Chapter 11 All-ceramic crowns
The porcelain jacket crown
The addition of alumina to feldspathic porcelain was reported by McLean and Hughes in 1965 and resulted in much stronger dental porcelain which was more resistant to crack propagation. However, aluminous porcelain does not have the same aesthetic qualities as feldspathic porcelain; it does not have the same translucency and cannot reproduce the life-like illusion of a natural tooth crown. Instead, aluminous porcelain can be used to form a coping over the crown preparation (Figure 11.1), which is itself covered with more aesthetic feldspathic porcelain. Using this principle, the first widely used all-ceramiccrown was developed and was often referred to as the porcelain jacket crown (PJC). This development increased the strength of the PJC to around 120–150 MPa by reducing the likelihood of crack propagation.
The PJC was widely used to provide an aesthetic restoration for upper anterior teeth. However, it was still not strong enough to resist much occlusal loading without the crown breaking (Figure 11.2). Its use was, therefore, confined mainly to upper incisors, and some premolar teeth in minimal occlusal function. This type of crown is not indicated for molar teeth.
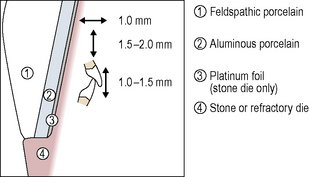
The tooth preparation for and construction of a PJC is described in a stylized diagram in Figure 11.3. The crown preparation requires a shoulder margin all around the gingival aspect of the preparation with an axial reduction of approximately 1.0–1.5 mm. Reduction at the incisal edge is in the order of 1.5–2.0 mm with 1.0–1.5 mm interocclusal clearance required.
Fabrication
Instead of a stone die model, refractory material may be used which maintains its dimensional stability when subjected to the heat of the porcelain furnace (see Chapter 12 on ceramic veneers). It has been argued that the use of a refractory die results in a more accurate fit of the final restoration to the prepared tooth.
Decreasing tooth tissue reduction for an all-ceramic crown
The dentine-bonded crown
The use of dentine-bonded crowns is mainly for anterior teeth where occlusal loading is relatively low (Figure 11.4). Such restorations are contraindicated for those patients with an obvious bruxing habit. Application of this type of restoration for premolar and molar teeth, which are normally subject to higher occlusal loading, should be made with caution and after careful examination of the patient’s occlusion. Generally, such applications should be avoided. The patient seen in Figure 11.5 has four posterior dentine-bonded crowns chosen for optimum aesthetics as the patient was young. No signs or symptoms of bruxism were noted and canine guidance was achieved; however, despite this, the lower crown fractured and had to be replaced with a metal–ceramic crown.
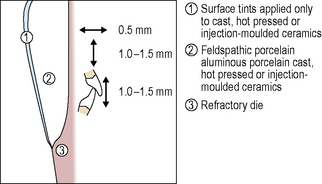
Tooth preparation for dentine-bonded crowns is kept as minimal as possible and less than that required for metal–ceramic crowns or a traditional PJC. The preparation, in some instances, can be confined to enamel. However, the ceramic should be sufficiently thick to mask discoloured teeth prior to cementation. A minimal shoulder or, more often, a minimal chamfer is the restoration margin of choice. All margins should be supragingival wherever possible to avoid the problems of moisture control at cementation. The axial reduction is in the order of 0.5 mm while the occlusal reduction is between 1.0 and 1.5 mm, with at least 1.0 mm reduction in all excursive movements associated with the preparation (Figure 11.6).
In common with other all-ceramic crown preparations, line and point angles should be rounded to avoid stress concentrations within the porcelain. Figures 11.7–11.9 show the tooth preparation that was carried out for the patients seen in Figures 11.4 and 11.5. Marked palatal erosion (Figure 11.7) has led to exposure of the tertiary (reactionary) dentine that has formed. The only preparation carried out palatally is the cervical chamfer; the tooth wear has removed the rest of the palatal tooth tissue(Figure 11.7). Interocclusal clearance has been created following anincrease in the patient’s occlusal vertical dimension by placing gold onlays on some of the posterior teeth (Figure 11.8).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses