Chapter 10
Making a Referral
Introduction
A referral is essentially a request for assistance regarding a patient, from an appropriate colleague. This may be a referral from primary care to secondary care or occasionally between clinicians in secondary care. Common principles apply to both. The referring practitioner may require a second opinion, or in many cases, the referral may also request that management of a patient be undertaken. Such a referral requires the transfer of information between the referring dental surgeon and, in many cases, a specialist, and may take a verbal, electronic or written form. Often, the referral may be an elective process following discussion between the patient and clinician regarding treatment options. However, on other occasions, the referral may require the prompt attention of a specialist to deal with an urgent concern raised by the patient or clinician. In order to facilitate the efficient referral of a patient, a few simple principles should be followed and these are discussed later.
When to refer
According to the General Dental Council’s ‘Standards for Dental Professionals’, 2009, registered dentists are expected to:
1.3 Work within your knowledge, professional competence and physical abilities. Refer patients for a second opinion and for further advice when it is necessary, or if the patient asks. Refer patients for further treatment when it is necessary to do so.
As such, the need for referral may be that the situation lies outside:
- the knowledge;
- the skill;
- the experience; or
- the facilities available to the referring dentist.
Knowledge and skills may change with time as experience is gained, or postgraduate training is undertaken. Conditions that may be referred in the early stages of a clinician’s career may be something that can be managed confidently later. Therefore, it is important that practitioners recognise their own level of competence. When deciding not to refer, then the clinician must be certain that they can manage the situation with the patient’s safety and best interests in mind.
In a profession in which time and monetary issues are frequently influences on treatment, it must be considered whether it is acceptable or indeed ethical to refer a patient for the management of a complaint that the referring dentist is capable of managing in every other respect. Referral of such cases increases the workload of the person or department receiving the referral and will inevitably lead to delays in managing patients that require more urgent or specialist care.
How to refer
The most common form a referral takes is that of a letter. Many attempts have been made to produce standard pro forma letters to simplify the process of referral. Standard letters are also considered by some to improve the information, which is provided by prompting the referrer for information. However, a written letter allows flexibility in the approach and a full description of a patient’s condition. The disadvantage of any written medium is ensuring that it reaches its destination in a timely manner, or indeed that it reaches its destination at all. Where an urgent referral is required, letters may be faxed. Faxing a letter may produce a record that the letter was sent, although not that it was received. In many cases, an identical letter is faxed and a copy also sent by mail. Where this is the case, it is important to mark the posted letter as a copy, in order that a duplicate appointment is not arranged, as it may be difficult to identify and match duplicate letters. Emergency referrals may also be made by telephone call. It is important to keep a record of the telephone conversation, and best practice is to follow this up with a letter. The letter should refer to the telephone conversation and provide the appropriate details expected in any referral. The use of electronic mail or online referral of patients has yet to become common practice, but many centres are now developing this service.
When a referral is made, it is important to retain a copy of correspondence in the patient’s records for medico-legal reasons. It may also be good practice or, depending on local policy, necessary to send a copy of the correspondence to the patient.
Patient confidentiality should be maintained at all times. Letters and faxes should be marked as confidential, as by their very nature they contain patient identifiable data and sensitive clinical information.
Where to refer
Careful consideration should be made with regard to where, and whom to refer a patient. Secondary care and specialist services are generally provided by district general hospitals and teaching hospitals. The community dental service may also accept referrals. Practitioners should consider what service the patient requires. In some cases, more than one service may be necessary. Where a single referral letter containing multiple unrelated requests is sent, this may delay treatment. The department receiving the referral initially may deal with the relevant issue to completion before returning the patient to the referrer with remaining issues unresolved. Referring for unrelated items is usually best done by individual letters to each appropriate department.
Most receiving units will ‘triage’ referral letters. The information contained within each letter is examined to determine the nature of the referral and the degree of urgency. The referral may then be ‘graded’, for example as urgent or routine and placed on an appropriate waiting list. Such triage ensures that, where sufficient detail is provided, potentially urgent issues are identified and treated as such. Although referral may be made to a named consultant, in order to minimise waiting times, the patient may be seen by another appropriate consultant. Similarly, specialists within a department may have different sub-specialty interests and referrals may be redirected to the most appropriate person.
If the practitioner is unsure as to whom to refer, it may be acceptable to refer to ‘the consultant’ in the most relevant department, with redirection by that person on receipt. This again may delay the patient being seen, and it may be better practice to contact the referral centre or department by phone for advice. This will ensure that the correct person receives the referral promptly.
The referral letter
The minimum data that a referral letter must include is summarised in Box 10.1 and an example of a ‘good’ referral letter is given in Figure 10.1.
Figure 10.1 An example of a ‘good’ referral letter that contains all the salient information that the receiver needs to know.
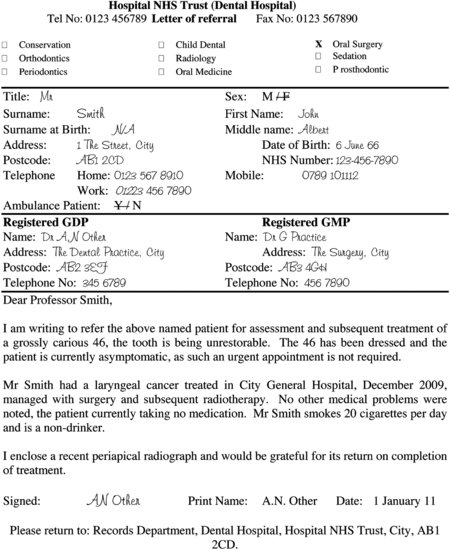
Box 10.1 Minimum data to be included in the letter of referral
- Referring dentist’s name, address and a telephone number
- The patient’s name, date of birth, address and telephone number
- An indication of the urgency of the referral
- The presenting complaint
- History of the presenting complaint
- Clinical findings
- Relevant medical history
- Whether an opinion or management is sought
In addition to those factors listed in Box 10.1, if the patient has been referred in the past, reference numbers or patient identifier numbers of the receiving centre should also be clearly stated as these will facilitate recall of existing notes and correspondence, greatly assisting in the management of the patient.
Other than the essential demographic data required to contact the patient, the nature of the problem is the next most important information. This should follow the order of a simple patient assessment. Where appropriate, the patient’s presenting complaint and history of the complaint should be given, along with the treatment history subsequent to presentation. Clinical findings should be summarised as follows:
- Accurate description of site size and nature of lesion(s)
- A brief report of radiographic findings
- Results of other investigations
If the referral concerns a soft tissue lesion, for example an oral mucos/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


