10
Orthognathic Surgery
Introduction
A combined orthodontic–surgical or orthognathic approach is often indicated to address malocclusion with a significant skeletal aetiology. Collectively, these procedures have broadened the scope of orthodontic correction. It is clear that interceptive orthodontic treatment has only a minor influence on skeletal growth and in the presence of a significant skeletal discrepancy, either camouflage or orthognathic treatment is often required to obtain a class I occlusion. With the introduction of the mandibular sagittal split osteotomy and later the maxillary Le Fort 1 osteotomy, clinicians have the means to fully correct a range of skeletal discrepancies (Trauner and Obwegeser, 1957; Obwegeser, 1969). Since then, numerous other surgical techniques and variations have been described, which allow the orthodontist and surgeon to address a wide range of antero-posterior, vertical and transverse skeletal discrepancies, including asymmetry. The development and evolution of orthognathic surgery has coincided with a paradigm shift in orthodontics, away from occlusal and hard tissue-based treatment planning to soft tissue and facial treatment planning (Ackerman et al., 1999). With modern techniques, comprehensive treatment today should aim to improve not only the patient’s dental aesthetics and occlusion, but also their facial aesthetics.
Indications for orthognathic surgery include cases where a significant skeletal discrepancy and orthodontic camouflage may be detrimental to facial aesthetics; where an ideal or acceptable occlusal result simply cannot be achieved with orthodontics in isolation; or where there is a desire for facial change. It is also indicated for the group of patients who present at the extremes of malocclusion, associated with a cranio-facial syndrome where the main aim of treatment is the improvement and normalization of facial appearance.
With experience, better understanding of aesthetics and more sophisticated planning, outcomes are becoming more predictable (Arnett and Gunson, 2004; 2010). There is less morbidity and inpatient stays are shorter; inter-maxillary fixation has also been largely superseded by rigid internal fixation, which permits an earlier return of masticatory function. Levels of satisfaction with orthognathic procedures are also generally very good, with significant improvement in oral health-related quality of life (Cunningham et al., 1995; 1996; 2003). Combined, these factors mean that in the last few decades, while it still remains highly specialized work that requires close collaboration between orthodontist and maxillofacial surgeon, it has become part of routine practice, allowing comprehensive treatment of skeletal problems that previously had been beyond the scope of orthodontics.
Case 10.1
| Extra-oral | |
| Skeletal relationship | |
| Antero-posterior | Moderate skeletal class II |
| Vertical | FMPA: Average |
| Lower face height: Average | |
| Transverse | Facial asymmetry: Chin point to the right |
| Soft tissues | Lip competence: Incompetent with lower lip acting behind maxillary incisors |
| Naso-labial angle: Average | |
| Upper incisor show | At rest: 3 mm |
| Smiling: 7 mm | |
| Temporo-mandibular joint | Healthy with good range and co-ordination of movement |
| Intra-oral | |
| Teeth present |  |
| Dental health | Good |
| (restorations, caries) | No restorations or active caries |
| Oral hygiene – periodontal Good | |
| Lower arch | Crowding: Mild |
| Incisor inclination: Average | |
| Curve of Spee: Average | |
| Upper arch | Crowding: Mild |
| Incisor inclination: Proclined | |
| Canine position: Line of the arch | |
| Occlusion | Incisor relationship: Class II division 1 |
| Overjet: 9 mm | |
| Overbite: Average and complete | |
| Molar relationship: Class II bilaterally | |
| Canine relationship: Class II bilaterally | |
| Centre lines: Lower to the right by 2 mm | |
| Functional occlusion: Group function | |
Summary
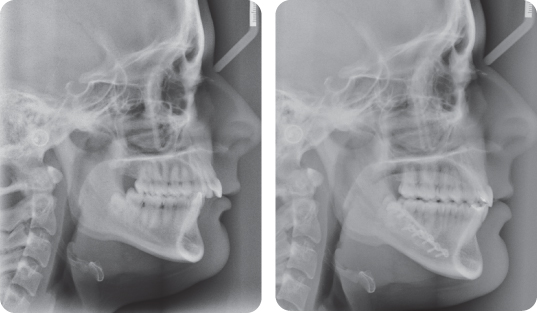
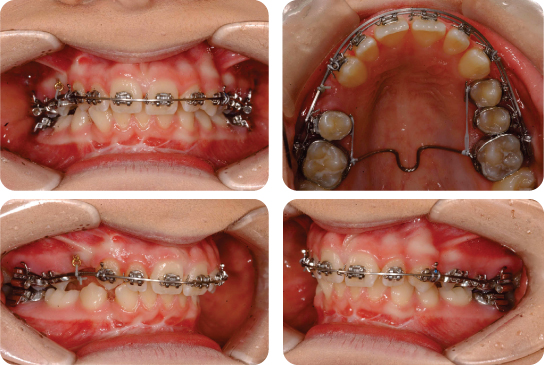
A 26-year-old female presented with a class II division 1 malocclusion on a moderate skeletal class II pattern with average vertical dimensions complicated by an increased overjet (9 mm), mild crowding of both dental arches and a chin point displaced to the right along with the dental centre line (Figure 10.1).
Treatment Plan
- Upper and lower pre-adjusted edgewise appliances on a non-extraction basis
- Bilateral sagittal split osteotomy to advance the mandible
- Long-term retention (the final result is shown in Figures 10.2 and 10.3)
What Were the Main Options for Treatment?
There were three main treatment options in this case:
- Alignment of the dental arches on a non-extraction basis. This would have resulted in a residual overjet and would necessitate permanent fixed retention in both arches, as the upper incisors would be unsupported by the mandibular anterior segment in occlusion.
- Orthodontic camouflage with removal of two maxillary first premolars. With anchorage reinforcement, this approach may have successfully reduced the overjet and produced ideal arch alignment. However, occlusal improvement may have been accompanied by unfavourable soft tissue effects, including retraction and thinning of the upper lip.
- Combined orthodontic–surgical approach. This modality would facilitate overjet reduction by correction of the antero-posterior skeletal discrepancy with mandibular advancement surgery. It would also be the only treatment strategy capable of correcting the mandibular chin point asymmetry.
What Was the Role of the Orthodontic Treatment in This Case?
- Decompensate and co-ordinate the dental arches
- Facilitate surgical advancement of the mandible
- Finish and detail the occlusion
Why Was Inter-Proximal Reduction Undertaken on the Mandibular Incisors?
This was undertaken to provide some space for alignment whilst maintaining their inclination and therefore facilitating mandibular advancement. The chin point and centre line discrepancy would be corrected with the mandibular surgery.
Why Were Mandibular Premolars Not Extracted?
Space requirements were not high in the mandibular arch and the extraction of premolar teeth might have led to an inappropriate increase in the overjet during space closure. Too great an overjet would lead to further advancement of the mandible, which can be less stable and might also result in too prognathic an appearance post-surgery; particularly in this case, as the chin point is already quite strong.
How Might the Final Result Have Differed If This Patient Had Been Treated With Orthodontic Camouflage?
- Clear skeletal effects are induced by surgery with increased mandibular length and anterior repositioning of pogonion (Mihalik et al., 2003).
- The dental effects would have differed significantly, with optimal inclination of the maxillary and mandibular incisors being maintained with combined treatment. Orthodontic camouflage would have necessitated dental inclination changes to camouflage for the underlying skeletal discrepancy.
- The lower facial profile would not have been enhanced with camouflage treatment.
- The mandibular asymmetry required surgery for correction.
If Orthodontic Camouflage Were Undertaken, How Much Upper Lip Retraction Would Be Likely to Occur?
Soft tissue changes are unpredictable, being governed by soft tissue tonicity, lip competence, racial characteristics and overall fullness of the soft tissues (Ramos et al., 2005). A recent study suggests that soft tissue retraction is approximately 40% of incisor retraction (Scott Conley and Jernigan, 2006). Consequently, a 5-mm reduction in overjet may be expected to translate into 2 mm of lip retraction.
Case 10.2
| Extra-oral | |
| Skeletal relationship | |
| Antero-posterior | Mild skeletal class II |
| Vertical: | FMPA: Increased |
| Lower face height: Increased | |
| Transverse | Mandibular asymmetry with deviation of chin point to the right side |
| Soft tissues | Lip competence: Incompetent |
| Naso-labial angle: Normal | |
| Upper incisor show | At rest: 1 mm |
| Smiling: 6 mm | |
| Temporo-mandibular joint | Healthy with good range and co-ordination of movement |
| Intra-oral | |
| Teeth present |  |
| Dental health (restorations, caries) | Good |
| Oral hygiene – periodontal | Good |
| Occlusion | Incisor relationship: Class II division 1 |
| Overjet: 5 mm | |
| Overbite: Reduced with an anterior open bite of 12 mm | |
| Molar relationship: Class I bilaterally | |
| Canine relationship: Class I bilaterally | |
| Centre lines: | |
| Upper centre line is correct to mid-facial plane | |
| Mandibular centre line is deviated 4 mm to right side | |
| Functional occlusion: Group function | |
| Upper arch | Crowding: Moderate |
| Incisor inclination: Proclined | |
| Canine position: Line of arch | |
| Lower arch | Crowding: Mild |
| Incisor inclination: Retroclined | |
Summary
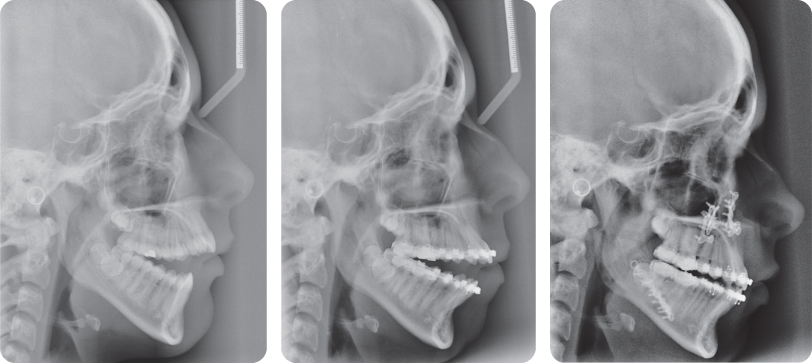
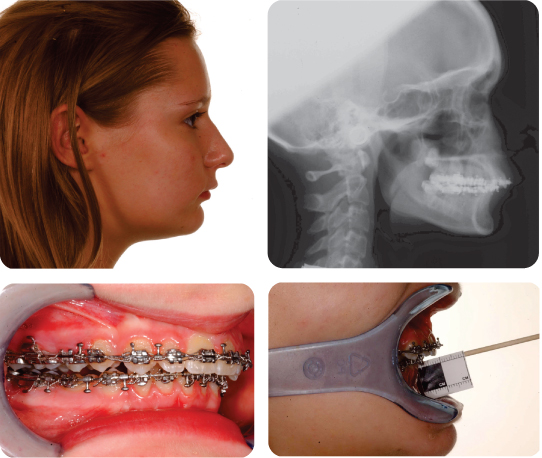
A 17-year-old female presented with a class II division 1 malocclusion on a skeletal class II base with increased vertical dimensions and a mandibular asymmetry, further complicated by a large anterior open bite (12 mm) and crowding of both dental arches (Figure 10.4).
Treatment Plan
- Upper and lower pre-adjusted edgewise appliances on a non-extraction basis
- Bi-maxillary surgery
- Long-term retention
The final occlusion is shown in Figures 10.5 and 10.6.
What Are the Causes of Anterior Open Bite?
Anterior open bites may occur for the following reasons:
- Transitional, as the permanent incisors are erupting.
- Due to local factors:
- A prolonged digit sucking habit may impede incisor eruption and procline the maxillary incisors
- Local pathology interfering with normal incisor eruption.
- Skeletal open bites: Caused by an imbalance between vertical growth of the anterior and posterior face. The Frankfort-mandibular plane angle (FMPA) and lower anterior face height are usually increased. This pattern is typically seen with a posterior mandibular rotation during growth. Skeletal open bites have a poor prognosis for orthodontic correction.
- Soft tissue abnormalities: Resting tongue position may contribute to anterior open bites with the tongue lying on the incisal edges of the incisor teeth, limiting vertical development. However, although this appearance may be seen in many cases, it may also occur as an adaptation to an underlying skeletal abnormality. Rarely, aberrant tongue behaviour, including endogenous tongue thrusting may contribute to anterior open bite.
How Stable Is the Correction of Open Bite?
Unless an obvious habitual cause is present (e.g. digit sucking) the correction of anterior open bite is inherently unstable, irrespective of the treatment modality. In a 10-year follow-up after orthodontic correction, 35% of subjects had a vertical gap between the incisal edges of the mandibular incisors and the palatal surfaces of the maxillary incisors of 3 mm or more (Lopez-Gavito et al., 1985). However, more prolonged follow-up suggests that a slight increase in overbite may occur during the post-retention phase, up to 15 years following appliance removal (Zuroff et al., 2010). There is also evidence of greater stability of open bite correction when orthodontic treatment is undertaken with extractions (Janson et al., 2006).
Similar levels of stability have been attributed to combined orthodontic –surgical treatment, involving superior repositioning of the maxilla (Denison et al., 1989; Swinnen et al., 2001). A key predictor of open bite recurrence appears to be the presence of frank open bite pre-treatment, with 43% developing open bite in the follow-up period (Denison et al., 1989). Conversely, those with incisal contact pre-treatment demonstrated higher levels of stability.
What Were the Aims of Pre-Surgical Orthodontics in This Case?
- Maintain optimal inclination of the maxillary incisors to compensate for their uprighting following a posterior maxillary impaction (therefore, the orthodontist will procline these teeth prior to the surgery)
- Arch alignment
- Transverse arch co-ordination
How Can Maxillary Incisor Proclination Be Achieved?
- Avoidance of maxillary arch extractions
- Bracket prescription: High torque variants, e.g. MBT and increased mesial tip in the maxillary canine brackets
- Class III inter-maxillary traction
- Supplementation of maxillary incisor palatal root torque prescription with third-order archwire bends
Why Was a Posterior Maxillary Impaction Employed in This Case?
Posterior impaction of the maxilla allows a counter-clockwise (upward and forward) rotation of the mandible and a reduction of the anterior open bite as the lower incisors move upward.
Why Was a Forward Mandibular Osteotomy Required As Well (Figure 10.6)?
This was required because the degree of auto-rotation following posterior maxillary osteotomy was not enough to produce a class I incisor relationship. The residual overjet was corrected with the mandibular osteotomy.
Could Mandibular Surgery in Isolation (With a Counter-Clockwise Mandibular Rotation) Have Been Used to Address the Anterior Open Bite?
Traditionally, counter-clockwise mandibular rotation in isolation to correct anterior open bites has been avoided. Pitfalls with this approach include inadvertent stretching of the pterygo-masseteric muscular sling. Following surgery, the mandibular closing muscles shorten, producing an opening mandibular rotation, which results in recurrence of the malocclusion (Iannetti et al., 2007). Although recent research has demonstrated some encouraging results with this approach (Stansbury et al., 2010), the degree of rotation required in this case would have been excessive and unlikely to produce prolonged stability.
Case 10.3
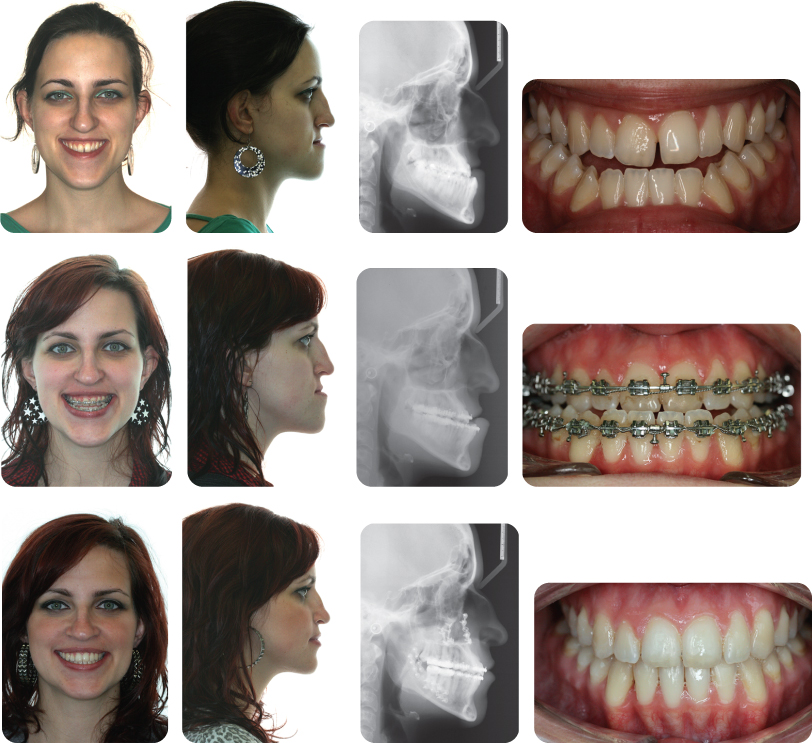
What Are the Main Features of This Malocclusion (Figure 10.7)?
- Class III malocclusion on a severe skeletal class III base with increased lower face height. The skeletal class III relationship has arisen because of maxillary deficiency and mandibular excess combined with increased vertical proportions.
- Class III incisor relationship with a reverse overjet, an openbite tendency, bilateral posterior crossbite and a centre line discrepancy.
- Slight gingival excess on smiling.
This Patient Underwent a Bi-Maxillary Osteotomy to Correct Her Malocclusion (Figure 10.7). What Are the Likely Jaw Movements Required to Achieve This?
In order to correct the open bite, the maxilla was impacted posteriorly; however, this was also accompanied by some anterior impaction to reduce gingival show and improve the aesthetics of the upper incisors. The maxilla was also moved forwards because of the underlying antero-posterior maxillary deficiency and an accompanying backward positioning sagittal split osteotomy of the mandible was carried out.
Why Has the Patient’s Profile Worsened Prior to Surgery?
This is because orthodontic decompensation has been carried out. The upper incisors have been retroclined and the lower incisors proclined, with a resulting increase in the reverse overjet and worsening of the profile.
The Appearance of the Patient 12 Months After Removal of Her Fixed Appliances Is Shown in Figure 10.8. What Is the Likelihood of Continued Stability of the Surgical Correction?
The surgical movements in this case are regarded as being stable over a 12-month period (little or no change in around 80% of patients). Beyond 12 months, maxillary superior movements are likely to relapse by more than 2 mm in around one-third of patients; however, these changes are not necessarily accompanied by significant changes in overjet or overbite. For bi-maxillary cases, class III correction is more stable than class II (Proffit et al., 1996; 2007).
Case 10.4
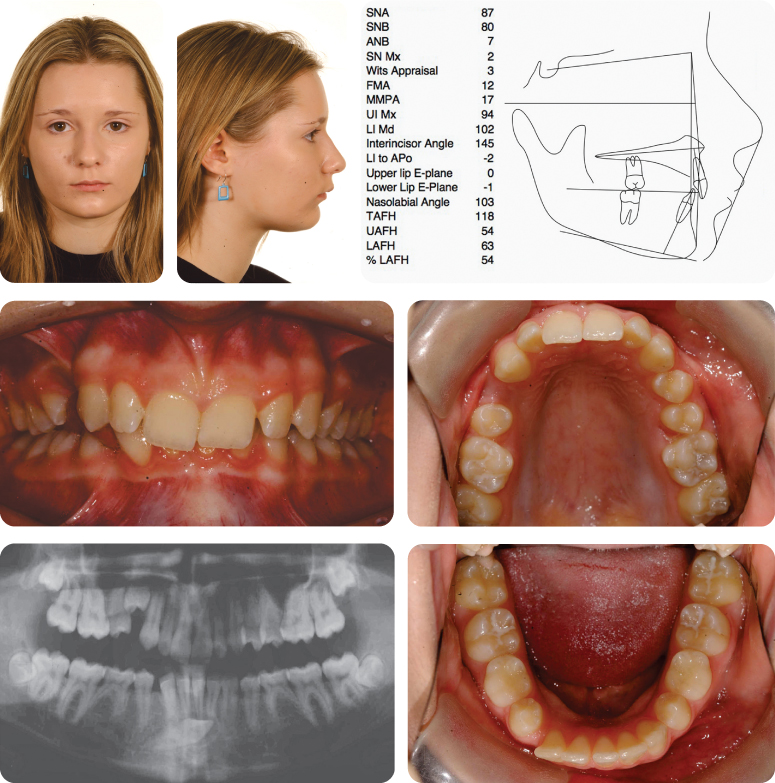
Describe the Skeletal Deformity
The patient has a skeletal class II discrepancy associated with a retrognathic mandible. She has reduced vertical proportions with a reduced FMPA and reduced lower anterior face height. There is no facial asymmetry.
Summarize the Problems on Intra-Oral and Radiographic Examination
- Hypodontia: congenital absence of the LL5 and LR5, retained LLE and LRE
- Ectopic, unerupted, transmigrated LR3
- Impacted UR4
- Class II division 2 malocclusion with retroclined upper central incisors and an increased and complete (to mucosa) overbite, which is potentially traumatic
What Is the Index of Orthodontic Treatment Need (IOTN) of This Malocclusion?
The IOTN is 5i.
How Would You Assess the Position of the LR3? What Is the Prognosis of This Tooth and How Could It Be Managed?
Clinical examination would involve visual inspection and palpation for the tooth buccally or lingually. In this case, the tooth was visible as a bulge in the buccal sulcus and could be palpated.
Radiographic assessment shows that the crown of the LR3 was lying horizontally, below the roots of the lower incisors.
The prognosis for the LR3 is poor due to the position. Orthodontic alignment would not be possible. If this were attempted, damage to the roots of the lower incisors may well occur.
What Is The Prognosis For the Lower Second Primary Molars? How Is This Assessed?
The lower second primary molars have a good prognosis. Clinically the primary teeth were firm, unrestored and showed no sign of infra-occlusion. Radiographically there was no evidence of root resorption or caries.
The UR4 Is Impacted. Will It Be Possible to Align This Tooth Orthodontically?
The panoramic radiograph reveals that the UR4 is rotated through approximately 90 degrees. Space creation by proclination and torque of the upper labial segment should provide additional space for this tooth and, once derotated, the tooth will occupy less space in the arch. Surgical exposure and bonding of this tooth will facilitate eruption.
What Are the Possible Treatment Approaches for Management of This Malocclusion? Outline a Possible Treatment Plan for Each Approach
- Growth modification: At 16 years of age, growth modification is not a realistic proposition in a female patient. A functional appliance could be considered to attempt some correction of the malocclusion through favourable tooth movement, but success is unlikely because of the lack of underlying growth and a reduced likelihood of good compliance in a 16-year-old girl.
- Orthodontic camouflage: Treatment would be carried out with upper and lower pre-adjusted edgewise appliances. The ectopic LR3 would be removed. In the lower arch the lower second primary molars would be retained, with a view to maintaining them as long as possible. When these teeth are lost in the future they could be replaced restoratively.
In the upper arch, a camouflage approach would require the loss of two premolar units. In this case it would be appropriate to remove both upper first premolars, to provide adequate space for reduction of the overjet produced, which would be achieved using torque and retraction of the upper labial segment. - Orthodontics and orthognathic surgery: Pre-surgical orthodontic treatment would involve removal of the ectopic LR3, and exposure and bonding of the impacted UR4. An overjet would be produced during orthodontic decompensation prior to surgical mandibular advancement.
A decision was made to treat the patient with orthodontics and orthognathic surgery.
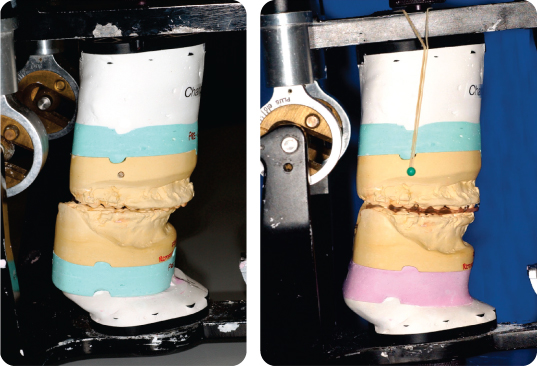
Describe the Mechanics Being Used in Figure 10.10
In the upper arch, Burstone mechanics are being used to allow simultaneous correction of the torque in the upper labial segment and reduction of the overbite. In addition to a base archwire, an auxiliary arch wire with tip back bends is placed in the auxiliary tubes in the molar bands and ligated anteriorly to the base archwire with a ligature. A trans-palatal arch is in situ to prevent buccal flaring of the molars. The UR4 is brought down into the arch using elastomeric chain attached to a gold chain following previous exposure and bonding of this tooth. Powerchain is also being used to derotate the UL4 and UR5, which have been banded and have metal cleats attached on the palatal side.
The Patient Is Shown at the End of The Pre-Surgical Orthodontic Phase of Treatment in Figure 10.11. What Is the Relevance of the Pre-Surgical Overjet in This Case?
The pre-surgical overjet dictates the mandibular advancement that can be achieved by the surgery. In order to check that sufficient increase in the overjet has been achieved, asking the patient to posture into a class I incisor relationship should reveal the desired change in facial profile.
Why Has the Overbite Not Been Completely Reduced Pre-Surgically?
Maintaining an increased overbite will facilitate some increase in the lower anterior face height as the mandible is advanced, which was thought desirable in this case.
What Is Illustrated in Figure 10.12?
Model surgery has been carried out in the laboratory. In this case the planned surgery was a mandibular advancement. The pre-surgical position has been reproduced using the articulated models on the left. On the right, the post-surgical position has been reproduced and an acrylic surgical wafer fabricated. This wafer will be used by the surgeon in theatre to accurately position the mandible in the correct post-surgical position.
What Is the Rationale for Model Surgery?
Model surgery allows the final position of the occlusion to be checked based on the planned surgical moves. The prescription for the model surgery is planned around the clinical assessment pre-surgically. If the aims of the pre-surgical orthodontics have been achieved, the definitive surgical plan should match the original proposed plan.
The model surgery may highlight the need for additional orthodontics before the surgery to enable the proposed plan to be achieved, or more rarely may suggest the surgical plan be amended. A change in surgical plan at this stage, in order to accept the occlusion may result in a compromise in the facial aesthetics.
The model surgery also allows the laboratory to produce surgical wafers which are used in theatre to help achieve the planned surgical moves.
Why Are Study Models Mounted Using a Facebow Record?
A facebow record is required if maxillary surgery is planned. The relationship between the Frankfort plane, maxillary base and terminal hinge axis of the mandible is recorded. Consequently, the influence of mandibular auto-rotation secondary to maxillary procedures may be gauged more accurately.
The Post-Surgical Records Are shown in Figure 10.13. What Is Being Carried Out in the Upper Left Panel?
The lower arch was not levelled pre-surgically, by maintaining the curve of Spee, an increase in lower anterior face height can be achieved with the mandibular advancement surgery. The post-surgical mechanics involved closure of the resulting lateral open bites with the use of bilateral box elastics. In order to facilitate this post-surgical settling, the lower archwire was changed to a 19 × 25-inch braided stainless steel.