chapter 10 Intramuscular Sedation
The intramuscular (IM) route of drug administration is a parenteral technique in which the drug enters the cardiovascular system without first passing through the gastrointestinal (GI) tract. Parenteral techniques possess an advantage over enteral techniques (oral, rectal) in that the drug does not first have to pass through the enterohepatic circulation before entering the systemic circulation. This eliminates several disadvantages of enteral routes, including a possible hepatic first-pass effect, presence of food in the stomach, and delayed gastric emptying. The advantages and disadvantages of the IM route were discussed in Chapter 3 and are summarized in Box 10-1.
Probably the most significant negative aspect of using the IM route is an inability to titrate the drug to a desired clinical effect. The dentist is unable to consistently predict the proper dose to administer in any given patient, leading to the use of an “educated guesstimate” based on a number of factors to be discussed shortly. Although the dose is often appropriate, situations occur in which the calculated dose proves ineffective, leading to an inability to treat the patient. More significant, however, are those occasions when the calculated dose has proven too great for the patient, leading to possibly dire consequences for both the patient and the dentist.1–4
Suggested uses of the IM route in the dental office include the following:
All 50 states in the United States require a dentist employing parenteral (IM/IN/IV) sedation to obtain a special permit from the state board of dental examiners. State requirements for parenteral sedation permits vary, but take into account the degree of education in the technique, preparedness for emergencies, and demonstrated clinical proficiency.5
Another use of the IM route in dentistry is the administration of nonsedative drugs. These drugs may also be administered orally or rectally; however, because of the greatly increased reliability of absorption and greater efficacy noted with the IM route, this technique should be considered when these drugs are used. Drugs commonly administered via this route are the anticholinergics (atropine, scopolamine, glycopyrrolate) and the antiemetics (ondansetron [Zofran], promethazine). These drugs are discussed later in this chapter. The suggested uses of IM drug administration in dentistry are presented in Box 10-2.
Box 10-2
Recommended Use of the Intramuscular Route
SUBMUCOSAL SEDATION
A variation on IM drug administration called submucosal (SM) administration has been used in pediatric dentistry.6 In the SM technique, a CNS-depressant drug is injected into the mucous membrane in either the maxillary or mandibular buccal fold. An advantage of SM administration over IM administration is a slightly more rapid onset of clinical action.7,8 However, this same rapid onset of action may also be associated with a more rapid appearance of undesirable drug actions, such as respiratory depression. As originally developed, the SM route was used for the administration of opioid agonists (OAs), such as alphaprodine.9 The technique has fallen into disrepute because of a significant number of serious adverse reactions that were noted in conjunction with the SM administration of alphaprodine.1–36 The SM route is discussed in greater detail in Chapter 35.
SITES OF INTRAMUSCULAR DRUG ADMINISTRATION
Four sites are available for IM drug administration.10–12 Proper site selection varies from patient to patient and is an important factor in the safety of this technique. The sites most commonly chosen for the administration of IM drugs are the following:
Gluteal Area
The upper outer quadrant of the gluteal region is the most commonly used site for IM drug administration in adults.13 The gluteus maximus is the muscle most commonly injected.
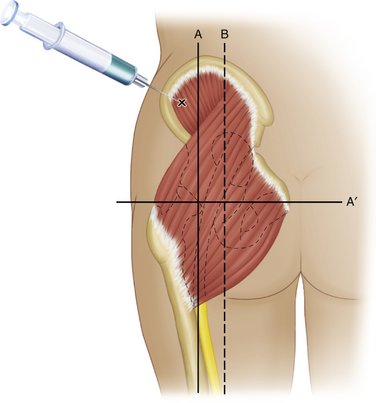
The gluteal region extends superiorly to the anterior superior iliac spine (Figure 10-1). With this as a landmark, the region is divided into quadrants. The upper outer quadrant is the most anatomically safe because it is distant from the sciatic nerve and the superior gluteal artery.14 The lower inner aspect of the upper outer quadrant is the preferred site within this quadrant.
The gluteal region in the adult can accept 4 to 8 ml of solution.11,14 In addition, the skin of this region is relatively thin and is more easily penetrated by the needle.
The upper inner quadrant is unacceptable as an IM injection site because it contains the roots of the sacral plexus. The lower inner quadrant contains the sciatic nerve. Ceravolo et al13 report a nerve injury rate of up to 8% following IM injection into the gluteal region.
For injection into the upper outer quadrant, the patient should be lying face down on a bed or examining table with the toes in and arms hanging off the table.15 This permits maximal relaxation. Although this site is also used with the patient standing, it is not as highly recommended because the muscles do not relax as well in this position. Muscle tissue that is contracted does not accommodate the injected fluid, forcing it upward into the subcutaneous tissues, where absorption is less reliable and slower and where certain chemicals are more likely to produce tissue irritation and damage. In addition, the administration of IM drugs into contracted muscle is thought to be more uncomfortable than IM injection into relaxed muscle.12
Of the four available IM injection sites, the gluteal region is the least well perfused, having 20% lower perfusion than the deltoid.16 Because perfusion is the rate-limiting step in the absorption of IM drugs, the rate of onset of action of drugs administered in the gluteal region is somewhat slower than when alternative sites are used.11,14
Ventrogluteal Region
The ventrogluteal region lies in close proximity to the gluteal region. Its primary use is for IM injection in patients who are bedridden and unable to lie face down.14
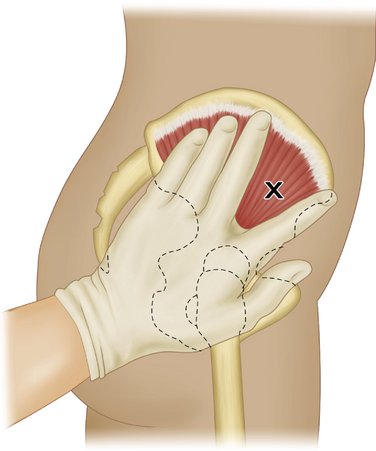
The site is located among three bony landmarks that are usually quite readily palpated. These are the anterior superior iliac spine, the iliac crest, and the greater trochanter of the femur. Anatomically, this region lies at some distance from the sciatic nerve and other anatomically important structures.15
For this site to be properly used, the anterior superior iliac spine is located with the tip of the index finger (Figure 10-2). The left hand is pressed onto the hip with the palm of the hand over the greater trochanter and the fingers pointed toward the patient’s head. The index and middle fingers are spread as far as possible, forming a V, with the tip of the ventrally placed finger pressed down on the soft tissue over the anterior superior iliac spine, preventing movement of the skin. The needle puncture is made between these fingers and aimed just below the iliac crest.
Vastus Lateralis
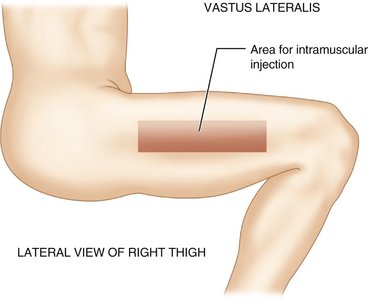
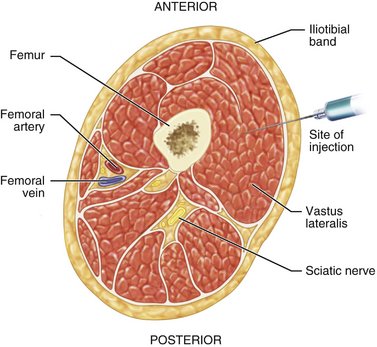
The site for injection in the vastus lateralis muscle is a narrow rectangular band running along the anterior lateral aspect of the thigh (Figure 10-3). The region begins approximately one handbreadth above the knee and runs to the same distance below the greater trochanter of the femur.15
Anatomically the vastus lateralis site contains no structures of importance (Figure 10-4). Overly deep penetration of the needle may strike the femur, resulting in discomfort and possible needle breakage. All significant anatomic structures are located on the medial and posterior aspects of the thigh (the femoral artery and vein and the sciatic nerve).
This site is strongly recommended for use in small children.11 Injection in the gluteal muscles is contraindicated in children who have not yet begun to walk because of the lack of maturity and development of their gluteal musculature. The gluteal region ought not to be chosen until at least 1 full year after the child has begun to walk.17
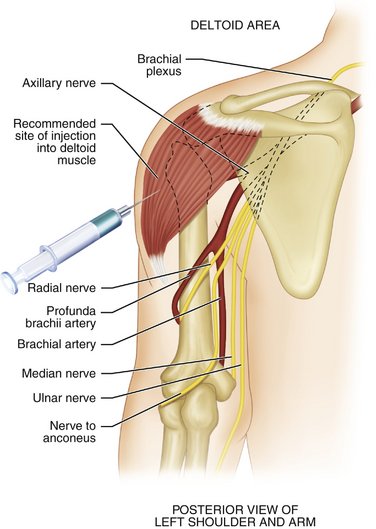
Deltoid
The deltoid muscle is easily accessible in the upper third of the arm. The injection is given between the upper and lower portions of the deltoid muscle (Figure 10-5), thereby avoiding the radial nerve.
Advantages of the deltoid region include easy access in most patients. It is important that the patient not be permitted to simply roll up the shirt sleeve to expose the injection site because if the sleeve is tight, it may not permit visualization of the entire site, in which case the injection might be administered inferior to the desired area and in too close proximity to the radial nerve. The patient should be required to remove the shirt or blouse to expose the entire injection site. A female assistant must be with the dentist (male or female) if the patient is female. Another positive factor in the deltoid region is more rapid absorption of the injected drug into the cardiovascular system than is seen with any of the other IM injection sites. Perfusion is 20% greater in the deltoid region than in the gluteal region.14 The deltoid region is not recommended for use in the infant or child who has not yet begun to walk.11
Probably the only negative feature of this site, other than the anatomy, is its lack of size; it is able to accommodate only up to 4 ml of solution (adult). However, this is not of significance in dentistry because it is rare to ever administer more than 3 ml intramuscularly. Giovannitti and Trapp18 suggest the deltoid muscle as the preferred site for IM sedation in the dental environment.
Site Selection
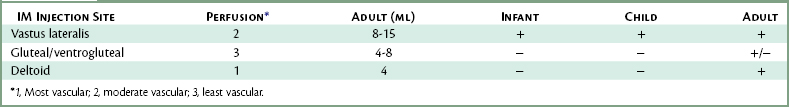
Selection of the site for IM injection in dentistry is predicated on several factors, including the size (age) of the patient, degree of patient cooperation, and volume of solution to be injected. In the younger (smaller) pediatric patient, the preferred site for IM injection is the vastus lateralis, whereas in older children the vastus lateralis and the deltoid regions are recommended. In the adult, the preferred sites for IM injection are the deltoid region, vastus lateralis, and both gluteal injection sites. Table 10-1 compares the four IM injection sites.
ARMAMENTARIUM
Very few items are required for IM drug administration. Included in this list are the following:
There is a very real concern for self-inflicted puncture injuries among health care professionals with possible infection with either human immunodeficiency virus (HIV) or hepatitis.19–22 Syringes and other devices (e.g., the “sharps” container) have been developed to permit IM drug administration with a minimal risk of needlestick injury.23–25 These “safe syringes” prevent accidental needlestick following drug administration through a self-locking sheath that covers the exposed (and now contaminated) needle.
TECHNIQUE
The appropriate injection site for the IM injection must be selected. After disrobing the patient, if necessary, the dentist must carefully palpate the site on every patient to determine the precise anatomic landmarks. Visual examination alone should never be relied on to determine landmarks. From the point of view of propriety (and medicolegally), it is important that the dentist have another staff member present in the treatment room during the injection, especially if the patient is of the opposite sex from the dentist. The following are step-by-step instructions for the administration of an IM injection11,15,26:
COMPLICATIONS
Although rare, complications can arise after IM drug administration. In most cases, the complication appears to be directly related to the site of needle entry and drug deposition.27,28
Management (rescue) of an oversedated patient consists primarily of airway maintenance (A, airway) and, when necessary, assisted or controlled ventilation (B, breathing). In addition, some drugs, such as the opioids and benzodiazepines, have pharmacologic antagonists that may be administered in these circumstances. Their use and a more detailed discussion of the management of the oversedated patient are found in Chapters 27 and 34.
Cyst formation, scarring, and necrosis and sloughing of tissues may also occur. Although several factors may be responsible for these, many are produced by the tissues’ reaction to the injected drug. Drugs that are irritating to the tissues are more commonly involved in these complications. Superficial injection of drugs is another possible cause of this problem. Management should consist of referral to a physician, preferably a dermatologist. Complications of IM injections are listed in Box 10-3.
DETERMINATION OF DOSAGE
The factors that influence the way in which a drug acts in a given patient were discussed in Chapters 3 and 7. With IM administration of CNS depressants, the influence of these various factors becomes quite important. How can the informed clinician safely determine the appropriate IM dose of the drug or drugs that are to be administered to a patient for intraoperative sedation?
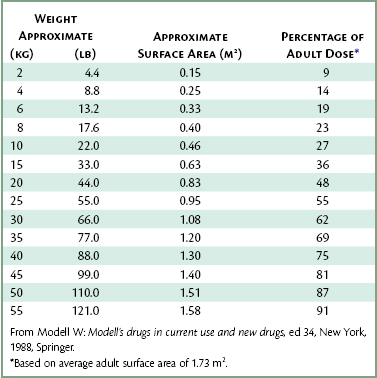
A factor that has proven even more accurate in determining effective pediatric dosages is the body surface area of the patient. Table 10-2 permits a determination of the approximate surface area of the patient. The pediatric dosage is determined as a percentage of the usual adult dosage, based on the average adult surface area of 1.73 m2.
Most of the drugs discussed in this chapter have their dosages presented on a milligram per kilogram or pound of body weight basis. Although not the most accurate method available, this remains the most frequently employed method of determining IM drug dosage. The reader may employ the surface area method of determining pediatric dosages for any drug listed in this book by simply referring to Table 10-2.
Dosages based on body weight (e.g., 1 mg/kg or 0.5 mg/lb) are determined by the middle of the “bell-shaped” curve (see Figure 7-1). Approximately 70% of patients respond appropriately to this dose, with 15% undersedated. Unfortunately, another 15% respond in an exaggerated manner—oversedation.
DRUGS
A myriad of drugs are available for the management of anxiety via IM administration. The level of sedation may vary from lighter levels (minimal to moderate sedation) to levels approaching unconsciousness (deep sedation). Although certain drugs are more apt to produce more profound sedation than others, any of the following drugs listed can produce overly deep sedation. When IM drug dosage is determined, it must always be remembered that the administrator cannot control the drug’s action, and that titration is not possible via this route. Care and prudence must be exercised whenever IM drugs are administered to all patients, but especially to pediatric, geriatric, or medically compromised patients. Box 10-4 lists drugs that are commonly given via IM administration in dentistry. As will be noted with specific drugs, different levels of training are recommended for their safe use. In some situations, the dentist should have received training in general anesthesia and be capable of managing the unconscious airway before ever considering the use of the drug in question.
Antianxiety Drugs and Sedative-Hypnotics
Chlordiazepoxide
Chlordiazepoxide should be administered deep into muscle to minimize discomfort and to optimize absorption. It is recommended that the drug be deposited slowly into the upper outer quadrant of the gluteus muscle.29 Any unused drug should be discarded. Following parenteral administration deep into muscle, the onset of action will be approximately 15 minutes. Maximal clinical effect arises 30 minutes following injection, with a gradual decrease in clinical action over the next 3 to 5 hours.30
Diazepam
Another reason for the infrequent use of diazepam IM was the results of early studies on the absorption of diazepam from IM injection sites. Diazepam injectable is an extremely lipophilic drug, and early studies on absorption of IM diazepam were conflicting.31–34 Peak plasma levels were noted 60 minutes after oral dosing, whereas IM dosing required 90 minutes.34 Absorption of diazepam from IM injection sites may be slow or incomplete or both because of its lipophilic nature. However, a more recent report indicates that IM diazepam absorption appears to be more rapid when the drug is injected into the deltoid rather than the gluteal or vastus lateralis muscle groups.35 The most likely explanation is the higher blood flow per gram of tissue in the deltoid muscle group.33 In the gluteal area, the depth of injection may be a factor in the completeness of absorption of diazepam. Given equal doses of diazepam via the oral and IM routes, the oral dose will be absorbed more completely than the IM dose, and in many cases, the rate of onset will be shorter via the oral route than with the IM route.34 However, diazepam deposited deeply into muscle (preferably the deltoid) can produce satisfactory sedation in most patients.
Lorazepam
Because the agent is virtually insoluble in water, its onset of action may prove to be prolonged in some patients, although, as with diazepam, the onset of action will be about 15 minutes in most patients. Peak plasma levels of lorazepam are seen in 60 to 90 minutes.36 The duration of action of lorazepam following IM administration is approximately 6 to 8 hours. The major side effect is excessive sleepiness and a prolonged amnesic period.
Odugbesan and Magbagbeola37 recommend that the IV route be preferred to IM for administration of lorazepam, providing a somewhat more rapid onset of activity. Patients receiving lorazepam IM must not be permitted to leave the dental office unescorted and must be advised of the possibly enhanced CNS-depressant actions of other agents, such as opioids, alcohol, and barbiturates. Because of the prolonged duration of action of lorazepam, it is seldom used in the outpatient practice of dentistry.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses