Management of acute emergencies and traumatic dental injuries
Principles of management of pain
Successful management of pain is:
1. preceded by sharp diagnostic and psychological insight complemented by a confident manner
2. accompanied by effective and efficient treatment execution, including adequate anaesthesia and analgesia
3. succeeded (hopefully) by patient gratitude and loyalty; and a personally enhanced reputation for the dentist.
The majority of patients attending the dentist in pain suffer from the acute consequences of pulpal or periradicular disease (Table 10.1), but the dentist must beware of confounding factors.
Table 10.1
Prevalence of acute orofacial or dental pain
| Population | Prevalence of acute orofacial or dental pain | Comments |
| USA (National Health Interview Survey, 1989) | 14% (acute orofacial pain in the past 6 months) | Most common causes: caries & periodontal disease |
| UK (Adult Dental Health Survey, 2009) | 26% (dental pain) | Most cases were associated with gross caries & sepsis |
| Toronto, Canada (Locker & Grushka, 1987) | 29% (teeth with cold/hot); 14% (toothache) in the past 4 weeks | 50% of cases reported severe symptoms |
| Sao Paulo, Brazil (age 12, 15 adolescents) (2010) | 26% (dental pain) | Most cases were associated with untreated caries or endodontic treatment need |
| Hong Kong, China (1222 18+ Chinese speaking people in 2006) | 28% (tooth sensitivity); 13% (toothache) |
Diagnostic accuracy
Patients presenting in a dental practice suffering from orofacial pain must be viewed from a broad diagnostic perspective. The cognitive and material tools possessed by dentists naturally sway their management towards dental intervention but non-dental factors can mimic dental pain too. This is due in part to convergence of peripheral neural pathways in the central nervous system and in part to the patients’ inability to articulate their experience in a meaningful way to the dentist. Dentists should therefore be aware of the common causes of misdiagnosis. These include non-odontogenic inflammation, vascular, musculoskeletal, neurological, and systemic or psychogenic problems (see Chapter 16). Temporomandibular joint (TMJ) and muscular pain from the masseter, lateral pterygoid and temporalis muscles may refer pain to the maxillary or mandibular molars, premolars or even anterior teeth on occasion. Such a condition may be more appropriately managed with reassurance, explanation, reduction in muscle and joint load, stretching exercises, heat/cold therapy and lastly, the use of an occlusal acrylic splint may help (Figs 10.1, 10.2).
Effective intraoperative pain control
Local analgesic agents and their actions
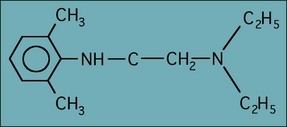
The most commonly used analgesic solution for most endodontic procedures is lignocaine with adrenaline (epinephrine) (Fig. 10.3). Providing the analgesic solution is given slowly with an aspirating technique, then the adrenaline (epinephrine) is not a problem in most patients.
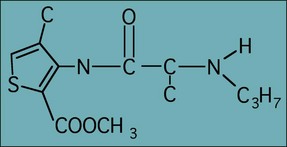
Articaine with adrenaline (epinephrine) (Fig. 10.4) has gained favour as a local analgesic solution to use where lignocaine appears to have failed. Articaine differs from lignocaine as it has a thiophene ring as its lipophilic component rather than a substituted aromatic ring. Studies show that it is no more effective as an analgesic agent than lignocaine. However, it does have an increased propensity to diffuse widely, which may allow it to block accessory innervations over a broader field. In addition, the different stereochemical structure may also account for its apparently higher success rate. Unfortunately, it is also associated with a higher frequency of persistent paraesthesia.
The use of long-acting anaesthetics may provide the patient pain relief while the postoperative analgesics start to act. Marcaine (0.5% bupivacaine with 1 : 200 000 epinephrine) when used as a regional block can give soft-tissue anaesthesia of 6–8 hours. Marcaine is not available in all countries in dental anaesthetic cartridges and, in some areas, is not licensed for dental use. Dental practitioners should satisfy themselves as to the local rules before administering it. Other preparations of bupivacaine are available, such as carbostesin (Fig. 10.5).
Local analgesic agent delivery
Gow–Gates technique
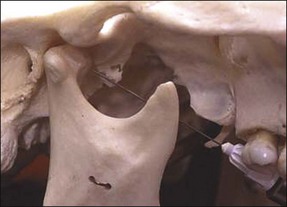
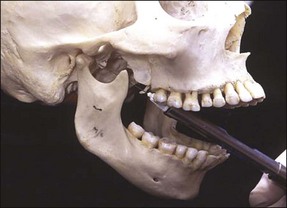
This is a true mandibular block injection that provides analgesia of all the sensory divisions of the mandibular nerve, including buccal, inferior alveolar, lingual and mylohyoid. The method relies upon the deposition of analgesic solution adjacent to the head of the mandibular condyle (Fig. 10.6). The patient has the mouth wide open and a line is imagined from the corner of the mouth to the intertragic notch; this is the plane of approach. The needle is introduced from the direction of the contralateral mandibular canine tooth and directed over the ipsilateral maxillary second molar (Fig. 10.7). The point of mucosal penetration is higher than for a conventional inferior dental block. The needle is advanced until bony contact is made with the head of the condyle, withdrawn slightly, aspiration performed, and a full cartridge of analgesic is delivered.
Akinosi technique
This is a simpler technique than the Gow–Gates method and is sometimes known as the closed-mouth technique. The patient has the mouth closed and a 35 mm needle is used. The syringe is advanced parallel to the maxillary occlusal plane at the level of the maxillary mucogingival junction. The needle is advanced until the hub is level with the distal surface of the maxillary second molar (Fig. 10.8). At this point, a cartridge of analgesic solution is deposited. This technique does not rely on touching bone and this can be a disadvantage. However, the Akinosi technique allows provision of analgesia in a situation where all other methods of giving an inferior dental block would fail. Both motor and sensory analgesia are achieved allowing the patient to open the mouth.
Intraligamental injections
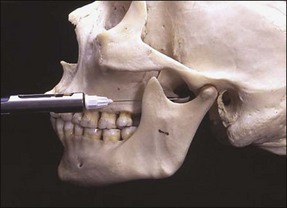
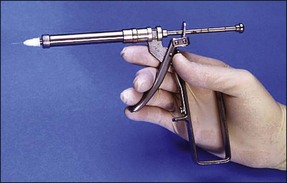
Intraligamental injections are used to deposit analgesic directly into the periodontal ligament space and a number of specialized syringes (Fig. 10.9) and small needles have been developed to facilitate this. The needle is inserted into the mesial gingival sulcus and in contact with the tooth (Fig. 10.10). The needle is supported by fingers and positioned with maximal penetration between the root and crestal alveolar bone. Pressure is slowly applied to the syringe handle for 20–30 seconds. Backpressure has to be developed for this technique to work and blanching of the soft tissues would be a sign of probable success. If analgesic solution flows readily out of the sulcus then analgesia will not be achieved. Pressure is necessary to force the solution into the marrow spaces to contact and block the dental nerves. The technique should be repeated on the distal and lingual surfaces of the involved tooth.
Intraosseous technique
The intraosseous technique allows analgesic solution to be deposited directly into the cancellous bone around the apices of the tooth. It has a rapid onset and has shown extremely favourable results when used as a supplemental analgesic for the “hot” mandibular molar. The mucosa overlying the injection site, either just mesial or distal of the tooth to be treated, is anaesthetized with a small infiltration. Special kits have been developed that facilitate drilling a small hole through the mucosa and cortical plate to allow injection of the anaesthetic solution into the cancellous bone. X-Tips (Prestige Dental, Bradford, UK) consist of a drill to perforate the cortical plate combined with a guide sleeve. When the drill is withdrawn the guide sleeve is left in situ. The analgesic solution can be injected through the guide sleeve, which is designed to accept an ultra-short 27-gauge needle (Fig. 10.11). The guide sleeve can be left in place during the procedure so that the anaesthetic can be “topped-up” if required (Fig. 10.12). A small number of patients develop soreness at the injection site and a transitory increased heart rate can occur depending on the analgesic solution used.
Management of the “hot” pulp
Supplemental analgesia is often required when treating the “hot” pulp to account for accessory nerve supply infiltrations; while not a replacement for inferior dental blocks, it may be required to block input from the cervical plexus, together with the mylohyoid and lingual nerves. Cross-innervation from the contralateral inferior alveolar nerve should also be considered. In the maxillary arch, the posterior superior alveolar block to the maxillary molars can be considered while anterior superior alveolar nerve block can deposit analgesic at the opening of the infraorbital foramen – decussation of the fibres of the anterior superior dental nerve can provide innervation to the premolar teeth. When treating vital molar teeth, palatal infiltrations to block innervation from the greater palatine or nasopalatine nerve should be considered mandatory.
Effective postoperative pain control
The relative efficacy of different analgesics is provided by the Oxford league table (Table 10.2). Aspirin is widely used. However, its efficacy is dose related, 1000–1200 mg four times per day providing greater analgesia than 500–600 mg four times per day. Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, can also be used. Ibuprofen has been shown to be one of the most effective analgesics at reducing acute pain and its efficacy is also dose related; 400 mg four times per day appears to be the optimal dose but up to 800 mg delivers 100% efficacy, if there are no side effects. Paracetamol is often used by patients with sensitivity to aspirin and the other NSAIDs and can be efficacious in high dosage, but it does not have the same anti-inflammatory properties.
Table 10.2
The 2007 Oxford league table of analgesic efficacy
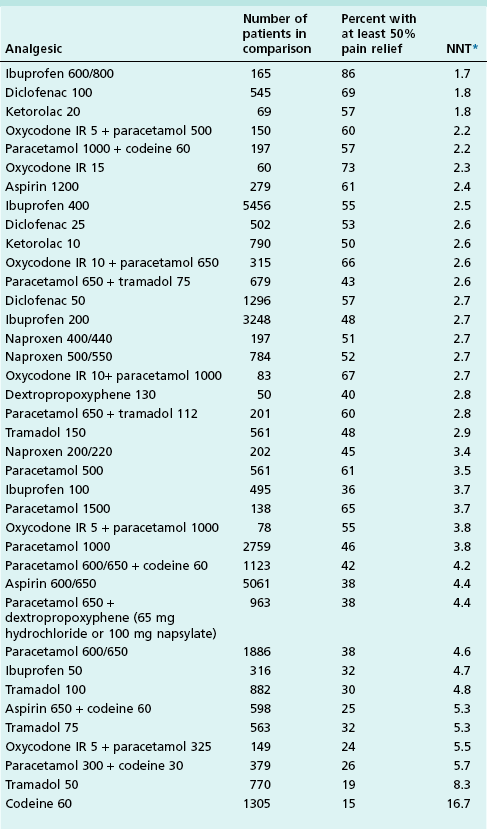
(www.jr2.ox.ac.uk/bandolier/booth/painpag/)
*Numbers needed to treat (NNT) are calculated for the proportion of patients with at least 50% pain relief over 4–6 hours compared with placebo in randomized, double-blind, single-dose studies in patients with moderate to severe pain. Drugs were oral, unless specified, and doses are milligrams.
Contraindications for aspirin include ulcers, asthma, diabetes, gout, influenza (Reye’s syndrome) and liver dysfunction. It is well to remember the possibility of drug interactions of NSAID-like drugs, which include: reduction of anti-high blood pressure effectiveness with ACE inhibitors, beta blockers, thiazide and loop diuretics; increased nephrotoxicity with cyclosporins; increased serum concentrations with hydantins and lithium; increased toxicity with methotrexate, increased blood pressure with sympathomimetics; and increased prothrombin time with anticoagulants.
Preoperative emergencies
Identifiable endodontic emergencies fall into the following categories:
Emergencies of pulpal origin
Diagnosis
The innervation of the dental pulp consists of myelinated Aδ fibres and unmyelinated C fibres, which give rise to distinct types of pain sensations as discussed in Chapter 4. Pulpal pain is typically stimulated by hot or cold stimuli, however, it is important to be clear whether the pain has the sharp quality attributable to Aδ fibre stimulation or the dull aching, throbbing quality associated with pulpitis and C fibres. Many dentists confuse localizable dentine sensitivity with the unlocalizable pain of pulpal origin. Identification of the tooth is not helped by the perception of the patient, as to which tooth is the culprit; even dentists with toothache get it wrong. Pulpal pain only becomes localizable when the inflammation is advanced enough to involve the periapical tissues and the tooth becomes tender to touch or tap.
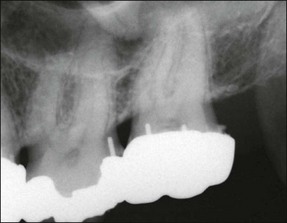
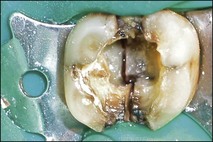
The dentist should seek all historical, clinical and radiographic clues to identify the cause. Sometimes, this will be obvious, such as secondary caries or crack (Figs 10.13, 10.14a) and, at other times, the patient may present with a quadrant of teeth with deep restorations (Fig. 10.15), all posing as potential candidates. It is not unheard of that, under such circumstances, several teeth end up with pulp extirpations. It is important to differentiate the causative tooth by using a combination of pulpal stimulation (uncomfortable as that may be) and selective, diagnostic local anaesthesia. There is no local anaesthetic technique that can be completely confined to one tooth but intraligamental anaesthesia affords a close possibility. The principle is to choose the most likely candidate but to anaesthetize from the mesial to distal and maxillary to mandibular. When the pain is abolished, the tooth is identified; effectiveness of anaesthesia may be tested by pulp testing.

Fig. 10.13 Irreversible pulpitis in mandibular first molar showing a widened periodontal ligament space around both apices
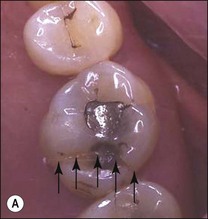


Fig. 10.14 (a) Vertical unrestorable fracture in maxillary molar (arrowed); (b) maxillary molar following extraction; (c) maxillary molar with separated fractured segment
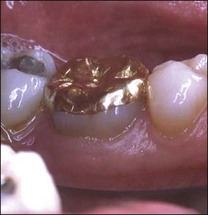
The distinction between reversible and irreversible pulpitis is not clear-cut. In both cases, there may be pain stimulated by hot, cold or sweet stimuli, lingering for various periods of time as a dull ache, sometimes arising spontaneously and sometimes keeping the patient awake at night. At times, the pain may be so severe that the patient will find it intolerable, described as the worst imaginable pain and likened to being stabbed in the jaw with a red-hot poker or knife. The longer the episodes of lingering pain, the more spontaneous the episodes, the greater the frequency of sleep loss, the more severe the pain, the greater the response to hot rather than cold (indeed sometimes cold may relieve), the more likely it is that the pain will be judged irreversible. Indeed, severe pulpal pain of the sort described may sometimes be associated with a relatively normal pulp (Seltzer et al., 1963; Dummer et al., 1980). In the case shown, placement of cast onlays resulted in pain characteristic of irreversible pulpitis, however, the patient was able to tolerate the pain and in time, the pain resolved. Many years on, the teeth respond normally to pulp tests and remain free of apical disease (Fig. 10.16). Patients unable to tolerate the pain would opt to have the pulps extirpated, therefore, the correct term for the diagnosis is pulpalgia rather than pulpitis.


Fig. 10.16 (a) Symptoms consistent with irreversible pulpitis were triggered following placement of cast onlays on the mandibular molars; (b) symptoms resolved spontaneously after 2–3 months, whilst the teeth continued to respond normally to pulp tests, remaining free of apical disease many years afterwards
Cracked tooth syndrome (CTS) may also result in pulpitis and the crack may need additional management by placement of an orthodontic band to prevent cuspal flexure and catastrophic fracture. The degree of pain may vary considerably, from momentary pain on encountering heat and cold to spontaneous pain or pain on biting. The pain on biting will have a sharp quality, while the pain on hot and cold may vary from sharp to a dull aching quality. A fibreoptic light may be useful in locating and determining the extent of the cracks (Fig. 10.17) but they are not always visible in the early stages of CTS.
Treatment
If it is judged that the pain is due to reversible pulpitis, treatment involves removing the source of dentinal or pulpal irritation. In the case of sensitive dentine, patent dentinal tubules may be treated using fluoride or desensitizing agents. Dental caries and faulty restorations should be removed and replaced with a sedative dressing, typically containing zinc-oxide/eugenol (Fig. 10.18).
If it is judged that the pain is due to irreversible pulpitis, the pulp should be extirpated (Fig. 10.19). The ideal emergency treatment for irreversible pulpitis is to remove the diseased pulp completely and to clean and prepare the pulp canal system. Irrigating the pulp chamber with a 2.5–5.0% solution of sodium hypochlorite ensures disinfection before canal instrumentation. If time does not allow this, removal of pulp tissue from the pulp chamber and coronal part of the root canals is often effective. The use of corticosteroid preparations in vital root canals has been advocated in situations where complete instrumentation is inconvenient or impossible because profound anaesthesia cannot be secured. In the presence of severe pulpal inflammation, the effectiveness of local anaesthesia is reduced as discussed above.
In cracked teeth, dentine bonded materials may prove useful in small cavities as an interim restoration before constructing a restoration giving occlusal protection (Fig. 10.20). Once a vertical crack is initiated, the treatment goal is to prevent catastrophic propagation and retain the tooth for as long as possible; some teeth can last up to 10 years with cuspal protection.
Where a crack involves the pulp and symptoms suggest an irreversible pulpitis, all restorations should be removed from the tooth and the extent of the crack determined. If the crack has propagated to a fracture and a portion of the tooth is mobile it should be removed, examined, and the possibility of restoring the remaining tooth substance established (see Fig. 10.14a). Examination of the extracted fragment allows accurate assessment of the restorability of the tooth. Where the fracture runs into the apical periodontal attachment apparatus, as in this case, then extraction is the only option (see Fig. 10.14b,c). If the tooth is restorable, root canal treatment may commence. Should the fracture line run through the floor of the pulp chamber, then it is unlikely that the tooth will respond to treatment in the long term.
In cases where the tooth is cracked but is incomplete, the crown should be supported with a metal band (Fig. 10.21) and root canal treatment commenced. The long-term prognosis of posterior teeth with oblique fractures above the alveolar crest and involving only the roof of the pulp chamber is higher than vertical fractures involving the floor of the chamber (Fig. 10.22).
Whether the treatment consists of a pulpotomy or pulpectomy, there should be 50–75% reduction in the severity of the pain within one day but the residual pain may linger for 24–48 hours gradually reducing over the following 24 hours (total 72 hours). It may take a further 7–28 days gradually to subside completely (Fig. 10.23). The lingering pain may be worse when a complete pulpectomy with cleaning and shaping is performed. If symptoms continue beyond this time, the presence of residual inflamed pulpal tissue should be investigated in the root canal system in the form of an undiagnosed canal.
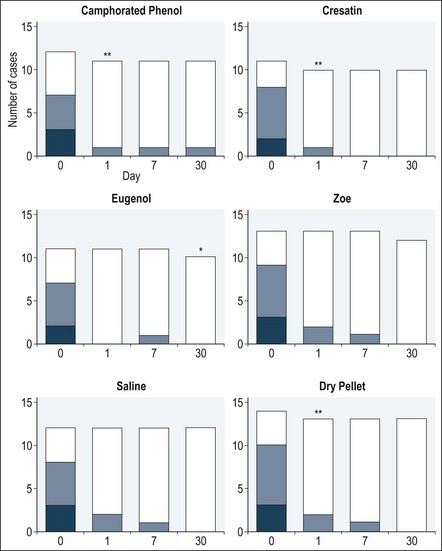
Fig. 10.23 Number of cases presenting with symptoms over a 30-day period following root canal dressing using various materials (darkest shade = pain, intermediate shade = discomfort, lightest shade = no symptoms; * patient did not attend for the 30 day clinical examination; ** patients needed further emergency treatment) (Ha/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses




 RN + H+
RN + H+