10
10
The Surgical Correction of Common Deformities
- Single Jaw Deformities
Mandibular prognathism
Mandibular asymmetry
Mandibular retrognathism
The chin
Mandibular incisor proclination
Maxillary hypoplasia
Nasomaxillary hypoplasia
Malar-maxillary hypoplasia
Maxillary prognathism - Bimaxillary Deformities
Gross mandibular prognathism
The deep overbite
Bimaxillary proclination
The long face
The open bite (apertognathia)
The large tongue
The short face
Maxillary asymmetry - Unfortunately, the diagnosis of a facial deformity does not always suggest an operative solution. There may be a choice of procedures or the complexity requires several simultaneous osteotomies. This chapter considers both single jaw and bimaxillary deformities. As will be seen, there is usually an overlap and what appears to be a major single jaw problem invariably requires a bimaxillary solution.
- It is also impossible to classify all cases under one treatment group. For instance, a patient with a long face may have an open bite. Both treatment sections in this chapter should therefore be consulted.
- Although it is possible to describe horizontal and vertical deformities separately, they are surgically interdependent, in that a vertical osteotomy will produce a horizontal change and vice versa.
Timing
The choice of age for any orthognathic procedure can be difficult. The optimum age is when facial growth has finished. This is approximately 16 years for girls and 18 years for boys. Later maturation of the face can undo the benefit of a well-intentioned osteotomy. This is particularly true if the prognathic mandible is treated too early. The only exception is the rare unilateral condylar hyperplasia which may require ablation of the articular growth cartilage during adolescence to prevent a major degree of secondary deformity. As all young patients with jaw deformities require orthodontic treatment, this provides a period of scrutiny to monitor continued growth with study models and lateral skull radiographs, at yearly intervals. Wrist radiographs when considering abnormal facial growth and sequential technetium-99m bone scans are unhelpful.
Presurgical orthodontic treatment not only simplifies the operative procedure but also improves the occlusal and profile outcome. However a decision must be made if surgery is to be the ultimate treatment of choice. The orthodontic decompensation for surgery for a jaw disproportion will be different from the pure orthodontic compensatory management to conceal the deformity, and will start later to reduce the period in appliance retention. Therefore, please read Chapter 4 (Orthodontic Preparation).
The neglected details of planning and data transfer and fixation are to be found in Chapters 7 and 8 and those for each operation are described in Chapter 9.
Single Jaw Deformities
Mandibular Prognathism
This is characterised by elongation of the mandible producing a negative overjet, with compensatory retroclination of the lower incisors, and proclination of the upper incisors. Both the dentition and jaws show a marked Class III relationship. Some patients also have an increased lower facial height which is automatically reduced when the mandible is displaced backwards, up an inclined occlusal plane (Figure 10.1).
Beware of seeing all negative overjets as cases of mandibular prognathism. With a mild mandibular protrusion in a man, the preferred aesthetic solution is often a forward movement of the maxilla, leaving a “strong chin”. This profile correction may be predicted by padding out the upper lip with cotton wool or wax. The same cephalometric values in a female usually require a mandibular setback for aesthetic harmony. The occlusal correction is identical in both cases.
Most prognathous mandibles are associated with a degree of maxillary retrognathism with the need for a bimaxillary correction. This becomes clear after presurgical orthodontics with incisor decompensation (see below, Bimaxillary Deformities).
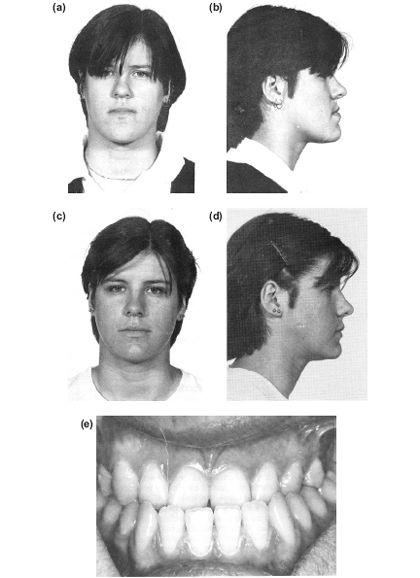

Figure 10.1 Mandibular prognathism requiring moderate orthodontic decompensation of the incisors followed by a sagittal split pushback. (a), (b) and (e) Preoperative. (c), (d) and (f) Postoperative.
Treatment
Presurgical orthodontics will be required to correct arch size discrepancy, overcrowding and to decompensate the incisors. Posterior displacement of the mandible can be achieved by a:
sagittal split osteotomy,
and less commonly,
oblique subcondylar (subsigmoid) osteotomy
a) extraoral,
b) intraoral (buccal approach), and
c) intraoral (medial approach).
Mandibular Asymmetry (Unilateral Hyperplasia and Hypoplasia of the Mandible)
Introduction
There are two distinct types of asymmetrical overgrowth, but hybrid forms are occasionally found with both abnormalities merged on one side or even one of each deformity on opposite sides. Each deformity is frequently attributed to condylar hyperplasia. However, in both types the increased dimension arises beyond the accepted localised area of condylar growth.
Unilateral hypoplasias will be treated in the same manner as mandibular retrognathism, except when part of a hemifacial microsomia deformity, which will require additional attention to the difficult problem of soft tissue deficiency.
Beware of diagnosing asymmetry where a malocclusion is really causing a unilateral displacement of the mandible on closure.
Hemimandibular Elongation
This asymmetry presents with an increased ascending ramus width and length of the body on the affected side, with deviation of the dental and jaw midline to the contralateral side and a crossbite (Figure 10.2). The condylar head may be minimally enlarged compared with the normal side but the neck is elongated. The occlusal plane is undisturbed. Surgical correction should be delayed until the end of adolescent growth particualrly as some cases “creep on” to the end of the second decade.
Treatment
Presurgical Orthodontics
Insufficient maxillary intercanine width to accommodate the lower arch is not uncommon. Surgery should therefore be preceded by maxillary expansion. Where there is a gross discrepancy between the arches the maxillary arch may be expanded with a quadhelix appliance, which increases the width from behind forwards over a period of three to five months. However in such cases, tipping of the molars may relapse postoperatively and produce an anterior open bite. For this reason with large discrepancies surgical expansion of the maxilla may be the treatment of choice or distraction osteogenesis with a bone borne expansion appliance.
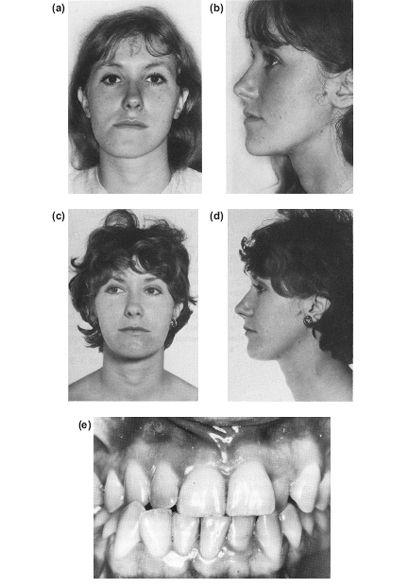

Figure 10.2 Left hemi-mandibular elongation with prognathism and deviation of the midline to the right, corrected by a bilateral sagittal split osteotomy. (a), (b) and (e) Preoperative. (c), (d) and (f) Postoperative.
Surgery
Asymmetry, with or without prognathism, can be corrected by a bilateral ramus osteotomy, such as the sagittal split, which shortens the affected side and allows rotation at the contralateral angle.
Although correction of the bony deformity produces a marked improvement in appearance by eliminating both the unilateral deviation and prognathism, there is often a persistent asymmetry of the face in movement.
Recurrent growth creates a difficult decision and will require a careful high condylar shave preserving the meniscus.
Hemimandibular Hyperplasia
This type of mandibular asymmetry often starts dramatically with the pubertal growth spurt, although it is detectable earlier. Other cases appear to develop insidiously during adolescence. Another enigma is the principal site of overgrowth. Although often considered to be a condylar hyperplasia, there is, in addition to the considerably enlarged condylar head and ascending ramus, a convex downward growth of the lower border of the mandibular body which extends as far forward as the midline. Initially this creates an ipsilateral lateral open bite followed by secondary maxillary alveolar growth. When all mandibular growth is complete, there is an overall hemimandibular hyperplasia and an occlusal cant down to the affected side but no deviation of the midline (Figure 10.3). The inferior dental neurovascular bundle is carried downwards with this growth. This seems to be associated with hyperplasia of the associated mylohyoid muscle in the same way as masseteric hyperplasia produces an enlarged square gonial angle. Excess growth appears to cease in most cases at the end of puberty. It is interesting to see the ipsilateral antral floor is also lower due to remodelling following the alveolar downgrowth.
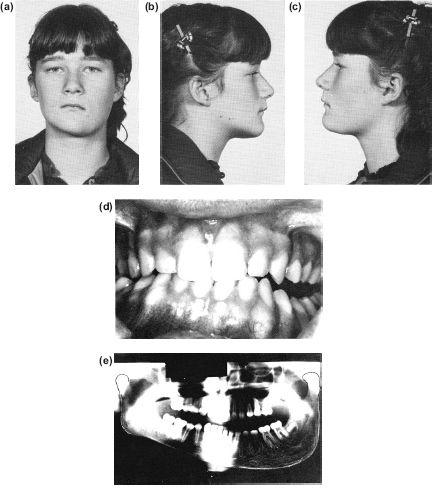
Figure 10.3 (a) to (e) This left hemi-mandibular hyperplasia dramatically occurred over 6 months at the onset of puberty. There is no horizontal displacement of the lower midline despite the increase in vertical dimensions producing a lateral open bite.
Treatment
Early
When seen early, the aim of surgery is to reduce ramus height before the secondary alveolar growth creates a permanent asymmetry with an oblique cant of the occlusal plane. It is tempting to remove part or all of the condyle to ablate the growth centre, i.e. a partial condylectomy. However, not only does the excess growth take place throughout the hemimandible beyond the influence of the condylar growth area, but it has usually finished by the time the deformity is diagnosed. Therefore, at this stage, surgical damage to the joint mechanism would seem unwarranted. A simple approach is a subsigmoid osteotomy, either intraorally or extraorally, to bring the teeth into occlusion. Later the increased depth of the body of the mandible can be corrected with trimming of the lower border and this can be done extraorally through a skin crease incision (see below) or if access permits, intraorally. However the displaced neurovascular bundle must be protected.
Late
Where compensatory alveolar growth has taken place, bringing the separated buccal segment teeth into occlusion, the most economical correction is simply reducing the lower border convexity. This improves the facial appearance and corrects the obliquity of the mouth, but not the occlusal plane (Figure 10.4). However, if desired, the downward tilt of the occlusal plane can be corrected with a bimaxillary procedure elevating the maxilla with a Le Fort I osteotomy (see Maxillary Asymmetry) and the mandible must then be adjusted to this horizontal occlusal plane, either by a sagittal split or subcondylar osteotomy. Finally, the convex lower border will still need to be trimmed. This is sometimes possible intraorally but is more easily achieved in conjunction with an external subcondylar osteotomy through the same skin incision.
Rarely, when all growth seems to have ceased and the deformity has been corrected, the condylar cartilage may suddenly spring to life again. This justifies a condylar cartilage trimming procedure with careful preservation of the meniscus.
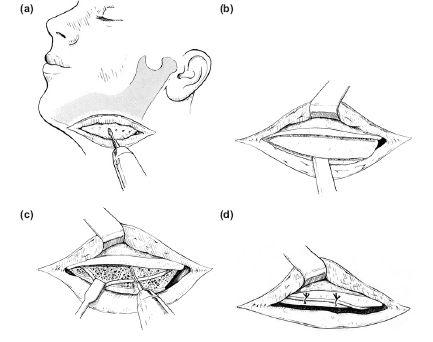
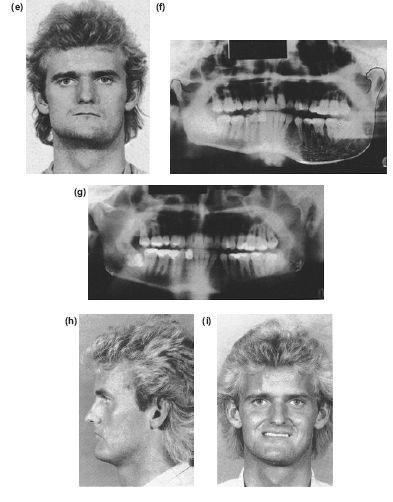
Figure 10.4 Lower border cortical split to expose and preserve the neurovascular bundle prior to trimming the excess depth of mandible. (a) The outer cortical plate is removed. (b) If the neurovascular bundle is found within the hyperplastic lower border, it is dissected from its canal and retracted prior to resection of the inner cortical plate (c) and (d). An adult left-sided hemimandibular hyperplasia where the lateral open bite has closed spontaneously leaving an ipsilateral downward slope of the occlusal plane. The external deformity has been corrected by trimming the lower border of the mandible through an external approach. (e) and (f) Preoperative. (g) to (i) Postoperative.
Trimming the convex mandibular lower border (Figure 10.4).
- An aesthetic incision is made in a low skin increase, or where a crease might be anticipated. The mandible is exposed subperiosteally.
- The lower border excess is outlined with bur holes, using the normal side for comparison (Figure 10.4a).
- These holes are then joined together, cutting only through the outer cortex so as not to damage the inferior dental neurovascular bundle, which is invariably near the lower border.
- A similar cortical bur cut is then made along the lower and posterior border and the excess outer cortex can then be split off with an osteotome, which is inserted in the lower cut, and rotated (Figure 10.4b).
- This allows the neurovascular bundle to be exposed by carefully trimming off its overlying shell of compact bone.
- The bundle is retracted and the excess lingual plate is trimmed off and the margins smoothed (Figures 10.4c and 10.4d). The neurovascular bundle is then left loosely sutured above the new lower border.
- The wound is drained and closed in layers after loosely suturing the neurovascular bundle into the deep aspects of the wound. The skin is sutured with a continuous subcuticular 3/0 Prolene suture.
Figures 10.4e-10.4i shows such a case.
Condylar Hypoplasia
Occasionally it can be difficult to decide whether the asymmetry is the result of unilateral overgrowth or contralateral deficiency. Most unilateral hypoplasias appear to follow neonatal or childhood condylar damage with preservation of the meniscus. In addition to deviation of the chin to the affected side, the condyle is usually short, flattened or deformed. An exaggerated antegonial notch is present on the affected side. As the deficiency in ramus height gives rise to a secondary restriction in maxillary growth, the asymmetry is also reflected in the transverse occlusal plane. This is tilted downwards towards the normal side. Loss of the meniscus through a fracture displacement or destruction by infection or juvenile arthritis may lead to joint ankylosis and an even greater asymmetry due to the lack of functional stimulation to the growing mandible. Such cases require reconstruction of the joint with a costochondral graft (see Chapter 13).
Treatment
Moderate degrees of hypoplasia may be treated like an asymmetrical hyperplasia, with a bilateral sagittal split osteotomy. This will lengthen the affected side and provide a rotation adjustment on the normal side. However, the maxillary occlusal plane has to be levelled first. In adolescence this can be achieved orthodontically after the mandibular surgery by creating a lateral open bite intraoperatively with a unilateral thickened occlusal wafer or splint. The lateral space to be created may be estimated by examining the models mounted with a face-bow on an anatomical articulator. In most cases, a little excess is desirable. Following the sagittal split osteotomy the buccal teeth are brought into occlusion orthodontically (Figure 10.5).
With a large unilateral deficiency, or where there has been previous ramus surgery, the downward and forward mandibular reconstruction can only be achieved with an inverted L osteotomy and interpositional bone graft or distraction osteogenesis (see Chapter 9). Again, the maxillary occlusal plane will also require correction. If the patient is an adult, a Le Fort I osteotomy will be necessary to level the transverse occlusal tilt, and precedes the mandibular correction as part of a bimaxillary operation (see also Maxillary Asymmetry).
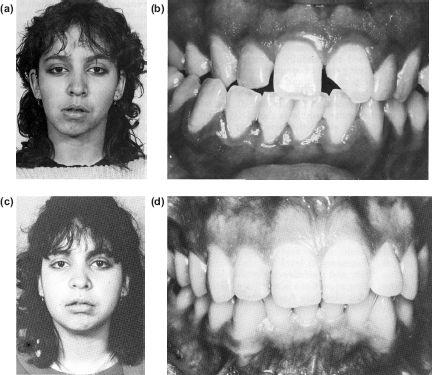
Figure 10.5 Post-traumatic right condylar hypoplasia treated with an inverted L bone graft to increase ramus height and correct the midline deviation. Postoperative orthodontics is used to achieve a horizontal occlusal plane. (a) and (b) Preoperative. (c) and (d) Postoperative.
Mandibular Retrognathism or Hypoplasia
The retrognathic mandible is either too small, i.e. a short Go-Pg, or set too far back with an increased saddle angle (NSAr) or a combination of both.
These cases may be classified as mild to marked skeletal Class II division 1 malocclusions. However, as with unilateral hypoplasias, there are both congenital and acquired forms of this deformity. The more severe, “bird face” deformity can be inherited, or acquired in utero as in the congenital Robin syndrome. One of the common features of this inherited form is a beak-shaped nose, which may also require reduction. In all cases the lower lip and tongue produce a secondary deformity of the maxilla, with dentoalveolar proclination and a narrow arch.
The severe acquired form follows bilateral loss of the condylar growth centres and is usually due to childhood trauma, in which case the condyles are small with no neck, and stigma of a submental scar may be found (Figure 10.6). Occasionally, the patient may have suffered juvenile rheumatoid arthritis (Still’s disease).
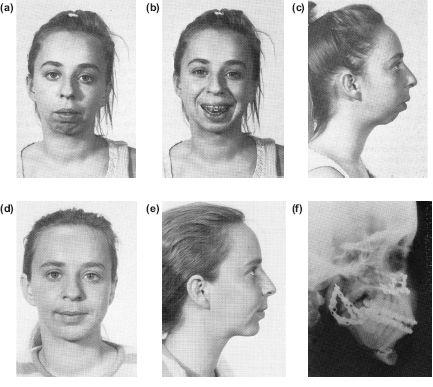
Figure 10.6 Marked retrognathia and an anterior open bite due to bilateral condylar damage in childhood (a), (b) and (c). Correction by a combination of a Le Fort I posterior impaction to close the open bite, and a bilateral inverted L advancement with interpositional bone grafts. The augmentation genioplasty was carried out simultaneously (d), (e) and (f).
Ankylosis only occurs when the meniscus is also displaced or destroyed, allowing the condyle to proliferate against the surface of the condylar fossa. In such cases the lack of function leads to a greater loss of mandibular development. The management of temporomandibular joint ankylosis will be discussed in Chapter 13.
Clinically there is an increased overjet which is usually exaggerated by the lower lip being trapped behind the upper incisors, increasing their proclination and spacing (Figure 10.7). Externally this is seen as an everted lower lip exaggerating the labiomental groove.
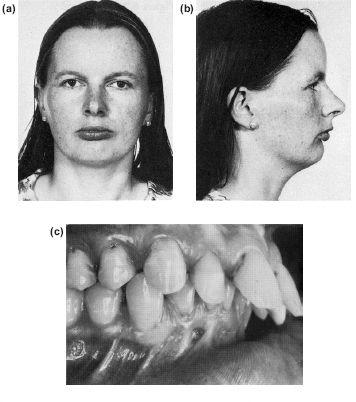
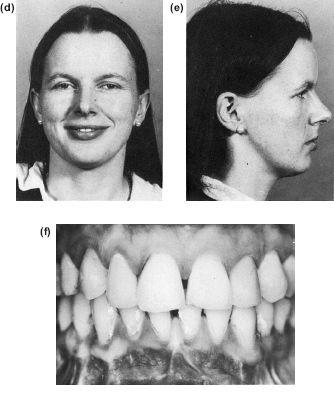
Figure 10.7 Surgical correction of mandibular retrognathism by a sagittal split advancement, after orthodontic incisor retroclination and levelling of the occlusal plane. Note to dramatic improvement of the lower lip contour as well as the skeletal profile. (a) to (c) Preoperative and preorthodontic therapy. (d) to (f) Postorthodontic therapy and surgery.
With unopposed occlusal drift (overeruption) of the lower incisors, the overbite is also increased.
The reduced lower facial height is a secondary aesthetic defect which may be self-correcting with the forward repositioning of the mandible.
A simple means of visualising the surgical correction is to study the face and profile before and after protruding the mandible. Before protrusion the chin will be set back and there will be a relatively low anterior facial height. With forward movement, not only does the profile improve but there is also an aesthetic gain from the increased lower facial height as the mandible moves downwards and forwards on the occlusal plane.
Treatment
The Occlusion
- As will be seen clinically and on the study models, the over erupted lower incisors will prevent the mandible being moved forward into a satisfactory relationship without a lateral open bite. In adults this lateral open bite will not be self-corrected by postoperative compensatory eruption of the molars and premolars. Some means of levelling the occlusal plane orthodontically pre-or postoperatively, or surgically will be necessary. Orthodontic depression of the incisors with the associated eruption of the posterior segments may not be possible to achieve preoperatively in adults without the lower incisors being proclined through the alveolar labial cortex.
The choices are:
a) Decompensation of the incisors and a forward osteotomy of the mandible to an overcorrected edge to edge incisor relationship, giving a three-point contact occlusion, i.e. incisors and distal molars, followed by orthodontic closure of the lateral open bites. However, this is only possible if there is sufficient interdental space in the buccal segments to allow the premolars and molars to erupt from the perimeter of a curve into the shorter horizontal straight line.
b) Separate orthodontic levelling of the canine and incisors, and the buccal segments. This will be followed by a lower anterior mandibulotomy setdown carried out at the same time as the mandibular lengthening procedure. This has the advantage of providing an additional supplement to the lower facial height. Figure 10.8 shows the increase in lower facial height and improved lip and chin profile after forward repositioning of the mandible with a lower incisor setdown achieved by an anterior mandibulotomy.
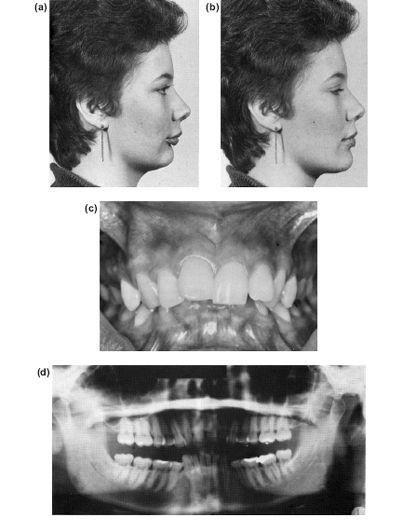
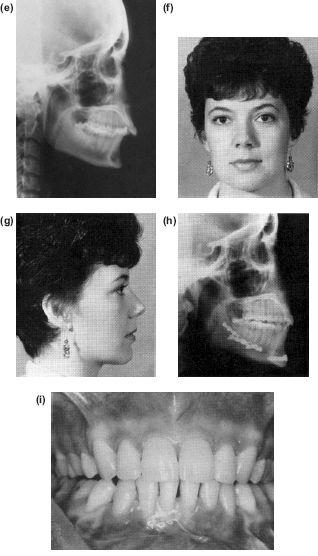

Figure 10.8 An anterior mandibulotomy combined with a forward osteotomy not only flattens the occlusal plane but also increases the chin depth. (a) Shows the preoperative profile in occlusion and (b) with the mandible postured forwards stimulating the surgical advancement. (c) to (e) The preoperative occlusion and radiographs before orthodontics and (f) after levelling the incisor and buccal segments independently. (g) to (k) Postoperative results. (k) The immediate postoperative orthopantomogram which shows the mandibulotomy cuts and set down.
In all cases, preoperative orthodontic decompensation, coordination of the arches and closure of any spaces, is essential preparation for surgery (Figure 10.7). This may reveal an unsatisfactory upper lip incisor relationship requiring a Le Fort I impaction.
Lengthening the Mandible and the Chin
Most marked Class II division 1 cases require not only a forward repositioning of the mandible to an overcorrected edge to edge incisor relationship by a sagittal split but also a sliding augmentation genioplasty. Always resist the temptation to wait and see if a genioplasty is also required — it is! (Figure 10.9).
The Chin
As described earlier there are aesthetic and ethnic variations in the profile. In most cases the chin point, i.e. the soft tissue pogonion (Pg), should lie within 6 mm of a vertical drawn downwards from subnasale at right angles to the Frankfort horizontal plane (Figure 10.10). Retrogenia is a receding chin and must be differentiated from the more common retrognathia, where the mandible is set too far back and is too short. The increased overjet of retrognathia is not usually found in pure retrogenia.
The chin depth (anterior inferior dentoalveolar height) from the incisor edge to the bony menton is 40 2 mm for women and 44 2 mm for men. This usually equals the distance of the lower lip margin to the soft tissue menton. Chin depth is often overlooked and may also require augmentation or reduction.
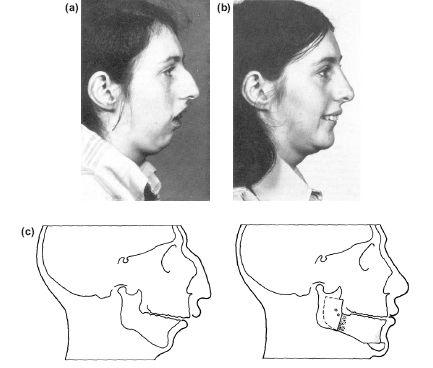
Figure 10.9 Severe “bird face” retrognathism corrected with a forward sagittal split osteotomy and genioplasty followed by a rhinoplasty. (a) Preoperative (b) postoperative, and (c) diagrammatic representation of change.
Unfortunately these estimations will be complicated by changes brought about by other osteotomies. For instance:
- after a Le Fort I elevation the chin will advance with the forward autorotation of the mandible, simultaneously reducing the apparent chin depth;
- forward movements of the mandible will have a predictable effect on the chin point (Po), but will simultaneously increase the lower facial height as the mandible moves down the occlusal plane;
- with backward correction of a prognathous mandible the distalisation of the chin is usually desirable, but occasionally it may require a paradoxical augmentation foreward slide;
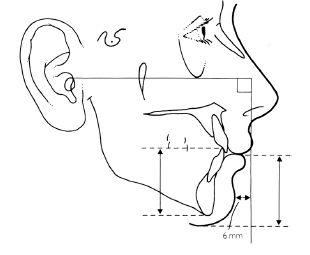
Figure 10.10 The vertical and horizontal parameters of the chin in relation to the vertical from the Frankfort mandibular plane (see text).
- bimaxillary osteotomies will also influence the chin profile if the occlusal plane is altered. By increasing the occlusal plane angle, the chin will rotate backwards and downwards. With a decreased occlusal plane, the chin will rotate forwards and become more prominent.
In all these cases a planning tracing on which the mandibular outline may be moved in the anticipated direction will enable the outcome to be predicted. Only in this way can any supplementary surgical addition or subtraction of the chin be confirmed.
Figure 10.11 shows the re/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


