Occlusal Aspects in Restorative Dentistry
Overview
When examining occlusal problems, one must deal with two aspects: anatomic ones and functional ones (Figure 16-1).
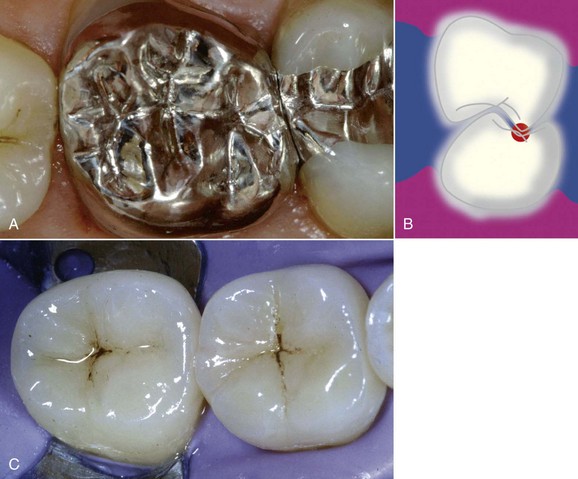
Figure 16-1 Anatomic and functional aspects of occlusion.
Anatomic aspects
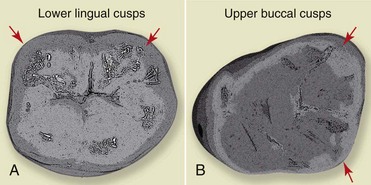
The cusps of the teeth can be distinguished as supporting (or centric) cusps, which are the buccal cusps of the lower teeth and the palatal cusps of the upper teeth, and nonsupporting cusps, which are the lower lingual and the upper buccal cusps (Figures 16-2 and 16-3).
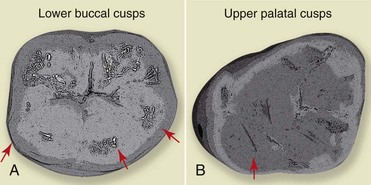
Figure 16-2 Supporting cusps: A, lower arch; B, upper arch.
Occlusal Relationships
Mandibular Movements
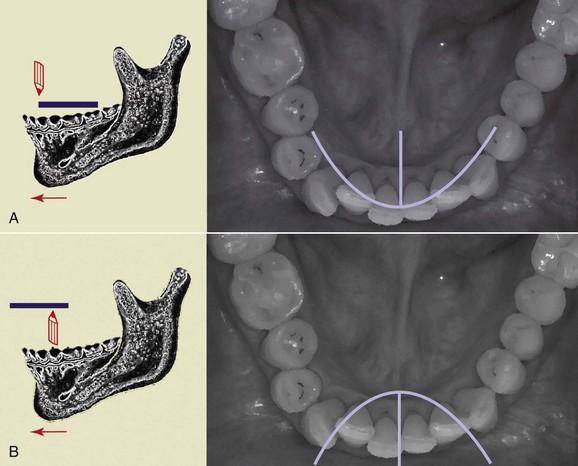
The lines traced by performing both left and right lateral movements and the protrusive movement form what is called a “Gothic arch” (Figure 16-5, A). The starting point is the CR. Instead, if the stylus is placed on the lower arch, and the plate on the upper arch, this yields an inverted curve that forms a “gull-wing pattern” (Figure 16-5, B).
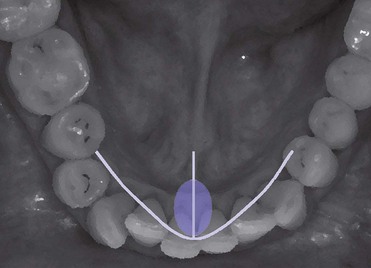
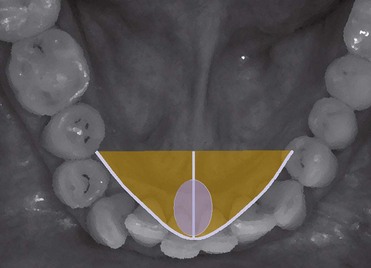
In the Gothic arch we can distinguish a functional area (Figure 16-6), which coincides with the movements performed most frequently by the patient during the day (such as eating or talking), and the total movement area (Figure 16-7), represented by the area covered by larger movements, which are conditioned and limited by bone structures, tendons, and muscles—hence the definition of border movements of the mandible.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses