Ceramic Materials in Implant Dentistry
Parag R. Kachalia
University of the Pacific Arthur A. Dugoni School of Dentistry, San Francisco, California, USA
Introduction
Over the last century, monumental improvements have occurred in dentistry and patients today have the ability to maintain their teeth for a lifetime, if they are healthy individuals and they are diligent with their overall oral health. In the event a single tooth or multiple teeth are lost, implant therapy can be utilized to restore the missing dentition. The challenge, however, is to fabricate an invisible replacement that will last for decades, given the growing esthetic demand and extended life expectancy. Since the introduction of endosseous implants, evidence‐based documentation has reported high implant survival rates, but more recently there has been an emphasis on biological, technical, and esthetic success outcomes measurements. Unfortunately, esthetic success with metal‐based restorations has not always been predictable. On the other hand, continual developments with all‐ceramic materials have led to restorative alternatives that can satisfy specific hue, saturation, and light refraction/reflection needs while providing durability. However, the selection and management of these materials may be less forgiving than metal‐based ceramics. This chapter will address the protocols for utilization of all‐ceramic implant restorations. In addition, new materials utilizing the properties of resin and ceramics will also be discussed as they may show some promise in providing a dampening behavior and ease of reparability.
Materials
Dental ceramics have continued to improve over the last quarter century and ceramics are no longer restricted to only being used in the anterior sextant of the mouth. Over this period of time new developments have focused on creating ceramics that are biocompatible, durable, and esthetic. Ceramics have always had a high esthetic potential and well‐trained ceramists have been able to create beautiful anterior restorations that blend seamlessly with the natural dentition. Unfortunately, in historical terms this beauty was not paired with strength. Dental ceramics have generally had low fracture toughness and traditional ceramics, such as feldspathic porcelain, were highly dependent on being fused to metal substructures in order to have intraoral success in the posterior aspect of the dentition.1 Leucite‐ and alumina‐based materials, such as IPS Empress (Amherst, NY) and Procera Alumina (Zurich, Switzerland) respectively, had come to market to combat some of the issues evident with feldspathic porcelain; however, advancements in leucite‐based materials and alumina‐based material have stagnated and the use of these materials in dentistry is clearly fading away.
Two key areas of evolution in ceramic dentistry have occurred, one is in the lithium disilicate arena and the other is in the zirconia arena. The primary reason for migration towards these materials is the fact that both materials can be utilized as either core materials or as monolithic materials that can be used in full contour. The ability to use these materials monolithically may help combat a significant portion of the chipping and fracture issues traditionally evident when ceramics are used as a veneering material.2
Lithium disilicate
The crystalline phase that forms in the manufacturing of this ceramic is lithium disilicate (Li2Si2O5) and it accounts for approximately 70% of the total volume of glass.3 The interlocked microstructure of lithium disilicate happens to occur in a random pattern and this is thought to give the material its ability to deflect cracks and minimize propagation. In fact, lithium disilicate exhibits a flexural strength of 350–400 Mpa, compared to the 160 MPa flexural strength of leucite glass. It also exhibits fracture toughness of approximately three times that of leucite glass. These properties allow this material to be used as a core that can be layered with veneering ceramic or as a material that can be used monolithically. The monolithic utilization of lithium disilicate appears to be most promising and, since Ivoclar Vivadent’s (Amherst, NY) introduction of IPS e.max in 2009, practitioners around the world have adopted this material and have had very good success in using the material for anterior and posterior full‐coverage single‐unit restorations, veneers, inlays, onlays, and selective three‐unit fixed partial dentures, replacing a single anterior tooth or a first bicuspid.
The material is available as IPS e.max Press or IPS e.max CAD (Figure 11.1). IPS e.max Press utilizes a traditional lost wax technique and exhibits a flexural strength of 400 MPa. IPS e.max CAD is manufactured and sold in a partially crystalized state with a purple to bluish hue and has an initial flexural strength of 160 MPa. This partially crystallized state is used to allow for efficient milling and simple chairside adjustment during intraoral fitting. Once the restoration is placed into a porcelain firing oven with the proper cycles, a final crystallization occurs and the material achieves its final esthetic appeal as well as its greater flexural strength of 360 MPa. The crystals of both the IPS e.max Press and IPS e.max CAD are the same in composition; however, the length and size of these crystals are different, leading to a difference in fracture strength and fracture toughness. The fracture strength of IPS e.max Press is approximately 10% greater than its counterpart and its fracture toughness is approximately 20% greater than that of IPS e.max CAD.


Figure 11.1 (a) IPS e.max pressable ingot. (b) IPS e.max CAD block.
Zirconia
In the general marketplace many types of zirconia are present; however, in dentistry 3% yttria‐stabilized zirconia oxide is what is typically used in dental prostheses. Zirconia is used in dentistry because of its biocompatibility, favorable physical properties, and its appearance. The strength and esthetic benefits of zirconia allow it to be utilized as a replacement for traditional dental alloys. Over the last decade zirconia has been used quite extensively for single‐unit, full‐coverage extracoronal restorations as well as for fixed dental prostheses in the posterior dentition. Historically these areas were restored utilizing metal‐based restorations; however, the strength of zirconia allows it to act as a viable tooth‐colored alternative compared to traditional metal‐based restorations. On the periodic table, zirconia is classified as a metal; however, in dentistry it is commonly classified as a ceramic due to its tooth‐colored appearance. In order to maintain alignment with common perception and limit confusion zirconia will be discussed as though it is a ceramic. Zirconia’s strength properties are considerably greater than those of feldspathic or glass ceramics. It can exhibit flexural strength properties up to 1200 MPa and fracture toughness KIC values of 3.2 MPam(1/2).4,5 This material is the most durable of all dental ceramics and its structural value derives from a phenomenon termed “transformation toughening”. Transformation toughening occurs in zirconia due to the transformation of meta‐stable tetragonal grains to stable monoclinic grains around the crack tip. This process is thought to limit crack progression in the material. These favorable physical properties paired with its relative tooth color have expanded zirconia’s use in dentistry.
Zirconia first came to the dental market in the late 1990s and, for the first decade, it was only used as a dentin‐colored core material to support veneering ceramic (Figure 11.2). In the early days of veneered zirconia restorations, numerous incidences of chipping and delamination of the veneering ceramic were being reported. These unusual occurrences were thought to be due to traditional feldspathic porcelain being used as a veneering ceramic and it having a different coefficient of thermal expansion than that of the zirconia core, but it was later demonstrated that residual stresses were introduced by fast cooling of the restorations upon removal from a porcelain furnace.6,7 The clear benefit of placing a veneering ceramic onto a zirconia coping is that an esthetic restoration can be achieved while having similar properties and indications to a traditional metal–ceramic restoration. Veneering ceramic chipping or delaminating from a zirconia core is less prevalent today then in years past. There is emerging science to understand the etiology of these fractures using fractology, which has disclosed that failures originate below the occlusal surface because of hoop stresses and do not involve the interface.8,9 This phenomenon underscores the importance of minimizing stresses by eliminating axial wall binding and achieving sufficient occlusal thickness of the restoration.
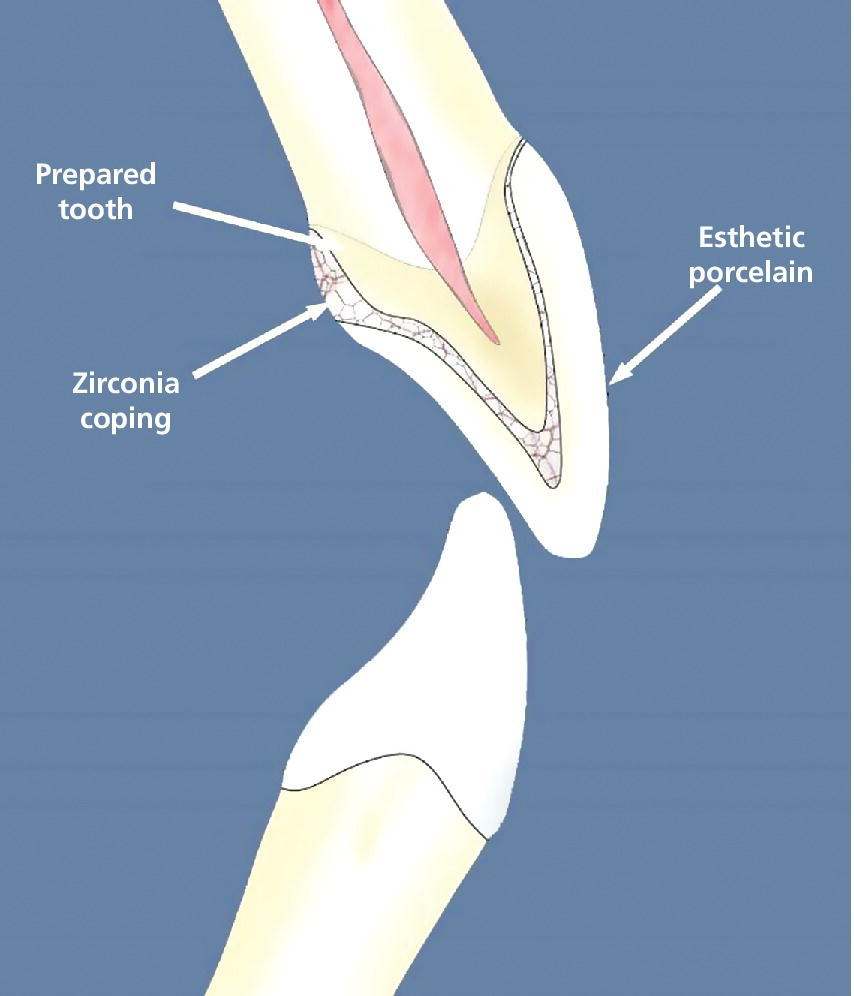
Figure 11.2 Cross‐section of layered zirconia crown depicting zirconia and veneering porcelain.
Source: Courtesy of Jeff Miles.
The fabrication process has also undergone scrutiny. The improved performance of veneered zirconia restorations is due not only to the slow cooling process but also the use of anatomic copings,10 as well as utilizing veneering ceramics that have been specifically developed to be applied directly to zirconia substructures. In fact, a study, which followed over 1000 of each zirconia‐based and porcelain‐fused crowns for more than 7 years, found that survival probabilities did not differ between the two and were independent of the molar or bicuspid site.11 The improvements in veneered zirconia restorations have run parallel with the developments of utilizing zirconia as a monolithic material for both single‐unit restorations as well as fixed dental prostheses.
The original concerns surrounding chipping of veneering ceramic (Figure 11.3) led researchers and material scientists down a path to see if zirconia could be utilized monolithically. The clear benefit of zirconia is that it offers a high flexural strength (800–1000 N), and a restoration made solely of this material may be able to hold up to the maximum occlusal forces.12 The initial caveats of utilizing zirconia as a monolithic material were that the material may cause significant amounts of wear on the opposing dentition and the material would be too opaque to be considered an esthetic alternative to monolithic metal restorations. To address the concern of wear on the opposing dentition, numerous researchers have studied the impact monolithic zirconia may have on enamel, and it has been shown that, when monolithic zirconia is hand polished to a high luster, it has a similar wear rate on enamel as enamel has against itself.13 In regard to the esthetic potential of monolithic zirconia restorations, new monolithic zirconia materials are coming to market that offer higher translucency levels that allow these types of restorations to be utilized on anterior teeth.14 These more translucent materials are being achieved by altering the grain size of yttria‐stabilized zirconia as well as the introduction of various trivalent oxides to the manufacturing process.15,16

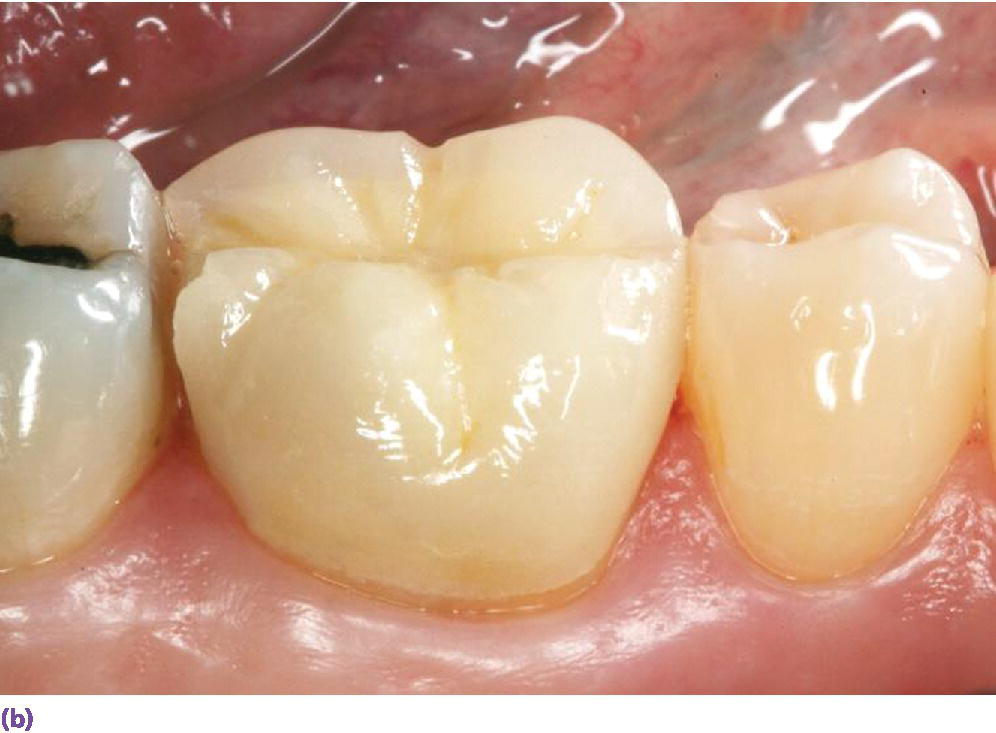
Figure 11.3 (a) Layered zirconia restoration with veneering ceramic fractured.
Source: Reproduced with permission from Charles Goodacre. (b) Layered zirconia restoration with marginal ridge veneering ceramic fractured.
The advances in glass‐based ceramics as well as polycrystalline ceramics are allowing these materials to be used predictably on natural teeth and they should be considered as reasonable alternatives to traditional metal‐based ceramics for implant restorations.
Abutments
If one is to restore an implant utilizing an abutment‐based approach, this abutment will have an esthetic as well as a physical property impact on the complete implant restorative complex, if an all‐ceramic restoration is to be prescribed. The trend over the last decade has been a move away from stock abutments towards customized CAD/CAM abutments. This change allows for an abutment that has optimal margin design, while allowing for appropriate retention and resistance form for each patient. The digital dental workflow, utilizing scanning and milling technologies, has allowed the cost of custom abutments to decrease substantially, making them more accessible for the average dental practice. CAD/CAM abutments are primarily produced utilizing titanium or yttria‐stablized zirconia. Zirconia abutments have generally been considered in the esthetic zone because of their coloration; however, titanium abutments that have been gold anodized may also be considered in moderate esthetic areas, as they may offer some physical property advantages while providing reasonable esthetics (Figure 11.4).


Figure 11.4 (a) Zirconia CAD/CAM abutment in place. (b) Gold hue abutment in place.
Zirconia abutments
Zirconia abutments have been utilized in the anterior region as well as the premolar region with high survival rates and the annual failure rate appears to be similar to that of metal abutments.17 Yttria‐stablilized zirconia abutments have the clear advantage over titanium abutment in terms of esthetics. The ability to colorize zirconia abutments into various shades allows for better color of the periodontium as well as the coronal restoration (Figure 11.5
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


