A smile characteristic of an older individual having experienced attrition secondary to aging, typically exhibits incisal embrasures that are more closed and incisal angles that are more prominent (i.e., less rounded). Frequently, minor modification of existing tooth contours, sometimes referred to as cosmetic contouring, can effect a significant esthetic change (see section on alterations of shape of natural teeth). Reshaping enamel by rounding incisal angles, opening incisal embrasures, and reducing prominent facial line angles can produce a more youthful appearance (Fig. 12-2).
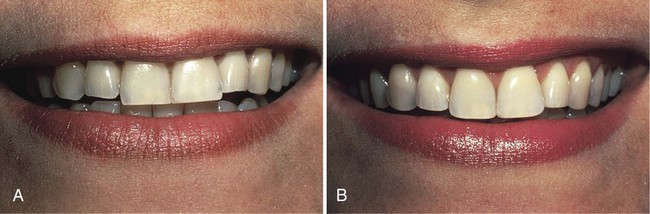
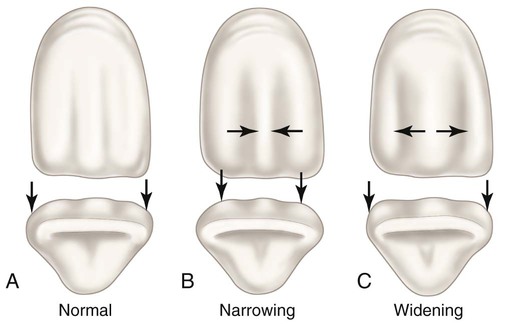
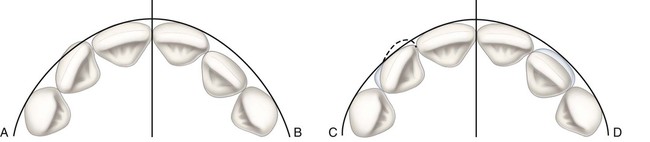
The apparent size of a tooth can be changed by altering the position of facial prominences or heights of contour without changing the actual dimension of the tooth. Compared with normal tooth contours (Fig. 12-3, A), a tooth can be made to appear narrower by positioning the mesiofacial and distofacial line angles closer together (see Fig. 12-3, B). Developmental depressions also can be positioned closer together to enhance the illusion of narrowness. Similarly, greater apparent width can be achieved by positioning the line angles and developmental depressions further apart (see Fig. 12-3, C).
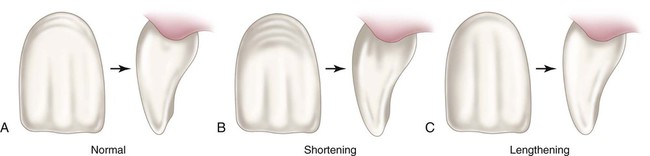
Although more difficult, the apparent length of teeth also can be changed by illusion. Compared with normal tooth contours (Fig. 12-4, A), a tooth can be made to appear shorter by emphasizing the horizontal elements such as gingival perikymata and by positioning the gingival height of contour further incisally (see Fig. 12-4, B). Slight modification of the incisal area, achieved by moving the incisal height of contour further gingivally, also enhances the illusion of a shorter tooth. The opposite tenets are true for increasing the apparent length of a tooth. The heights of contour are moved farther apart incisogingivally, and vertical elements such as developmental depressions are emphasized (see Fig. 12-4, C).
Used in combination, these illusionary techniques are particularly valuable for controlling the apparent dimension of teeth in procedures that result in an actual increased width of teeth, such as in diastema (i.e., space) closure (see the section on Correction of Diastemas). By contouring the composite additions in such a way that the original positions of the line angles are maintained, the increased widths of the restored teeth are less noticeable (Fig. 12-5). If full facial coverage restorations are placed in conjunction with a diastema closure, vertical elements can be enhanced and horizontal features de-emphasized to control further the apparent dimension of teeth.
Symmetry and Proportionality
The overall esthetic appearance of a human smile is governed largely by the symmetry and proportionality of the teeth that constitute the smile. Asymmetric teeth or teeth that are out of proportion to the surrounding teeth disrupt the sense of balance and harmony essential for optimal esthetics. Assuming that the patient’s teeth are aligned normally (i.e., rotations or faciolingual positional defects are not present), dental symmetry can be maintained if the sizes of contralateral teeth are equivalent. A dental caliper should be used in conjunction with any conservative esthetic dental procedure that would alter the mesiodistal dimension of teeth. This recommendation is particularly true for procedures such as diastema closure or other procedures involving augmentation of proximal surfaces with composite. By first measuring and recording the widths of the interdental space and the teeth to be augmented, the appropriate amount of contour to be generated with composite resin addition can be determined (Fig. 12-6). In this manner, symmetric and equal tooth contours can be generated (see the section on Correction of Diastemas). When dealing with restorations involving the midline, particular attention also must be paid to the incisal and gingival embrasure forms; the mesial contours of both central incisors must be mirror images of one another to ensure an optimally symmetric and esthetic result.
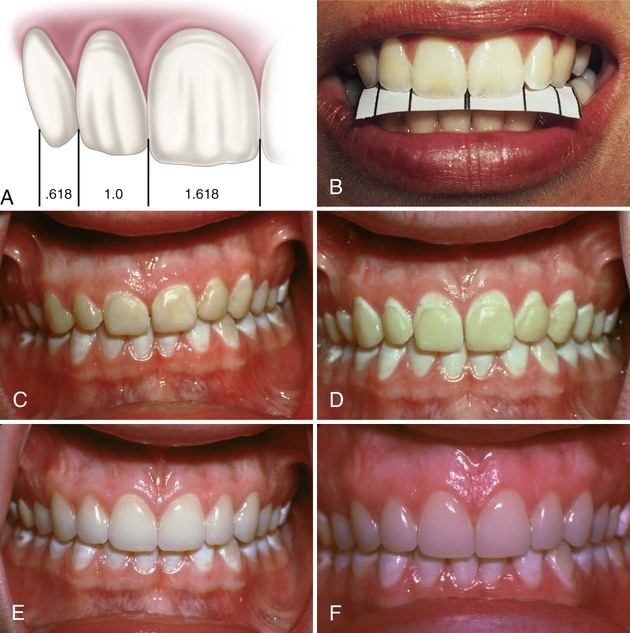
In addition to being symmetric, anterior teeth must be in proper proportion to one another to achieve maximum esthetics. The quality of proportionality is relative and varies greatly, depending on other factors (e.g., tooth position, tooth alignment, arch form, configuration of the smile). One long-accepted theorem of the relative proportionality of maxillary anterior teeth typically visible in a smile involves the concept of the golden proportion.2 Originally formulated as one of Euclid’s elements, this theorem has been relied on through the ages as a geometric basis for proportionality in the beauty of art and nature.3 On the basis of this formula, a smile, when viewed from the front, is considered to be esthetically pleasing if each tooth in that smile (starting from the midline) is approximately 60% of the size of the tooth immediately mesial to it. The exact proportion of the distal tooth to the mesial tooth is 0.618 (Fig. 12-7, A). These recurring esthetic dental proportions are based on the apparent sizes of teeth when viewed straight on and not the actual sizes of individual teeth. An example of an esthetically pleasing smile that meets the golden proportion can be seen in Figure 12-7, B.
Although the golden proportion is not the absolute determinant of dental esthetics, it does provide a practical and proven guide for establishing proportionality when restoring anterior teeth, especially if these teeth are considered long. However, according to a study by Preston, only 17% of the population naturally exhibits smiles that meet the golden proportion as the recurring esthetic dental proportion.4 According to a survey of dentists by Ward, a recurring esthetic dental proportion of 70% (as opposed to 61.8 % as with the golden proportion) is preferred when teeth are of normal dimension.5
Little scientific information is available regarding the proper proportions of individual anterior teeth. A study by Sterrett et al. revealed that the average width-to-length ratio for a maxillary central incisor in men was 0.85 and in women was 0.86.6 The actual width-to-length ratios found in this same study for maxillary lateral incisors in men and women were 0.76 and 0.79, respectively. Another study by Magne et al. reported average width-to-length ratios of 0.87 for worn maxillary central incisors and 0.78 for unworn maxillary central incisors.7 An accepted theorem for achieving esthetically pleasing central incisors maintains that the ideal width-to-length ratio should be 0.75 to 0.80.8 This ratio represents the ideal proportions needed to optimize the esthetic result and can help guide the treatment planning process. Considering the range of recommended width-to-length ratios, 0.80 seems to be a good benchmark for achieving optimally esthetic results when restoring maxillary central incisors and 0.75 for maxillary lateral incisors.
A good example can be seen in Figure 12-7, C through F. Because of altered passive eruption, this teenaged patient exhibited a preoperative width-to-length ratio of 1 : 1 for her maxillary central incisors (see Fig. 12-7, C). She revealed excessive gingival tissues relative to the display of her anterior teeth. To achieve a more esthetic appearance, it was determined that a width-to-length ratio of 0.80 would be desirable. After a periodontal surgical crown-lengthening procedure, a more esthetic width-to-length ratio of 0.80 was attained (see Fig. 12-7, D). After placement of eight etched porcelain veneers for the treatment of fluorosis discoloration, the same 0.80 width-to-length ratio can be seen (see Fig. 12-7, E). A 7-year postoperative photograph reveals the long-term esthetic result (see Fig. 12-7, F).
Position and Alignment
Minor rotations can be corrected by reducing the enamel in the area of prominence and augmenting the deficient area with composite resin (Fig. 12-8, A and B). Care must be taken to restrict all recontouring of prominent areas to enamel. If the rotation is to be treated with an indirectly fabricated composite or porcelain veneer, an intra-enamel preparation is recommended, with greater reduction provided in the area of prominence. This preparation allows subsequent restoration to appropriate physiologic contours.
Malposed teeth are treated in a similar manner. Teeth in mild linguoversion can be treated by augmentation with full facial veneers placed directly with composite or made indirectly from processed composite or porcelain (see Fig. 12-8, C and D). Care must be exercised in maintaining physiologic gingival contours that do not impinge on tissue or result in an emergence profile of the restoration that is detrimental to gingival health. A functional incisal edge should be maintained by appropriate contouring of the restoration (an excessively thick incisal edge should be avoided). If the occlusion allows, limited reduction of enamel on the lingual aspect can be accomplished to reduce the faciolingual dimension of the incisal portion of the tooth. Lingual areas participating in protrusive functional contact should not be altered, however. Individual teeth that are significantly displaced facially (i.e., facioversion) are best treated orthodontically.
Color
Problems in color perception also complicate selection of the appropriate shade of restorative material. Various light sources produce different perceptions of color. This phenomenon is referred to as metamerism.9 The color of the surrounding environment influences what is seen in the patient’s mouth. Color perception also is influenced by the physiologic limitations of the dentist’s eye. On extended viewing of a particular tooth site, eyes experience color fatigue, resulting in a loss of sensitivity to yellow-orange shades.7 By looking away at a blue object or background (i.e., the complementary color), the dentist’s eyes quickly recover and are able to distinguish subtle variations in yellow-orange hues again. Because of the many indirect factors that influence color perception, it is recommended that the dentist, the assistant, and especially the patient all be involved in shade selection.
Translucency
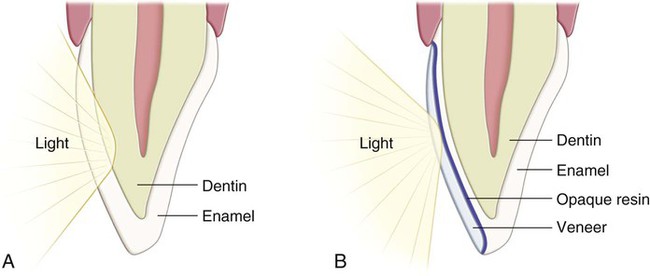
Translucency is another factor that affects the esthetic quality of the restoration. The degree of translucency is related to how deeply light penetrates into the tooth or restoration before it is reflected outward. Normally, light penetrates through enamel into dentin before being reflected outward (Fig. 12-9, A); this affords the realistic esthetic vitality characteristic of normal, unrestored teeth. Shallow penetration of light often results in loss of esthetic vitality. This phenomenon is a common problem encountered when treating severely intrinsically stained teeth such as teeth affected by tetracycline with direct or indirect veneers. Although opaque resin media can mask the underlying stain, esthetic vitality is usually lost because of reduced light penetration (see Fig. 12-9, B). Indirect veneers of processed composite or porcelain fabricated to include inherent opacity also may have this problem.
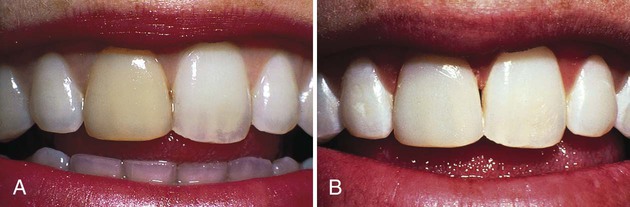
Illusions of translucency also can be created to enhance the realism of a restoration. Color modifiers (also referred to as tints) can be used to achieve apparent translucency and tone down bright stains or to characterize a restoration. Figure 12-10 shows a case in which the maxillary right central incisor with intrinsic yellow staining caused by trauma to the tooth warranted restoration. When bleaching treatments were unsuccessful because of calcific metamorphosis, a direct composite veneer was used in this patient. After an intra-enamel preparation and acid-etching, a violet color modifier (the complementary color of yellow) was applied to the prepared facial surface to reduce the brightness and intensity of the underlying yellow tooth. Additionally, a mixture of gray and violet color modifiers was used to simulate vertical areas of translucency. The final restoration is shown in Figure 12-10, B. Color modifiers also can be incorporated in the restoration to simulate maverick colors, to check lines, or to surface spots for further characterization. Color modifiers always should be placed within a composite restoration, not on its surface.
Clinical Considerations
Although an understanding of basic artistic elements is imperative to successfully placing esthetic restorations, certain clinical considerations must be addressed concomitantly to ensure the overall quality of the restoration. In addition to being esthetic, restorations must be functional. Dawson stated, “Esthetics and function go hand in hand. The better the esthetics, the better the function is likely to be and vice versa.”10
Conservative Alterations of Tooth Contours and Contacts
Alterations of Shape of Natural Teeth
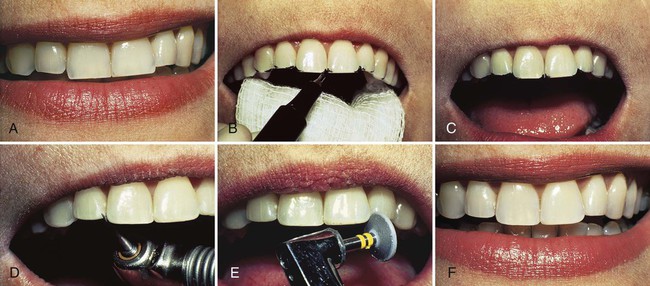
Some esthetic problems can be corrected conservatively without the need for tooth preparation and restoration. Consideration always should be given to reshaping and polishing natural teeth to improve their appearance and function (Fig. 12-11). In addition, the rounding of sharp angles can be considered a prophylactic measure to reduce stress and to prevent chipping and fractures of the incisal edges.
Etiology
Attrition of the incisal edges often results in closed incisal embrasures and angular incisal edges (see Fig. 12-11, A). Anterior teeth, especially maxillary central incisors, often are fractured in accidents. Other esthetic problems, including attrition and abnormal wear from poor dental habits (e.g., biting fingernails, holding objects with teeth), often can be corrected or the appearance improved by reshaping natural teeth.
Treatment
The patient must understand what is involved and must want to have the alteration made. If reshaping is desired, it is helpful to mark, by using a pencil or alcohol-marking pen, an outline of the areas of the teeth to be reshaped (see Fig. 12-11, B). By marking the anticipated areas for enamel reshaping, the patient is provided some indication of what the post-operative result may look like (see Fig. 12-11, C). If available, esthetic computer imaging also can be used to illustrate the possible result before treatment.
Because all reshaping is restricted to enamel, anesthesia is not required. A cotton roll is recommended for isolation. Diamond instruments and abrasive disks and points are used for contouring, finishing, and polishing (see Fig. 12-11, D and E). Through careful reshaping of appropriate enamel surfaces, a more esthetic smile (characterized by youthful features) is attained. Rounded incisal edges also are less likely to chip or fracture (see Fig. 12-11, F).
A second example involves the irregular, fractured incisal surfaces of maxillary central incisors (Fig. 12-12, A). An esthetic result can be accomplished by slightly shortening the incisal edges and reshaping both teeth to a symmetrical form. Photographs, line drawings, esthetic imaging, or marking the outline on the patient’s teeth enables the patient to envision the potential improvement before any changes are made. Protrusive function always should be evaluated to prevent inadvertent elimination of this occlusal contact. Conservative treatment consists of using diamond instruments and abrasive disks and points for contouring and polishing the central incisors. The finished result is illustrated in Figure 12-12, B.
As some patients grow older or have the habit of bruxism, the incisal surfaces often wear away, leaving sharp edges that chip easily. This is also accompanied by loss of the incisal embrasures (Fig. 12-13, A). To lessen the chance of more fractures and to create a more youthful smile, the incisal embrasures are opened, and the incisal angles of teeth are rounded (see Fig. 12-13, B).
Alterations of Embrasures
Etiology
Anterior teeth can have embrasures that are too open as a result of the shape or position of teeth in the arch. When the permanent lateral incisors are congenitally missing, canines and posterior teeth may drift mesially, or the space may be closed orthodontically. The facial surface and cusp angle of some canines can be reshaped to appear like lateral incisors. In many instances, the mesio-incisal embrasures remain too open (Fig. 12-14, A).
Treatment
A polyester strip is inserted to protect the adjacent tooth during acid etching. After etching, rinsing, and drying, the contoured strip is positioned. A light-cured composite material is inserted, and the strip is closed during polymerization. The incisal embrasures of both canines are corrected, and both restorations are finished by routine procedures (see Fig. 12-14, B). The occlusion should be evaluated to assess centric contacts and functional movements, and any adjustments or corrections should be made, if indicated.
Correction of Diastemas
Etiology
The presence of diastemas between anterior teeth is an esthetic problem for some patients (Fig. 12-15). Before treatment, a diagnosis of the cause is made, including an evaluation of the occlusion. Probably the most frequent site of a diastema is between maxillary central incisors. A prominent labial frenum with non-elastic fibers extending proximally often prevents the normal approximation of erupting central incisors.11 Other causative factors include congenitally missing teeth, undersized or malformed teeth, interarch tooth size discrepancies (i.e., Bolton discrepancy), supernumerary teeth, and heredity. Diastemas also may result from other problems such as tongue thrusting, periodontal disease, or posterior bite collapse. Diastemas should not be closed without first recognizing and treating the underlying cause, as merely treating the cause may correct the diastema.
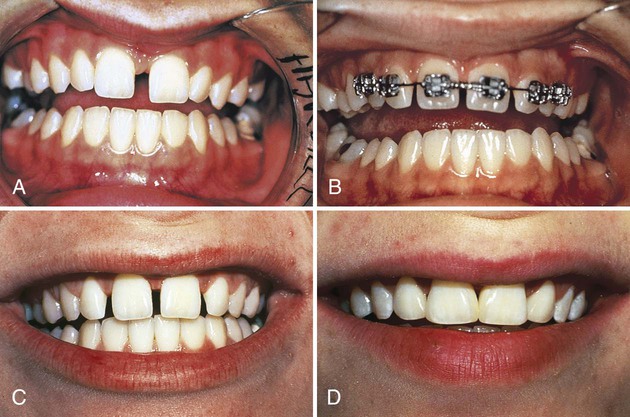
Treatment
Traditionally, diastemas have been treated by surgical, periodontal, orthodontic, and prosthetic procedures. These types of corrections can be impractical or unaffordable and often do not result in permanent closure of the diastema. In carefully selected cases, a more practical alternative is use of the acid-etch technique and composite augmentation of proximal surfaces (see Figs. 12-5 and Fig. 12-6). All treatment options (including no treatment) should be considered before resorting immediately to composite augmentation. Line drawings, photographs, computer imaging, models with spaces filled, and direct temporary additions of ivory-colored wax or composite material on natural teeth (unetched) are important preliminary procedures.
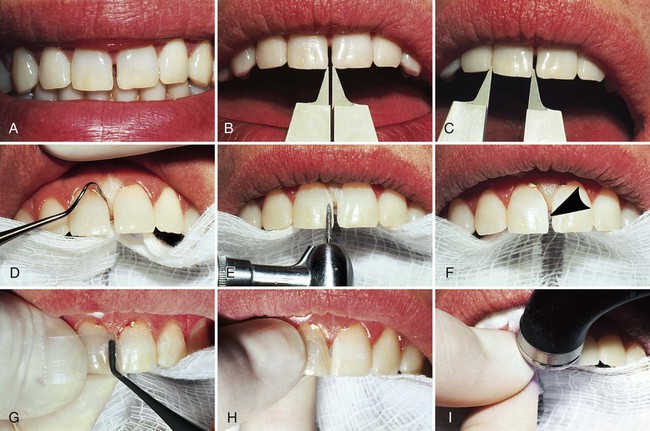
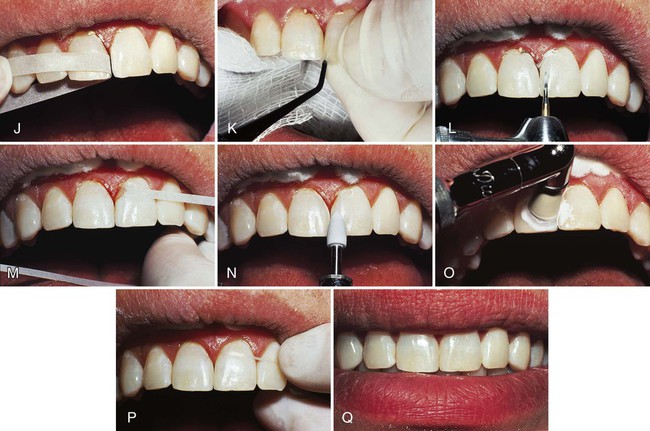
The correction of a diastema between maxillary central incisors is described and illustrated in Figure 12-15. After the teeth are cleaned and the shade selected, a Boley gauge or other suitable caliper is used to measure the width of the diastema and the individual teeth (see Fig. 12-15, B and C). Occasionally, one central incisor is wider, requiring a greater addition to the narrower tooth. Assuming the incisors are of equal width, symmetrical additions can be ensured by using half of the total measurement of the diastema to gauge the width of the first tooth restored. Cotton rolls, instead of a rubber dam, are recommended for isolation because of the importance of relating the contour of the restoration directly to the proximal tissue. Usually, the restoration must begin slightly below the gingival crest to appear natural and to be confluent with the tooth contours.
With cotton rolls in place, a gingival retraction cord of an appropriate size is tucked in the gingival crevice of each tooth from midfacial mesially to midlingual (see Fig. 12-15, D). The cord retracts the soft tissue and prevents seepage from the crevice. In some instances, the retraction cord may need to be inserted for one tooth at a time to prevent strangulation of interproximal tissue during preparation and restorative procedures. To enhance retention of the composite, a coarse, flame-shaped diamond instrument is used to roughen the proximal surfaces, extending from the facial line angle to the lingual line angle (see Fig. 12-15, E). More extension may be needed to correct the facial or lingual contours, depending on the anatomy and position of the individual tooth. The enamel is acid-etched approximately 0.5 mm past the prepared, roughened surface. The acid should be applied gingivally only to the extent of the anticipated restoration. After rinsing and drying, the etched enamel should display a lightly frosted appearance (see Fig. 12-15, F). A 2 × 2 inch (5 × 5 cm) gauze is draped across the mouth and tongue to prevent inadvertent contamination of the etched preparations by the patient. After both preparations are completed, the teeth are restored one at a time.
A polyester strip is contoured and placed proximally, with the gingival aspect of the strip extending below the gingival crest. Additional contouring may be required to produce enough convexity in the strip. In most cases, a wedge cannot be used. The strip is held (with the index finger) on the lingual aspect of the tooth to be restored, while the facial end is reflected for access. A light-cured composite is used for the restoration. After the bonding agent is applied, the composite material is inserted with a hand instrument (see Fig. 12-15, G). Careful attention is given to pressing the material lingually to ensure confluence with the lingual surface. The matrix is gently closed facially, beginning with the gingival aspect (see Fig. 12-15, H). Care must be taken not to pull the strip too tightly because the resulting restoration may be under-contoured faciolingually, mesiodistally, or both. The light-cured composite material is polymerized with the light directed from the facial and lingual directions for an appropriate amount of time. Note that curing times may vary according to the type of light source, the composite used, and the thickness of the material (see Fig. 12-15, I). Initially, it is better to over-contour the first restoration slightly to facilitate finishing it to an ideal contour.
When polymerization is complete, the strip is removed. Contouring and finishing are achieved with appropriate carbide finishing burs, fine diamonds, or abrasive disks (see Fig. 12-15, L). Finishing strips are invaluable for finalizing the proximal contours (see Fig. 12-15, J and M). Final polishing is deferred until the contralateral restoration is completed. It is imperative for good gingival health that the cervical aspect of the composite addition be immaculately smooth and continuous with the tooth structure. Overhangs must not be present. Removal of the gingival retraction cord facilitates inspection and smoothing of this area. Flossing with a length of unwaxed floss verifies that the gingival margin is correct and smooth if no fraying of the floss occurs (see Fig. 12-15, P). It is important that the correct mesiodistal dimension of the first tooth be established before the second tooth is restored.
After etching, rinsing, and drying, the second restoration is completed. A tight proximal contact can be attained by displacing the second tooth being restored in a distal direction (with the thumb and the index finger) while holding the matrix in contact with the adjacent restoration (see Fig. 12-15, K). Contouring is accomplished with a 12-fluted carbide bur and finishing strips (see Fig. 12-15, L and M). Articulating paper should be used to evaluate the patient’s occlusion to ensure that the restorations are not offensive in centric or functional movements; adjustments can be made with a carbide finishing bur or abrasive disks. Final polishing is achieved with rubber polishing points or polishing paste applied with a Prophy cup in a low-speed handpiece (see Fig. 12-15, N and O). Unwaxed floss is used to detect any excess material or overhang (see Fig. 12-15, P). The final esthetic result is seen in Figure 12-15, Q.
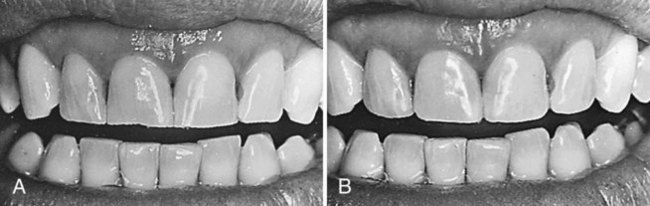
Multiple diastemas among the maxillary anterior teeth are shown in Figure 12-16, A. Closing the spaces by orthodontic movement was considered in this patient; however, because the patient’s teeth were under-contoured mesiodistally, the diastemas were closed by etching the teeth and bonding composite to the proximal surfaces. The teeth after treatment are shown in Figure 12-16, B. In the presence of defective Class III restorations or proximal caries, it is recommended that the teeth be restored with the same composite used for closing the diastema. Often, these restorations can be performed at the same time the diastema is closed with composite additions (Fig. 12-17).
Occasionally, diastemas are simply too large to close esthetically with composite augmentation alone (Fig. 12-18, A). Closing a large space of this magnitude with composite would merely create an alternative esthetic problem, that is, excessively large central incisors, which would further exacerbate the existing discrepancy in proportionality among anterior teeth. In such cases, large spaces are best redistributed orthodontically among anterior teeth so that symmetric and equal composite additions can be made to the central and lateral incisors (see Fig. 12-18, B and C). This approach that involves space distribution results in improved proportionality among anterior teeth (see the earlier section on Artistic Elements). The final result, immediately after completion, is shown in Figure 12-18, D.
Conservative Treatments for Discolored Teeth
Extrinsic Discolorations
Etiology
Stains on the external surfaces of teeth (referred to as extrinsic discolorations) are common and may be the result of numerous factors. In young patients, stains of almost any color can be found and are usually more prominent in the cervical areas of teeth (Fig. 12-19, A). These stains may be related to remnants of Nasmyth’s membrane, poor oral hygiene, existing restorations, gingival bleeding, plaque accumulation, eating habits, or the presence of chromogenic microorganisms.12 In older patients, stains on the surfaces of teeth are more likely to be brown, black, or gray and occur on areas adjacent to gingival tissue. Poor oral hygiene is a contributing factor, but coffee, tea, and other types of chromogenic foods or medications can produce stains (even on plaque-free surfaces). Tobacco stains also are observed frequently. Existing restorations may be discolored for the same reasons.
An example of one of the most interesting and unusual types of external staining is illustrated in Figure 12-19, B. In Southeast Asia, some women traditionally dye their teeth with betel nut juice to match their hair and eyes as a sign of beauty.13 Slices of lemon are held in contact with the teeth before applying the betel nut juice to make the staining process more effective. This example was probably one of the first applications of the acid-etch technique. A weak acid, such as that found in citrus fruits, is known to cause rapid decalcification of enamel.
Treatment
Most surface stains can be removed by routine prophylactic procedures (Fig. 12-20). Some superficial discolorations on tooth-colored restorations and decalcified areas on teeth, however, cannot be corrected by such cleaning. Conservative correction may be accomplished by mild microabrasion or by surfacing the thin, outer, discolored layer with a flame-shaped, carbide finishing bur or diamond instrument (i.e., macroabrasion), followed by polishing with abrasive disks or points to obtain an acceptable result. (See subsequent sections on Microabrasion and Macroabrasion for details of clinical technique.)
Intrinsic Discolorations
Etiology
Intrinsic discolorations are caused by deeper (not superficial) internal stains or enamel defects; these stains are more complex to treat than are external types. Teeth with vital or non-vital pulps as well as root canal–treated teeth can be affected. Vital teeth may be discolored at the time the crowns are forming, and the abnormal condition usually involves several teeth. Causative factors include hereditary disorders, medications (particularly tetracycline preparations), excess fluoride, high fevers associated with early childhood illnesses, and other types of trauma.12 The staining may be located in enamel or dentin. Discolorations restricted to dentin still may show through enamel. Discoloration also may be localized or generalized, involving the entire tooth.
Various preparations of the antibiotic drug tetracycline can cause the most distracting, generalized type of intrinsic discoloration (Fig. 12-21, A).14 The severity of the staining depends on the dose, the duration of exposure to the drug, and the type of tetracycline analogue used. Different types of tetracyclines induce different types of discoloration, varying from yellow-orange to dark blue-gray. Dark blue-gray, tetracycline-stained teeth are considerably more difficult to treat than are teeth with mild yellow-orange discolorations. Staining from tetracycline-type drugs most frequently occurs at an early age and is caused by ingestion of the drug concomitant with the development of permanent teeth. Studies indicate that permanent teeth in adults also can experience a graying discoloration, however, as a result of long-term exposure to minocycline, a tetracycline analogue.14
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses