CHAPTER 11
Osteomyelitis
Matthew W. Hearn,1 Christopher T. Vogel,2 Robert M. Laughlin,3 and Christopher J. Haggerty4
1Private Practice, Valparaiso, Indiana, USA
2Department of Oral and Maxillofacial Surgery, University of Missouri–Kansas City, Kansas City, Missouri, USA
3Department of Oral and Maxillofacial Surgery, Naval Medical Center San Diego, San Diego, California, USA
4Private Practice, Lakewood Oral and Maxillofacial Surgery Specialists, Lees Summit; and Department of Oral and Maxillofacial Surgery, University of Missouri-Kansas City, Kansas City, Missouri, USA
Osteomyelitis: Inflammation of the osseous medulla.
General Principles of Management of Osteomyelitis (Acute and Chronic)
- A definitive diagnosis of osteomyelitis can only be made via bone biopsy with histopathological examination and staining, and microbiologic culture (including actinomyces and nocardia) and sensitivities.
- All forms of osteomyelitis are managed with a combination of removal of the source of the infection, bone removal or resection to healthy, bleeding bone margins, reestablishment of blood flow to the involved area, and antibiotic therapy.
- All potential sources of infection are eradicated. Decayed and mobile teeth within the involved area should be extracted, all fixation plates and screws should be removed, and intraoral and cutaneous fistulae are resected.
- All necrotic and involved bone must be completely removed to expose healthy bleeding bone. Bone that does not freely bleed from its marrow cavity is avascular bone, will interfere with antibiotic penetration of the involved area, will serve as a nidus for future infections, and will prevent adequate blood flow to the involved area. The removal of involved bone will frequently lead to continuity defects.
- Initial antibiotic coverage includes broad-spectrum antibiotics with both aerobic and anaerobic coverage.
- Bone biopsy culture and sensitivities will ultimately guide antibiotic selection.
- Cases that do not respond to initial surgical debridement and antibiotic therapy require more aggressive surgical intervention, the extraction of adjacent teeth, infectious disease consultation, and peripherally inserted central catheter (PICC) line placement for long-term intravenous antibiotic management.
- Due to the inflammatory nature of osteomyelitis, anti-inflammatory medications such as nonsteroidal anti-inflammatory drugs and corticosteroids are beneficial in the management of symptoms both before and after surgical intervention.
- Acute osteomyelitis: Clinical symptoms present for less than 4 weeks. Radiographic findings are typically absent.
- Chronic osteomyelitis: Clinical symptoms present for 4 weeks or longer. Commonly has radiographic findings. Subclassifications include suppurative and nonsuppurative forms.
- Clinical symptoms of osteomyelitis: Pain, edema, mobile teeth, suppuration, induration, paresthesia or anesthesia, tissue erythema, and exposed bone (Figure 11.1). Acute osteomyelitis frequently presents as a facial abscess with symptoms specific to the space involved (i.e., trismus).
- Radiographic findings of osteomyelitis: Altered areas of bone density, including areas of osteosclerosis, osteolysis, periosteal reaction (periostitis ossificans), sequestrum, and cortical and trabecular defects (see Figures 11.2, 11.3, 11.4, and 11.5).
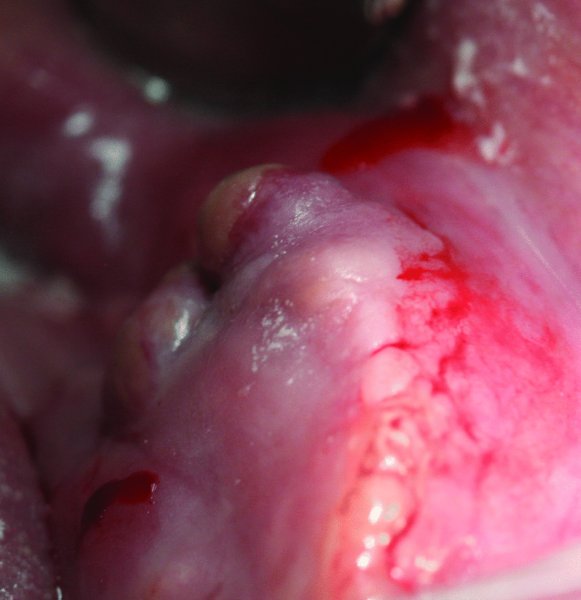
Figure 11.1. Suppurative osteomyelitis of the anterior mandible. Note fistula formation, edema, and overlying tissue erythema.
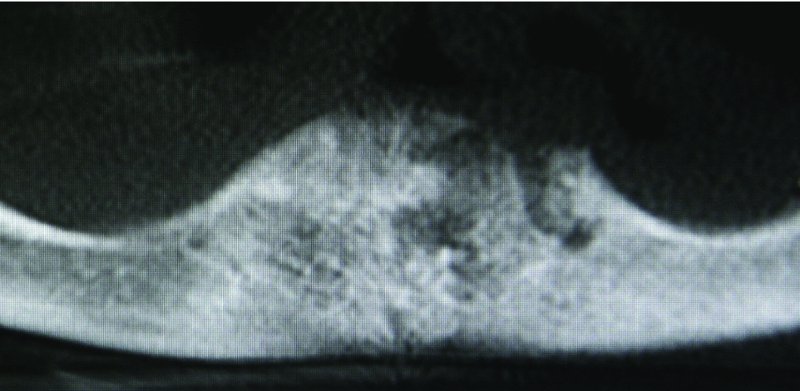
Figure 11.2. Cone beam computed tomography scan of the patient in Figure 11.1. Radiograph demonstrates areas of osteolysis and trabecular defects within the anterior mandible.
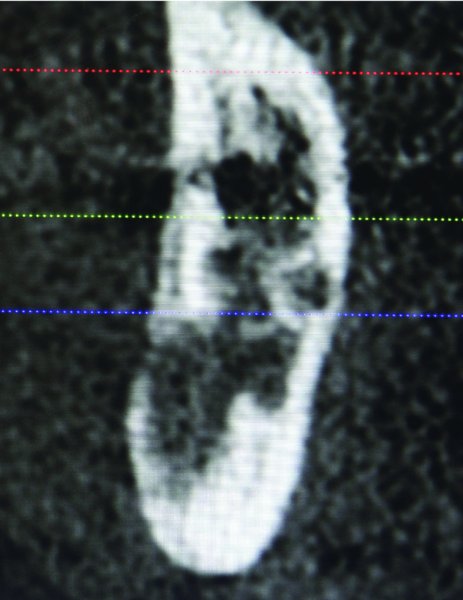
Figure 11.3. Coronal cone beam computed tomography scan demonstrating alternating areas of osteosclerosis and osteolysis of the posterior mandible.

Figure 11.4. Orthopantomogram of the left posterior mandible demonstrating areas of cortical defects and osteolysis extending to the inferior border.
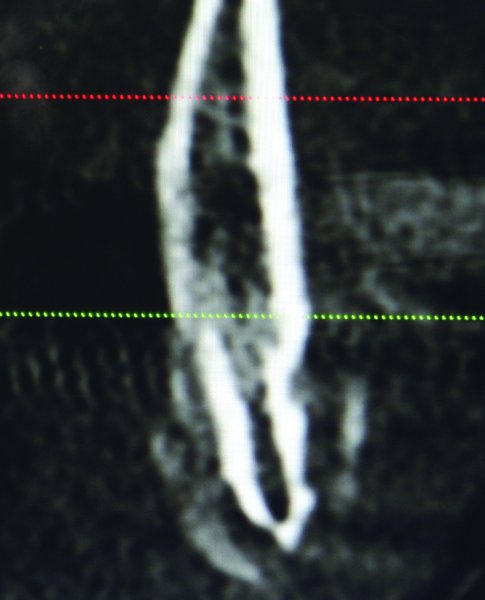
Figure 11.5. Coronal cone beam computed tomography scan of the patient in Figure 11.4 demonstrating a periosteal reaction associated with osteomyelitis of the posterior mandible.
Surgical Treatment Options for Osteomyelitis
Saucerization
Saucerization involves the removal of involved bone to expose the medullary cavity and the smoothing of surrounding bone.
Saucerization Technique
- This procedure may be performed under local or general anesthesia.
- Mobile teeth and loose segments of bone are removed.
- The exposed or involved bone is removed with a combination of a ronguer and a rou/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


