Posterior Composite Restorations
Direct or Indirect Technique?
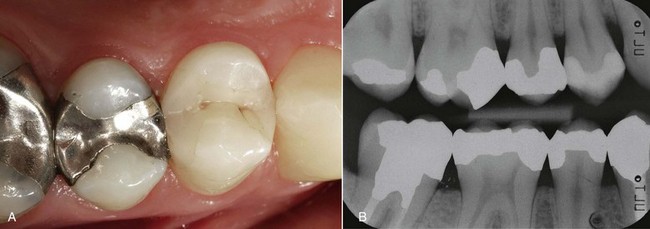
Improved enamel-dentin adhesives, combined with less polymerization shrinkage, deliver good marginal quality that is stable over time, significantly reducing microleakage (Perdigão and colleagues, 2000; Lopes and colleagues, 2002) (Figure 10-1).
Better physical and chemical properties and enhanced polymerization of materials have greatly increased wear resistance (Spreafico and Roulet, 2009), and the problem finally seems to have been solved, at least for medium-sized restorations (Ferracane, 2006).
The result of these improvements is restorations that boast excellent longevity (van Dijken, 2000; Pallesen and Qvist, 2003; Pallesen, 2005; Opdam and colleagues, 2007) (Figure 10-2).
However, optimal proximal and occlusal anatomy and defect-free margins are difficult to achieve, especially when dealing with large cavities and areas that are difficult to access. Adhesives inlays have shown better behavior than direct restorations in complex cavities with cervical margins close to or extending beyond the cemento-enamel junction (Krejci, 1992; Roulet, Gotz, and Losche, 1993; Dietschi and Herzfeld, 1998). The main goals of restorative dentistry are as follows:
• Anatomic and functional restoration of removed or missing tissues
• Guarantee of esthetically pleasing results
These objectives, which are crucial for long-term clinical success, can be achieved with different types of treatment, and the materials can be applied with various techniques (Figure 10-3).
Composite resins can be applied to posterior teeth using different techniques (Dietschi and Spreafico, 1997), as follows:
The direct and indirect techniques are the ones that are used most often.
Direct Technique
Cavity margins are finished with fine-grain diamond burs (30 to 40 microns). The aim here is to smooth the cavity margins and remove unsupported enamel prisms. The importance of preparing chamfered margins is still subject to debate. Chamfering is designed to expose the upper surface of enamel prisms and increase the bonding surface, thereby improving adhesion values (Porte and colleagues, 1984). Consequently, chamfering promotes better marginal quality (Han, Okamoto, and Iwaku, 1992; Schmidlin and colleagues, 2007).
However, in a 5-year in vivo study Wilson and colleagues (1991) demonstrated that chamfering does not increase the quality of margins.
However, in order to place the matrices easily and prevent distortion, clear proximal, cervical, buccal, and lingual separations are required (Spreafico and Roulet, 2005).
Composite Layering
Lutz and Kull (1980) were the first to demonstrate the good marginal adaptation of layered composite restorations in vitro. It should be noted that effective dentinal adhesives were not available at the time, and that composites were subject to greater polymerization shrinkage than current materials.
Through in vitro experiments several authors later demonstrated the effectiveness of layering in controlling polymerization stress (Lutz, Krejci, and Luescher, 1986; Lutz, Krejci, and Oldenburg, 1986; Tjan, Bergh, and Lidner, 1992; Park and colleagues, 2008).
Nevertheless, based on a comparison of the bulk technique and multilayered techniques, not all authors believe that layering can produce satisfactory margin quality (Versluis and colleagues, 1996; Jedrychowski, Bleier, and Caputo, 1998; Kuijs and colleagues, 2003).
In any case, in order to obtain adequate polymerization, the thickness of the material should not exceed 2 mm, even when high-intensity irradiation lamps are employed (Rueggeberg, Ergle, and Mettenburg, 2000). Therefore the composite must be layered (the number of increments will depend on the size of the cavity) using a thickness of 2 mm as a benchmark.
There are different layering techniques—horizontal, oblique, and vertical—but to date it is still unclear which one is the best (Ferracane, 2008).
It must be noted that the use of flowable composite is controversial. In an in vitro study on Class V cavities, Kemp-Scholte and Davidson (1990) showed that an intermediate elastic layer placed between the bonding agent and the restoration decreased stress by 20% to 50% while preserving marginal integrity.
Many professionals have investigated this over the years, but no unequivocal conclusions have been reached. Some have shown that a layer of flowable composite improves marginal adaptation (Attar, Turgut, and Gungor, 2004; Li and colleagues, 2004, 2006), whereas others have found no improvement (Braga, Hilton, and Ferracane, 2003; Lindberg, van Dijken, and Horstedt, 2005). At the same time, however, no one has ever shown that the quality of restoration deteriorates. In my clinical experience, the use of flowable composite reduces postoperative sensitivity to practically zero.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses