11
Patients at risk
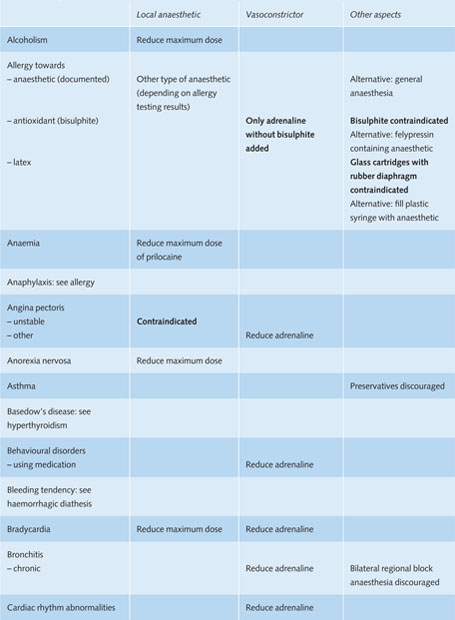
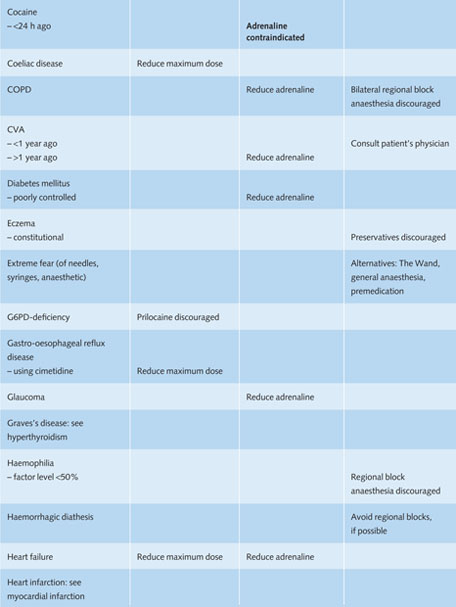
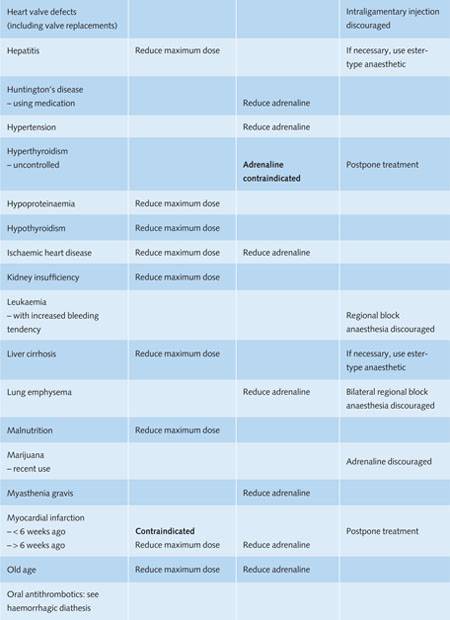
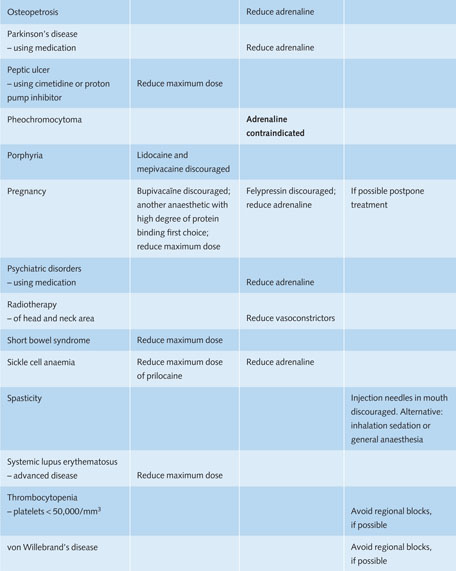
Dentists are increasingly confronted with medically compromised patients. In this chapter, systemic diseases will be discussed that are associated with a (theoretically) increased risk of side effects during the administration of local anaesthetics (Table 11.1).
11.1 Introduction
For the prevention of side effects of local anaesthesia it is important to identify patients with increased risk before administration. By taking a structured medical history, preferably written, the dentist usually can retrieve relevant information about the general health of the patient. It will also identify any medication that could interfere with the local anaesthetic.
When the patient reports a disease or condition that may interact with the administration of local anaesthetics, consultation with the patient’s physician is advisable and sometimes necessary. To obtain this medical information from a general physician or medical specialist, explicit permission of the patient is required, preferably in written form.
11.2 Cardiovascular disease
Local anaesthetics reduce the contraction strength of the heart. Therefore, one has to consider the risk that latent heart failure may manifest itself during the administration of a local anaesthetic. In addition, liver perfusion is reduced in heart failure, which increases the half-life of amide-type anaesthetics and the risk of overdose. Since the transmission of action potentials in the heart is delayed under the influence of local anaesthetics, one also should consider – at least theoretically – the development of an atrioventricular block, which results in an abnormally slow heart rhythm accompanied by dizziness or loss of consciousness.
An increased adrenaline concentration in the blood results in an increased workload of the heart. In patients with ischaemic heart disease this will increase the oxygen deficit of the heart muscle, which may provoke an attack of angina pectoris or even a myocardial infarction. It is recommended that dental treatment, when necessary, is performed at least 6 weeks after a myocardial infarction. Furthermore, epinephrine can lead to heart rhythm disturbances.
Table 11.1 Recommendations for the use of local anaesthetics in medically compromised patients in general dental practice.
Reduce maximum dose = during one treatment session no more than 25–50% of the maximum recommended dose of the anaesthetic should be used.
Reduce adrenaline = during one treatment session the total amount of adrenaline should be restricted to a maximum of 0.04 mg for adults (= 4 ml adrenaline 1:100,000 or 8 ml adrenaline 1:200,000).
Because pain during dental treatment induces a substantial increase in the release of adrenaline from the renal medulla, adequate anaesthesia is essential in patients with ischaemic heart diseases. According to the American Heart Association, use of adrenaline as vasoconstrictor is justified in a dilution of 1:100,000 or 1:200,000 and the total amount of adrenaline should be restricted to 0.04 mg for adults (= 4 ml anaesthetic solution with adrenaline 1:100,000 or 8 ml with 1:200,000), though this also depends on the weight of the patient. Of course, one should always aspire to minimise the risk of intravascular injection of adrenaline. A possible alternative for adrenaline is the use of prilocaine with the vasoconstrictor felypressin, which has no or only limited cardiac effects.
Patients with structural heart defects and/or prosthetic heart valves have an increased risk of developing infective endocarditis, an infection of the endothelium that covers the inside surface of the heart and the heart valves. Since most injections in the oral cavity do not induce a substantial bacteraemia, prophylactic use of an antibiotic is in general not necessary. However, endocarditis prophylaxis may be indicated for the subsequent dental procedure.
Intraligamentary anaesthesia may introduce considerable numbers of bacteria into the bloodstream. This injection technique should be avoided in patients at risk of infective endocarditis, unless antibiotic prophylaxis is already indicated for following invasive dental procedures.
11.3 Hypertension
The stress associated with the administration of a local anaesthetic induces an increase in blood pressure, both in healthy individuals and in patients with hypertension. Therefore, the severity of the hypertension must be determined before the administration of a local anaesthetic. One can ask the hypertensive patient whether his or her blood pressure has been measured recently and, if so, which values were determined at that moment. Dentists can also measure the patient’s blood pressure themselves.
Patients with a systolic blood pressure exceeding 200 mmHg and/or a diastolic value over 115 mmHg should only receive dental treatment when their blood pressure has been medically treated. When the hypertensive patient has a systolic blood pressure between 160 and 200 mmHg or a diastolic pressure between 105 and 115 mmHg and the patient is currently under medical treatment, most dental treatment can be performed. Fear of the injection may induce a further increase in blood pressure. It is important to create an open atmosphere, where the patient feels free to discuss possible concerns about the intended injection and the dentist takes these into consideration.
Pain during dental treatment will also lead in hypertensive patients to a substantial release of adrenaline from the adrenal medulla, with a considerable increase in blood pressure. On the other hand, the use of lar/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


