chapter 11 Inhalation Sedation: Historical Perspective
BEGINNINGS (PRE-1844)
As difficult as it is to imagine, the gases oxygen (O2) and N2O were once unknown. It was not until 1771 that the German scientist Karl Scheele and the Englishman Sir Joseph Priestley (1733-1804), working independently, discovered O2. In 1727, O2 had been prepared by Stephen Hales; however, he did not recognize that it was an element, and credit for the discovery of O2 is given to Scheele and Priestley. The year following the discovery of O2 Priestley discovered N2O.1,39
During the late 1700s a branch of science known as pneumatic medicine came into being. Thomas Beddoes’ Pneumatic Institute in Bristol, England, became one of the major centers of investigation of the newly discovered gaseous “vapors.” It was at this time that Sir Humphrey Davy (1778-1829) became interested in the study of these gaseous agents. In 1795, at the age of 17, Davy had become an apprentice to the surgeon J. B. Borlase and, during his stay with Borlase, had experimented with N2O and the effects of its inhalation. Davy became the superintendent of the Pneumatic Institute in 1798 and a year later published his book Researches, Chemical and Philosophical; Chiefly Concerning Nitrous Oxide. In this book Davy hinted that the inhalation of N2O might be used to diminish pain during surgical procedures. He also provided the still commonly used nickname “laughing gas” (Figure 11-1). The following is an excerpt from Davy’s work on N2O in which he explains the effects of the agent on himself following self-administration for a toothache and gingival inflammation:
On the day when the inflammation was the most troublesome, I breathed three large doses of nitrous oxide. The pain always diminished after the first four or five inspirations; the thrilling came on as usual, and uneasiness was for a few minutes swallowed up in pleasure. As the former state of mind returned, the state of organ returned with it; and I once imagined that the pain was more severe after the experiment than before. … As nitrous oxide in its extensive operation appears capable of destroying physical pain, it may probably be used with advantage during surgical operations in which no great effusion of blood takes place.2
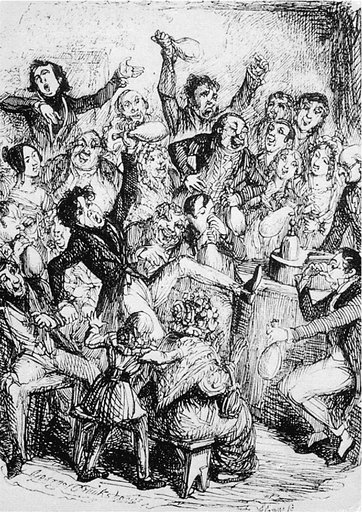
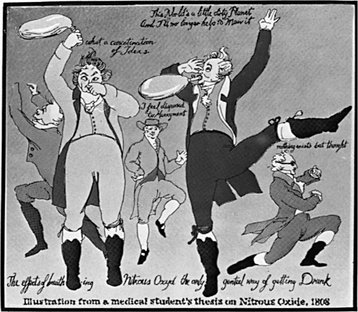
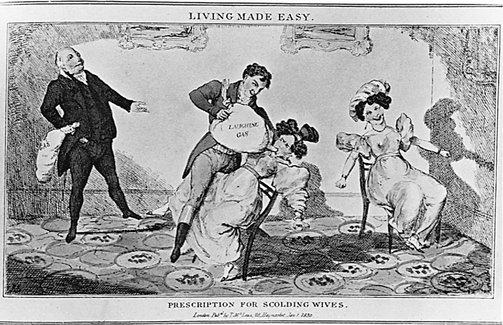
Unfortunately, both Davy and the rest of the medical profession failed to take serious notice of N2O or to administer it for the relief of pain during surgery. One of the reasons for this failure to even try these newer gaseous agents was the fact that during the late 1700s and early 1800s, “ether frolics” and “laughing gas demonstrations” were a popular source of entertainment and enjoyment among younger people (Figure 11-2). Ether (ethyl ether) had been first described by Valerius Cordus in Germany in 1540, who called it sweet vitriol.1 In 1794, Beddoes3 reported that ether produced a deep sleep. As with N2O, however, ether had also been used as a source of entertainment in the late eighteenth and early nineteenth centuries. The thought that agents such as ether and N2O, which were commonly used to produce intoxication, could ever be employed during surgery as a means of abolishing pain was offered serious consideration by very few persons.
One of these persons, Henry Hill Hickman (1800-1830), an English physician, experimented with the use of carbon dioxide (CO2) for the creation of “suspended animation.” Hickman successfully performed surgical procedures on animals using the inhalation of CO2 to abolish pain during the procedure. In 1824, Hickman’s paper, “A Letter on Suspended Animation,” was published.4 Unfortunately, the medical profession did not take notice, and Hickman’s potentially important research was ignored and forgotten.
In 1842, two other ambitious men took the great step forward and successfully administered ether to a patient during a surgical procedure. In Rochester, N.Y., Dr. W.E. Clark administered ether to a patient having a tooth extracted by a dentist, Dr. Elijah Pope. In Georgia, Dr. Crawford W. Long administered ether to John Venable for the removal of a tumor from his neck. It is interesting that neither of these persons thought this discovery important enough to write about it in the scientific journals. Dr. Long finally wrote about his use of the agent, stating that he had used it on three occasions in 1842 and on at least one occasion annually since that time.5 The date of Long’s paper was 1849, years after he had originally used ether clinically. The purpose of the paper was to lay claim to the title of the “Founder of General Anesthesia,” which was at that time being contested among Morton, Wells, and Jackson, three men who are discussed shortly.
THE EARLY DAYS (1844-1862)
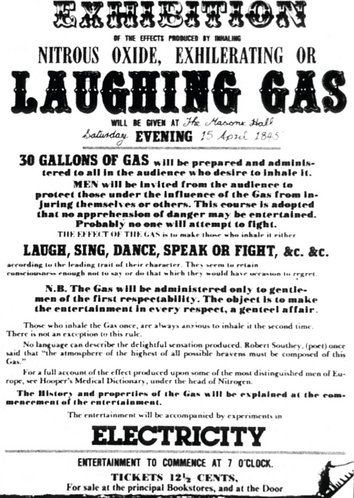
On December 10, 1844, in the town of Hartford, Conn., Professor Gardner Quincy Colton presented a popular science lecture. Professor Colton was an itinerant medical school dropout from Columbia University, traveling around the countryside presenting his show of new scientific and quasi-scientific discoveries to eager audiences.6 In his show, N2O gas was discussed and demonstrated, and as a part of the demonstration, male volunteers were invited from the audience to partake of the effects of N2O (Figure 11-3). Women were also permitted to try N2O, but not in the presence of the men. A private session was held for the women.
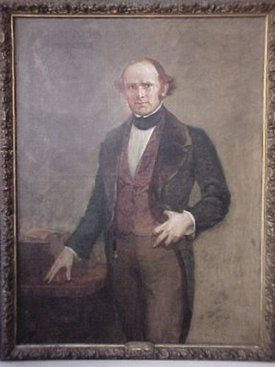
A Hartford dentist, Dr. Horace Wells (1815-1848), was in the audience on this particular evening (Figure 11-4). Wells had a productive dental practice but, being an especially sensitive person, had difficulty in dealing with the terrible anguish and suffering of his patients. In the early 1840s, in dentistry as in medicine, medications for the prevention and relief of pain were nonexistent. At the demonstration a store clerk by the name of Samuel Cooley volunteered to receive N2O. Breathing 100% N2O from a spigot attached to a bladder bag filled with the gas, Cooley quickly became intoxicated, running about the stage. During his running about, Cooley’s leg hit the side of a table quite hard, yet Cooley continued to carry on as before, apparently oblivious of his injury. The skin had been broken, the wound bleeding, but there was no indication that Cooley either felt discomfort or was even aware of the injury. Wells spoke with Cooley after the incident and confirmed that he had been unaware of the injury.
Wells discussed this occurrence with Professor Colton and arranged for a demonstration of N2O at Wells’ dental office the next day. At the office, on December 11, 1844, a reluctant Colton served as the anesthesiologist as another dentist, Dr. John Riggs, extracted a wisdom tooth from Dr. Wells. After recovering from the effects of the N2O, Wells stated that he had been totally unaware of the procedure and that there had been absolutely no pain associated with it.7 Wells was taught the process of manufacturing N2O by Professor Colton and shortly thereafter began using N2O in his dental practice with great success.
Through his association with William T. G. Morton, Wells was able to gain permission to demonstrate his newly found technique to the medical students and faculty at the prestigious Harvard Medical School. Morton, a dentist who became a student and later a partner of Dr. Wells in Hartford, eventually left dentistry, becoming a medical student at Harvard. Morton was present in the audience on this fateful day. Using a medical student volunteer as a patient, Dr. Wells administered N2O to the patient through a newly developed inhaler. As the patient lapsed into unconsciousness, Wells had to remove the inhaler, pick up his instruments, and attempt to extract the volunteer’s infected tooth. During the extraction attempt the patient cried out. The audience, assuming that the procedure had failed, proceeded to boo and hiss Wells until he was forced to leave the demonstration hall, thoroughly humiliated and his demonstration a failure.8
A second possible explanation is the concept of biologic variability. As is well known today and has been stressed throughout this text, people respond differently when given the same dose of a drug. This concept is illustrated with the so-called bell-shaped, or normal distribution, curve (see Figure 7-1).
Within a year or so of his ill-fated demonstration of N2O, a discouraged Wells abandoned the practice of dentistry. He ceased to publicize N2O and to attempt to introduce it into clinical use, although he personally knew that it could be used successfully. He was able to earn a living by partaking in several strange occupations—buying pictures in Paris to sell in the United States and traveling around the countryside with a troupe of singing canaries. Wells continued to experiment with newer inhalation agents and soon became addicted to chloroform. Many of the founders of anesthesia became addicted to the chemicals they discovered, for they had no one to experiment on but themselves. The concept of addiction was unknown at the time and proved to be a terrible personal price to pay for the introduction of newer drugs and chemicals.9
In May 1848, a friend of Wells asked him to provide a vial of sulfuric acid so that he could throw it at a prostitute who earlier had damaged his clothes. Several days later, after Wells had inhaled some chloroform, he returned alone to Broadway in New York and while under the influence of the chloroform threw sulfuric acid at two other prostitutes. Arrested and placed in jail for these acts, Wells took his own life. The following are excerpts from the last letters written by Wells.10
On May 30, 1848, Horace Wells, later acknowledged as the founder of anesthesia, committed suicide while in jail by cutting the femoral artery in his left thigh with a razor. Prior to this act, Wells had inhaled some chloroform to produce insensibility to the pain.11
Interestingly, N2O was reintroduced in 1863 by Professor Colton in New Haven, Conn.12 The Colton Dental Association devoted the next 33 years to extracting teeth under N2O. With 193,800 patients and no recorded fatalities, N2O became the most commonly used inhalation anesthetic, a position it still maintains today.
Toward evening a man residing in Boston came in, suffering great pain, and wishing to have a tooth extracted. He was afraid of the operation, and asked if he could be mesmerized. I told him I had something better, and saturating my handkerchief, gave it to him to inhale. He became unconscious almost immediately. It was dark, and Dr. Hayden held the lamp while I extracted a firmly-rooted bicuspid tooth. There was not much alteration in the pulse and no relaxing of the muscles. He recovered in a minute and knew nothing of what had been done for him. He remained for some time talking about the experiment. This was the 30th of September 1846.9
Morton continued to experiment with ether, both on his own and with Dr. Henry J. Bigelow, for whom Morton administered ether for more than 37 operations. All of these cases were done prior to the famous demonstration of ether at the Massachusetts General Hospital in 1846.13
On Oct. 16, 1846 (now called Ether Day), Morton administered ether to Gilbert Abbott (Figure 11-5). The famous surgeon John Collins Warren excised a tumor from the jaw of Mr. Abbott. Although considered an absolute success, Morton’s demonstration was actually little more successful than Wells’ had been. Abbott later mentioned that when the incision was first made it felt as though his neck had been scratched by a hoe. However, unlike Wells, Morton was not hissed out of the operating theater. The reason for this is twofold: first, Dr. Bigelow had attested to Dr. Warren the success of ether; therefore Warren was more inclined to believe that this new agent was not a fraud but in fact the real thing. Second, and of considerable importance, is the fact that Morton was a physician and not a dentist. At the time, dentistry was looked down on by the medical profession as a mere trade. That Wells should have even attempted to demonstrate his new technique to such an august group, including Warren, was, sad to say, quite laughable. His audience was filled with cynics and disbelievers. Morton, on the other hand, being a member of the “club,” was more readily accepted. When the endorsement of Bigelow is added, it is readily seen why the less than absolutely successful procedure was proclaimed as the great event it truly was. In the words of John Collins Warren, “Gentlemen, you have witnessed a miracle. This is no humbug!”13–15
Ether had been for many years a popular agent for enjoyment. Ether follies were a popular form of entertainment, especially among medical students. Morton, acutely aware that if he were to suggest that this same agent be used for a serious purpose he might also be laughed at, modified the agent. He added a dye to it and called it Letheon, thus gaining acceptance for it among his colleagues.16 The surgical amphitheater at the Massachusetts General Hospital in which this famed event took place has been preserved and is today known as the Ether Dome.
News of Morton’s “etherization” spread rapidly throughout the United States and Europe, creating a degree of celebrity for Morton. On Dec. 21, 1846, Dr. Robert Liston performed the first surgical procedure under “etherization” in England. Almost immediately following the introduction of etherization into surgery by Morton, Dr. Charles T. Jackson came forward to lay claim to its discovery, stating that it was he who had suggested its use to Morton, had advised him about the nature of the agent, and had advised him of the best manner in which to administer it. The controversy was only beginning. Soon Morton, Wells, and Jackson were engaging in bitter accusations and secret deals, each in an effort to prove that it was he in fact who was the sole founder of anesthesia. To complicate the matter still further, Crawford W. Long, who had first administered ether in 1842, came forward in 1849 to lay claim to this title.17
The name etherization was used for only a short time, and a more acceptable name for />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses