Chapter 10
Paramedian forehead flap
Introduction
The paramedian forehead flap may be one of the oldest flaps in use for the reconstruction of facial defects. Its use in nasal reconstruction dates as far back as 1500 BC as it was used to reconstruct nasal amputation defects.1,2 The classic Indian forehead flap became popular in the United States when Blair3 in 1925 and Kazanjian4 in 1946 described the median forehead flap for nasal repair. Several years later, Millard revised the flap by narrowing the base and rendering the perfusion based solely on the supratrochlear vessels.5 The modification allowed for an increase in the length of the flap to be harvested and ease of rotation of the flap due to the narrower pedicle width. The modification increased the reliability of the flap by diminishing the torsion on the vessels and therefore allowing for better perfusion and diminished likelihood of congestion.6
The main use of the paramedian forehead flap has been in the reconstruction of partial to total nasal defects. Its use is not limited to nasal reconstruction; the flap may be used to reconstruct any defect within the reach of its arc of rotation. This fact allows for its use in reconstructing defects in the forehead, and the periorbital region.
The main advantages of this flap rest on its texture, thickness, and color match to the surrounding skin, making it an indispensable option in reconstructing a vast range of nasal defects.
The drawback of the paramedian forehead flap is the need for multiple stage surgery. Typical use requires first a transfer then sectioning of the pedicle and inset of the flap several weeks later. In order to keep the positives of this flap while removing the main drawback, some authors have advocated its use as a single stage flap.7,8
Anatomy
The anatomy of the forehead is relatively simple in terms of tissue composition. The layers of the forehead consist of the skin, the subcutaneous skin, the frontalis muscle, areolar tissue, and the pericranium. The skin of the forehead region is of similar color, texture, and thickness to many of the surrounding areas within the reach of the paramedian forehead flap.
The vascular supply to the forehead comes from the paired supraorbital arteries, which divide into a superficial and a deep branch, and the paired supratrochlear arteries. Both the supraorbital and the supratrochlear arteries are branches of the ophthalmic artery, which in turn is a branch of the internal carotid artery. The glabellar region of the forehead also receives terminal branches from the angular artery, which is a branch from the facial artery. The latter is a branch from the external carotid artery. The forehead region in fact receives its arterial supply from both the internal and external carotid system. The venous drainage of the forehead region is carried out by the accompanying venae comitantes of the supraorbital and supratrochlear vessels. The sensory innervation of the forehead is by the supraorbital nerve and the supratrochlear nerve, while the motor innervation to the frontalis muscle comes from the frontal branch of the facial nerve.
The blood supply of the paramedian forehead flap is based on the supratrochlear artery and vein as its axial and random blood supply from the anastomosing vessels from the terminal branches of the angular artery and the contralateral. The artery can be located as it emerges from the foramen and travels in a cephalad direction in the forehead region between the medial brow and the lateral aspect of the nasal dorsum. The path of the artery and the venae commitantes is in a more or less vertical direction, thus resulting in an axial flap.
In the caudal aspect, as the artery begins its cephalad travel, it is located above the pericranium. As it travels, it migrates towards the subcutaneous plane. In the forehead region near the hair line, the vessel branches are found in the subcutaneous plane.
The frontalis muscle is found in the location of this flap, especially at the most superior portion of the flap.
Flap harvest
First stage
- The path of the supratrochlear artery is marked as it travels in a cephalad direction in the forehead.
- The size of the defect to be transferred is measured and the location of the defect is noted.
- The outline of the defect can be retraced with a marking pen. Using a small piece of paper from the surgical glove packing, the imprint of the defect is picked up onto the paper by pressing down over the marking.
- The template is trimmed and transferred to a good position on the forehead.
- With a suture string, a pivot point along the brow is marked and the string is then rotated to the most inferior point of the defect.
- The string is then rotated along this pivot point to the forehead and the point is marked. This will be the most cephalad portion of the flap.
- The defect shape is then transferred to the forehead, taking care to center it along the axial path of the artery.
- The elevation of the flap is begun on the most superior portion of the flap and is extended to a depth superior to the frontalis muscle.
- The incision is made along the marked flap and dissection is carried out in a caudal direction towards the nasal bridge and medial canthus along the main axial direction of the artery.
- The depth of the dissection is extended to the subperiosteal layer about 3 cm superior to the brow region. This depth offers a layer of protection to the vascular pedicle.
- Once the dissection nears the brow region, care should be taken not to injure the main pedicle.
- The medial portion of the pedicle should be extended in a curvilinear fashion towards the medial canthus, leaving at least a 1 cm bridge of skin overlying the vascular pedicle.
- The dissection in the brow region should be made with care not only to maintain the integrity of the vascular pedicle but also to release the periostium in this area, therefore aiding rotation of the flap to reach the defect site passively.
- Once the flap dissection is completed, the rotation and reach of the flap is assured to be in a passive fashion. The flap may be thinned if the defect warrants it.
- If thinning is needed, this is carried out using thernotomy scissors only in the area of the flap to be inset into the recipient site.
- The flap is inset in the recipient site from the most caudal area to the most cephalad region. The most superior portion of the flap will not be sutured into the defect because of the axial extension of the skin and vascular pedicle. The area is, however, in tight contact to the underlying defect site.
- The forehead defect is undermined widely and advanced towards the midline.
- The closure of the defect is begun from the inferior aspect and extended in a superior direction. In cases where primary closure is not possible, the area is then left to heal in a secondary intention.
- See Figures 10.1 to 10.13.
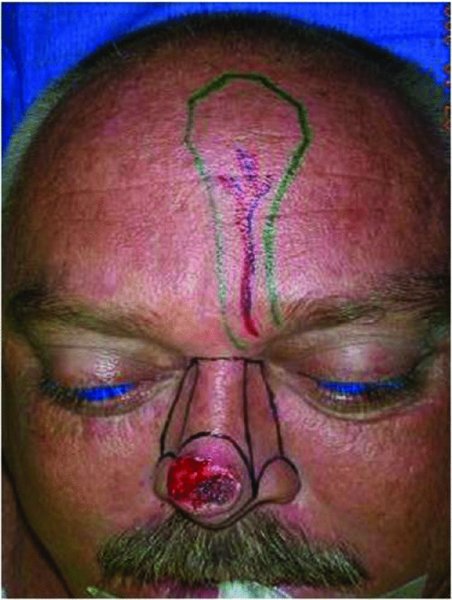
Figure 10.1 Markings for the resection of the nasal lesion and reconstruction of the planned defect with a paramedian forehead flap.
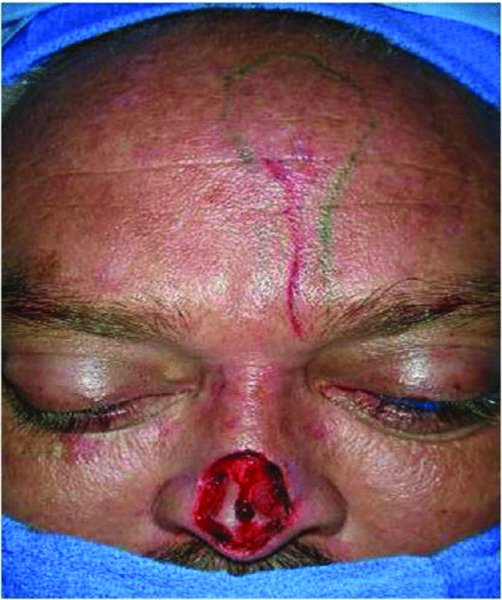
Figure 10.2 View of the defect after resection of the nasal lesion.
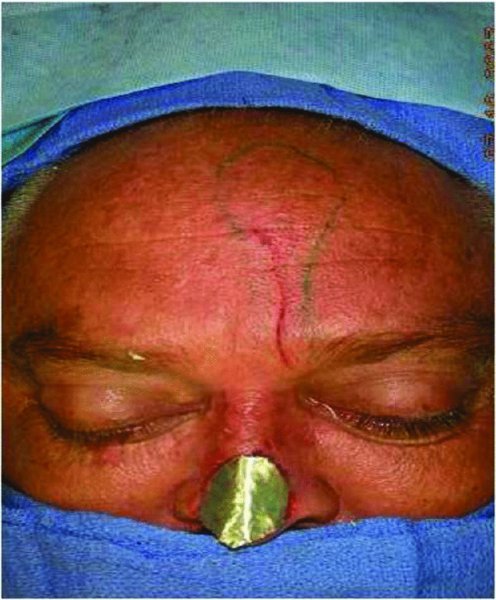
Figure 10.3 Assessment of the donor site defect to be used as a template for the reconstruction.
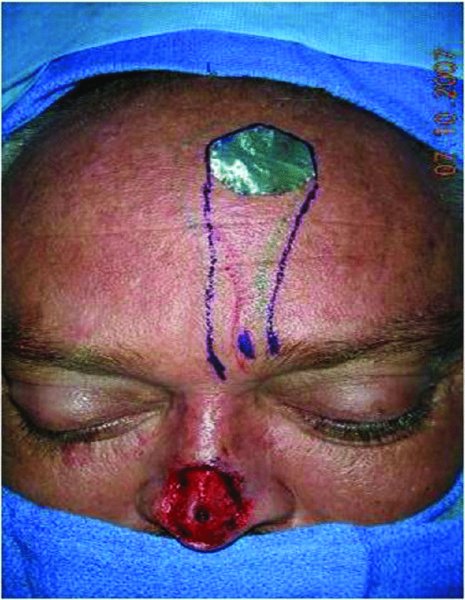
Figure 10.4 Transfer of the template to the forehead.
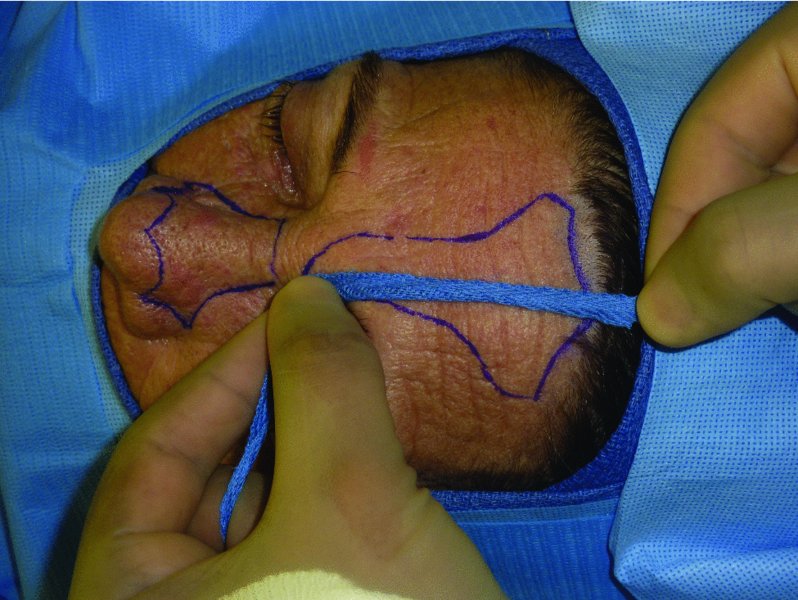
Figure 10.5 Measurement of the flap to confirm reach of the flap to the defect site.
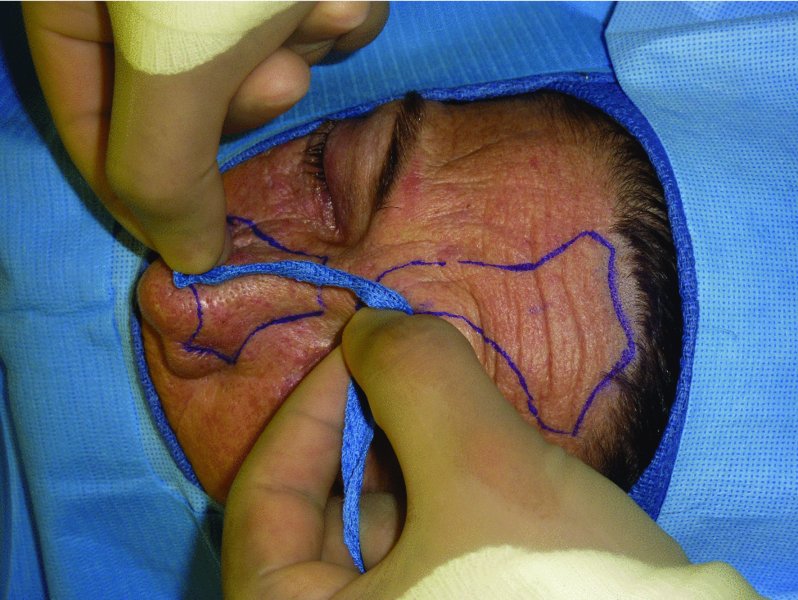
Figure 10.6 Rotation of the measurement to the planned defect from the pivot point.

Figure 10.7 Nasal defect prior to the reconstruction.

Figure 10.8 Elevation of the flap prior to transfer to the nasal defect.

Figure 10.9 Elevated flap. Note that the depth is changed to a subperiosteal plane in the region of the brow.

Figure 10.10 Assessment of the reach of the flap to the defect./>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


