Temporomandibular Disorders
•. Components of Temporomandibular Joint
•. Clinical Evaluation of Temporomandibular Joint
•. Clinical Evaluation of Muscles of Mastication and Accessory/Cervical Muscles
•. Disorders Associated with Deviation/Alteration in the Form of Articular Surfaces
Disk Displacement with Reduction
Disk Displacement without Reduction
Displacement of Disk–Condyle Complex (Hypermobility and Dislocation)
•. Inflammatory Joint Disorders
•. Degenerative Joint Diseases
•. Masticatory Muscle Disorders
•. Congenital, Developmental and Acquired Disorders of the TMJ
Components of Temporomandibular Joint
Mandibular Condyle
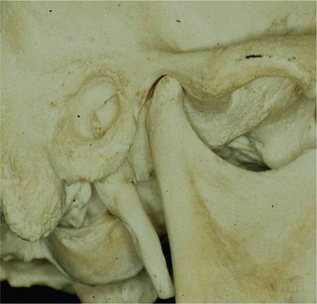
The condyle is elliptically shaped with its long axis oriented mediolaterally. The dimension of the condyle is roughly 20 mm in the mediolateral direction and approximately 8–10 mm in the anteroposterior direction. The articulating surface of the condylar head is covered by fibrocartilage (Figure 1).
Articular Capsule and Articular Disk
The articular capsule is a fibrous membrane that surrounds the joint and incorporates into the articular eminence. It attaches to the articular eminence, the articular disk and the neck of the mandibular condyle. Superiorly, it is attached to the temporal bone and inferiorly to the neck of the condyle. The anatomical and functional boundaries of the TMJ are defined by the articular capsule. The inner surface of the capsule is covered by the synovial membrane that aids in the secretion of the synovial fluid. The articular capsule confines the synovial fluid to the articulating surfaces. Temporomandibular ligaments provide additional reinforcement to the capsule on its lateral wall.
Articular disk is a biconcave oval structure with a thin intermediate zone and a thick posterior and anterior border. These thick posterior and anterior bands act as wedges, giving the disk a self-seating capacity with the condyle functioning against the intermediate zone. The importance of this feature cannot be overemphasized; the contour of the disk with the thick bands helps prevent the displacement of the disk from the condyle during translation. An absence of blood vessels and nerves in the intermediate zone of the disk enables this part of the disk to act as a pressure-bearing area (Figure 2).
Synovial Fluid
During movement, the synovial fluid held within the cartilage is squeezed out mechanically to maintain a layer of fluid on the cartilage surface (so-called weeping lubrication). Boundary lubrication is a function of water physically bound to the cartilaginous surface by a glycoprotein.
Ligaments Associated with Temporomandibular Joint
Accessory ligaments of TMJ include the stylomandibular and sphenomandibular ligaments.
Muscles of Mastication
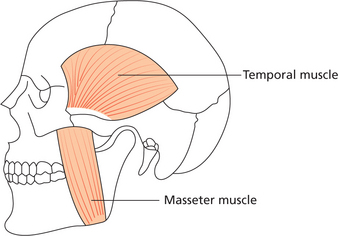
Masseter muscle
Masseter muscle arises from the lower border and inner surface of the anterior two-thirds of the zygomatic arch, passes inferiorly and posteriorly, and inserts on the outer surface of the mandibular ramus (Figure 3). The deep fibers of the masseter muscle (pars profunda) are vertically oriented whereas the superficial fibers (pars superficialis) are more oblique. This muscle is responsible for elevating the mandible to aid in jaw closure and for clenching and crushing action.
Temporalis muscle
The temporalis is a broad, fan-shaped muscle that arises from the temporal fossa (superior and inferior lines of the temporal bone). Via a strong tendon it inserts into the upper anterior border and the medial aspect of the coronoid process, and into the anterior border and adjacent medial surface of the mandibular ramus.
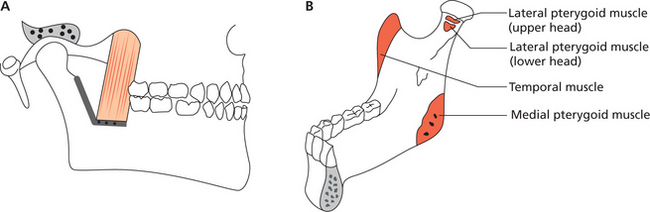
Medial pterygoid muscle
The medial pterygoid muscle originates from the pterygoid fossa (medial surface of the lateral pterygoid plate). Some of the fibers also originate from the maxillary tuberosity. The muscle fibers extend inferiorly, posteriorly and laterally to insert into the medial surface of the ramus, approximating the angle of the mandible. Here it joins with the masseter to form a muscle sling (Figure 4A, B).
Lateral pterygoid muscle
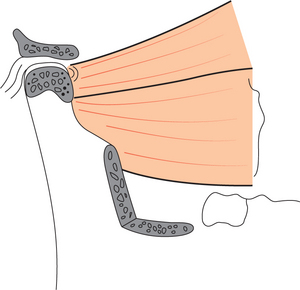
The lateral pterygoid muscle comprises two functionally distinct entities: (i) the smaller, superior head arises from the infratemporal surface of the greater wing of the sphenoid and runs backward in a nearly horizontal direction; (ii) the larger, inferior head arises from the lateral surface of the lateral pterygoid plate and runs backward in a somewhat oblique upward direction. Both heads merge posteriorly into a tendon that inserts in the following way: the upper fibers, which correspond more to the superior head, insert into the anterior surface of the capsule and disk; the inferior fibers, which correspond mainly to the inferior head, attach mostly to a depression (pterygoid fovea) on the inner side of the anterior surface of the mandible (Figure 5). Studies on the run and the attachment of the lateral pterygoid muscle on 41 cadavers by Abe et al (1993) showed the presence of a third intermediate belly of the lateral pterygoid muscle.
Both the heads of the lateral pterygoid muscle function as independent antagonistic muscles. Contraction of the inferior head pulls the condyle forward down the slope of the articular eminence (opening of the mandible and protrusion); whereas the superior head is active during mandibular closure and contracts in conjunction with the mandibular elevation muscles. It also exerts a holding or bracing action on the condyle when the teeth are held together and during power strokes. The superior head also acts to rotate the disk anteriorly on the condyle when the disk–condyle complex is moving upward and backward against the eminence. By keeping the disk between the condyle and eminence, the superior head of the lateral pterygoid muscle aids in maintaining joint stability.
Clinical Evaluation of Temporomandibular Joint
Examination of Temporomandibular Joint
The TMJ is examined by a thorough inspection, palpation, and auscultation.
The face is inspected for any obvious asymmetry, scars (may be indicative of previous surgeries, trauma), swelling/ulceration/sinus openings in the pre-auricular region. Observe for deviation/deflection (Figure 6) of mandible on mouth opening.

Figure 6 Deflection of the mandible to the left side. Courtesy: Department of Oral Medicine and Radiology, Manipal College of Dental Sciences, Mangalore
The TMJs can be palpated by extra-auricular and intra-auricular methods. Palpation can be done standing at 10 o’clock or 11 o’clock positions by the clinician. Intra-auricular palpation can be achieved by placing the little finger inside the external auditory meatus. During mandibular movement the posterior poles of the condylar head can be palpated with the pulp of the little finger. Intra-auricular palpation may also be used to elicit capsular tenderness.
Clinical Evaluation of Muscles of Mastication and Accessory/Cervical Muscles
Pterygoids
Palpation of the pterygoid muscle is difficult because of the inaccessibility of the muscle.
Lateral pterygoid
Tenderness of the lateral pterygoid can occasionally be detected by indirect application of pressure. The index finger or back end of the handle of an instrument is positioned distal and posterior to the maxillary tuberosity and posterior pressure is exerted to compress tissue against the muscle (Figure 7).

Figure 7 Use of the back end of a mouth mirror to elicit tenderness at the site of the attachment of the lateral pterygoid muscle
Alternatively, the medial and lateral pterygoid muscles can be assessed by functional evaluation. These can be achieved by asking the patient to perform simple tasks like opening the mouth against resistance (Figure 8) and closing the mouth against resistance.
Cervical Examination
Sternocleidomastoid
Palpation is done bilaterally near its insertion on the outer surface of the mastoid fossa behind the ear. The entire length of the muscle is palpated down to its origin near the clavicle.
Posterior cervical muscles
Trapezius, longissimus (capitis and cervices) splenius (capitis and cervices) and levator scapulae.
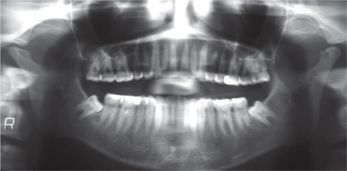
Occlusal Evaluation
Examining the dentition and occlusion is an important part of the physical examination of a TMJ disorder or orofacial pain patient. It may provide very useful information about the existence of bruxism or other oral habits and their possible effects on the dentition, periodontium or other oral structures. Such an examination can also determine whether there has been a progressive change in the occlusal relationship (midline shift, anterior open bite, unilateral posterior open bite, etc.) that may indicate the presence of such conditions as unilateral condylar hyperplasia, rheumatoid arthritis, or neoplasm. Noting the number of missing teeth particularly loss of posterior occlusal support is important since this situation may predispose the TMJs to degenerative joint disease (osteoarthrosis) especially in the presence of bruxism.
Imaging Protocol
Decision should be taken considering the following:
These depict the osseous structures of the joint with varying degrees of bony detail.
Disorders of TMJ
TMJ disorders may arise from macro trauma such as in road traffic accident (RTA), excessive mouth opening (yawning, biting onto a large chunk of food) or from repeated micro trauma such as in parafunctional habits (bruxism), uneven occlusal loading (malocclusion, high points in restorations, poorly contoured crowns). Other causes include stress, underlying systemic diseases, arthritis and developmental abnormalities. See Box 1 for classification of TMJ disorders.
Disorders Associated With Deviation/Alteration in the Form of Articular Surfaces
Changes associated with the articular surfaces include those of the mandibular condyle and glenoid fossa. The changes that can be appreciated are condylar head flattening (Figure 9), flattening of the glenoid fossa or bony irregularities over the condylar head.
Articular Disk Defects
Disk Thinning and Perforation
Clinical features
Cholitgul et al (1990) evaluated 15 patients who were reported to have disk perforation at arthrography. Eleven patients reported pain. Clicking and crepitation was common. Deviation of the mandible at maximum mouth opening toward the affected side was seen in nine patients. The muscles of the affected side were tender on palpation. The disk perforation was located in the posterior attachment in most joints. An anterior disk displacement was found in almost all patients. They concluded that most joints with disk perforations were osteoarthrotic and the most severe clinical and radiological findings are associated with an ant/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses