10
Detection of Incidental Findings in Cone Beam Computed Tomography Imaging and Their Clinical Implications
Introduction
The introduction of cone beam computed tomography (CBCT) to dentistry in the late 1990s transformed the way the profession as a whole analyzes the oral and maxillofacial complex. Dental providers, who previously were limited to two-dimensional (2D) images of three-dimensional (3D) anatomical structures, now have the ability to visualize the hard tissues of the head and neck in all the desired planes as well as in 3D reconstructions. The principal limitation of CBCT is that the soft tissue resolution is limited to visualization of the soft tissue profile, the airway, and the relatively higher density muscles and major salivary glands.
Since the introduction of CBCT is relatively recent, many dentists have not been trained to identify the cross-sectional anatomy visualized in CBCT imaging; an overview is provided in Chapter 9. In addition, CBCT scans may reveal occult pathology and incidental findings of varying clinical significance located in structures outside a dentist’s conventional area of expertise.
The frequency of incidental findings identified by CBCT has been reported to be as high as 3.2 findings per scan (Price et al., 2012). Not surprisingly, individual studies have reported different frequencies of these incidental findings, depending on the field of view (FOV) employed, the average age of the population studied, and the method used to categorize these findings (Miles, 2006, 2010; Cha et al., 2007; Rogers et al., 2011). Price and colleagues (2012) reviewed 272 consecutive CBCT scans and found that the most prevalent incidental discoveries were airway-associated findings (35%), soft tissue calcifications (20%), lesions of bone (17.5%), temporomandibular joint (TMJ; 15.4%), endodontic etiology (11.3%), developmental dental lesions (0.7%), and pathologic lesions (0.1%). Of these findings, 16.1% required intervention/referral and 15.6% required monitoring; the remainder (68.3%) required no further treatment. Similarly, Caglayan & Tozoglu (2012) conducted a review of 207 consecutive CBCT scans and reported that the highest number of incidental findings was noted within the airway structures (51.8%), followed by the presence of impacted teeth (21.7%), TMJ-associated lesions (11.1%), endodontic lesions (4.3%), condensing osteitis (1%), and miscellaneous other processes (2.9%). Lack of recognition of these incidental findings can have significant medico-legal implications (Zinman et al., 2010; see also Chapter 7). On the other hand, the untrained clinician may have a higher likelihood of reporting false-positive findings, which could result in unnecessary healthcare costs and patient anxiety (Kapila et al., 2011; Ahmed et al., 2012).
In orthodontics, the use of extended or large FOV CBCT scans is relatively common since one of the principal applications of CBCT imaging is the evaluation of the craniofacial complex prior to orthognathic surgery or, in some instances, as an alternative to traditional 2D radiographic imaging even in nonsurgical cases. Using an extended FOV increases the likelihood of discovering incidental pathology since a larger volume of the head and neck is imaged.
A recent study demonstrated that orthodontists and orthodontic residents failed to detect approximately 67% of incidental lesions while having a 50% false-positive detection rate. These numbers decreased to 33% and 30%, respectively, after 3 hours of training by an oral and maxillofacial radiologist (Ahmed et al., 2012). This highlights the importance of having an oral and maxillofacial or medical radiologist assist with the interpretation of CBCT scans.
The objective of this chapter is to provide information on the radiographic presentation and locations of incidental and pathological findings in CBCT scans, as well as their clinical implications. The overall goal of this chapter is to enhance the diagnostician’s ability to identify these lesions and undertake appropriate steps where needed. More specifically, we review incidental findings under the categories of (1) intracranial soft tissue calcifications and lesions, (2) extracranial soft tissue calcifications, (3) airway lesions, (4) lesions of the paranasal sinuses and nasal cavity, (5) tooth-related findings and developmental defects of the jaws, (6) TMJ-associated processes, (7) lesions of the cervical spine, and (8) other miscellaneous findings. Within each of these sections, we provide tables summarizing the CBCT presentation, age and sex distribution, and clinical implications, including the recommended follow-up for each CBCT lesion or finding.
Intracranial Soft Tissue Calcifications and Lesions
Internal Carotid Calcifications
Internal carotid calcifications represent deposits of fat, cholesterol, and associated inflammatory cells that contribute to the formation of a plaque within the artery. Progressive narrowing of the internal diameter of the arterial lumen reduces the maximum volume of blood flow. This process ultimately may result in decreased vessel elasticity and erosion of the vessel walls. Plaque deposits also can become dislodged and transported to other structures, resulting in pulmonary emboli or deep vein thrombosis, or may lead to a myocardial infarction or stroke. On CBCT imaging, internal carotid calcifications are seen as high-density, well-defined, single or ring-like opacities commonly located on either side of the sella turcica or the sphenoid sinus (Figure 10.1; Table 10.1). They tend to be bilateral and are more common in older male patients. The prevalence of identifiable intracranial carotid calcifications in CBCT scans has been reported to be as high as 0.5% (Price et al., 2012). Overall, intracranial calcifications have been reported to occur in greater than 80% of older Caucasian individuals (Bos et al., 2012). The presence of intracranial carotid calcifications has been linked to smoking, hypercholesterolemia, and a history of cardiac disease (deWeert et al., 2009). These calcifications are an indicator of arterial stenosis, which is associated with an increased risk of stroke. Therefore, identification of internal carotid calcification by CBCT imaging mandates referral for further medical evaluation.
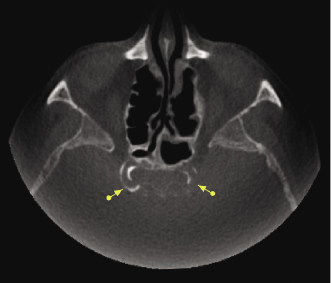
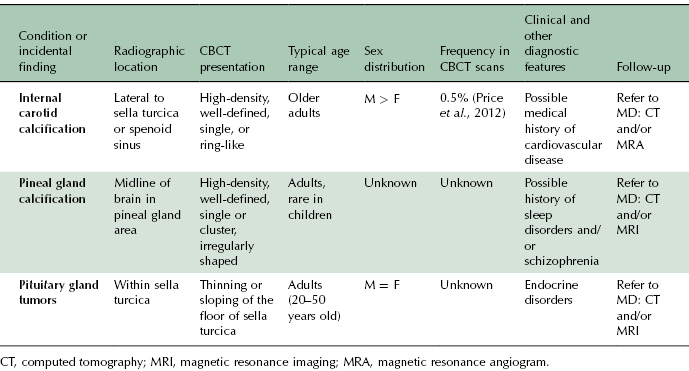
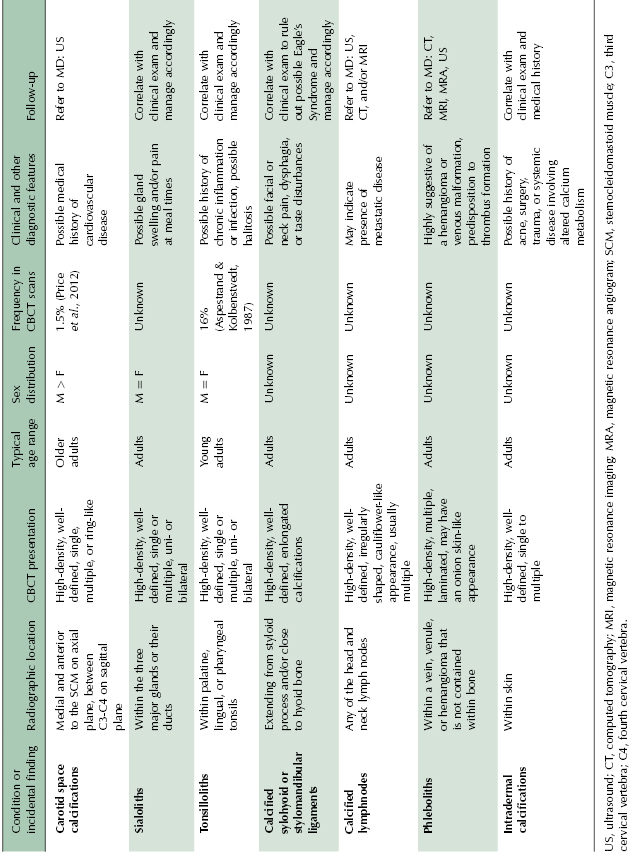
Table 10.1 Summary of CBCT presentation, age and sex distribution, additional diagnostic features, and recommended follow-up of intracranial soft tissue calcifications and lesions.
Pineal Gland Calcifications
The pineal gland is a small endocrine gland located between the two hemispheres of the brain, approximating the center. It is larger in children, with a decrease in size noted after the onset of puberty. It produces the serotonin derivative melatonin, a hormone that affects the modulation of wake/sleep patterns and seasonal functions and plays an important role in sexual development and metabolism. In CBCT scans, calcifications of the pineal gland area can be seen as a single lesion or a cluster of multiple small high-density, well-defined, irregularly shaped opacities, typically 3–5 mm or smaller (Figure 10.2; Table 10.1). Pineal gland calcifications have been linked to sleep disorders and schizophrenia (Bersani et al., 1999; Kunz et al., 1999); these are rare in children younger than 6 years of age. When found in this age group or when greater than 1 cm in diameter, the possibility of a pineal gland tumor should be considered.
Pituitary Gland Tumors
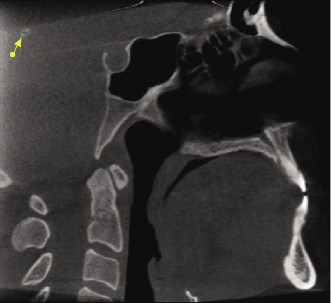
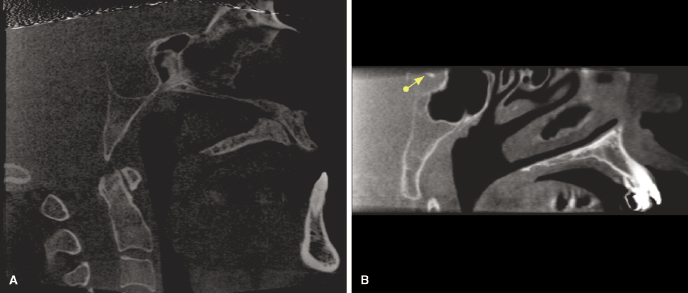
The possibility of a pituitary adenoma, the most common neoplasm arising within the substance of the pituitary gland, should be suspected when the pituitary gland measures greater than 9 mm in the superior to inferior dimension. These occur with equal frequency in males and females, typically in individuals between the ages of 20 and 50 years. On CBCT imaging, thinning and sloping of the floor of the sella turcica may be noted. On occasion, extension into the sphenoid sinus also may be evident (Figure 10.3A; Table 10.1). Although relatively uncommon, calcifications within the pituitary gland can be seen in association with certain secretory pituitary tumors (Figure 10.3B). Therefore, the presence of any of these radiographic findings requires further evaluation by medical computed tomography (CT) or magnetic resonance imaging (MRI).
Extracranial Soft Tissue Calcifications
Carotid Space Calcifications
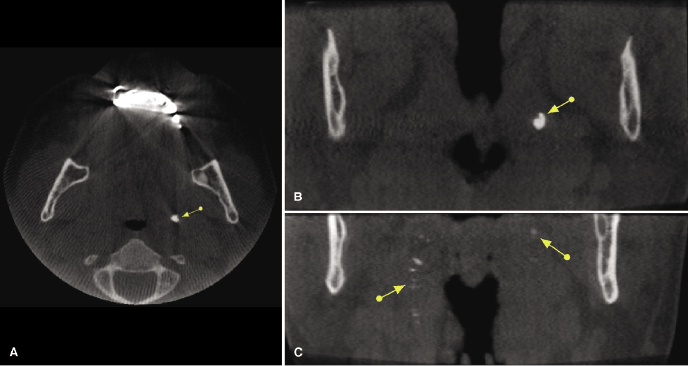
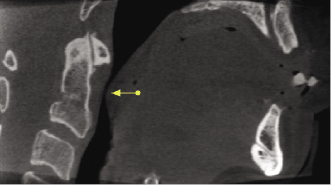
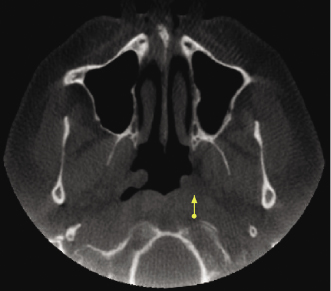
The most common location for carotid artery calcifications is at the bifurcation of the common carotid artery into the internal and external branches of the carotid artery, which is located at the level of the C3-C4 vertebrae. The incidence of carotid calcifications in a general dental population has been reported to be as high as 5% in older patients (Lewis & Brooks, 1999). On CBCT scans, Price and associates (2012) reported an incidence of 1.5%. In axial CBCT imaging, these calcifications are seen within the carotid space, located medial and anterior to the sternocleidomastoid muscle (Figure 10.4A,B; Table 10.2) as single, multiple, or ring-like well-defined high-density opacities. It is important to note that the tip of the greater horn of the hyoid bone is located in close proximity to the carotid space and may be mistaken for a single carotid calcification, particularly when this “calcification” is located toward the inferior edge of the FOV (Figure 10.4C). The presence of calcifications within the carotid space requires further medical evaluation. Doppler ultrasound has been found to be useful in determining the exact location and degree of arterial stenosis (Ravon et al., 2003).
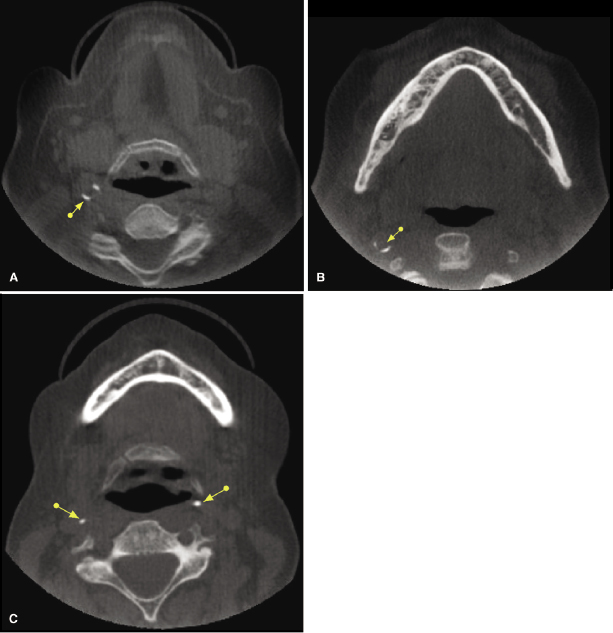
Table 10.2 Summary of CBCT presentation, age and sex distribution, additional diagnostic features, and recommended follow-up of extracranial soft tissue calcifications.
Sialoliths
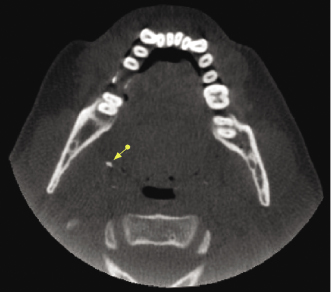
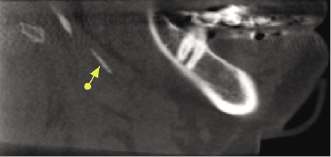
Sialoliths are crystallized minerals that can be found in the parenchyma or the ductal system of the parotid, submandibular, or sublingual salivary glands, with approximately 80% of the cases involving the submandibular gland. Submandibular gland sialoliths are located near the hilum of the gland or in the proximal portion of Wharton’s duct. Sialoliths may cause pain and swelling of the affected gland, particularly at meal times, and may be associated with decreased salivary flow. On CBCT imaging, they present as single to multiple, unilateral, or bilateral high-density calcifications within the salivary gland or their ductal system (Figure 10.5; Table 10.2). Correlation with clinical examination for the presence of associated signs and symptoms helps to determine the need for additional imaging (sialogram with plain film radiography, CT, or ultrasound) and/or the appropriate treatment.
Tonsilloliths
Tonsilloliths represent clusters of calcified material that form in the crevices of the palatine tonsils and rarely within the lingual or pharyngeal tonsils (Figure 10.6; Table 10.2). On CBCT imaging, tonsilloliths are seen as single to multiple small high-density calcifications that may be unilateral or bilateral (Figure 10.7; Table 10.2). Tonsilloliths are a common incidental imaging finding, identified in up to 16% of patients (Aspestrand & Kolbenstvedt, 1987). Their presence may indicate a history of chronic inflammation or infection; they have been found to be associated with halitosis.
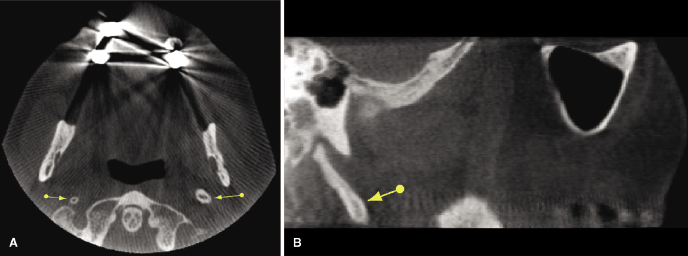
Calcified Ligaments
Unilateral or bilateral calcification of the stylohyoid or stylomandibular ligament (Figure 10.8; Table 10.2) is a frequently noted incidental finding on panoramic radiography and CBCT imaging (Radfar et al., 2008). Approximately 4% of the general population has an elongated styloid process and a partially calcified stylohyoid ligament. However, only 4% of this group is symptomatic. The etiology of this process is unknown, although congenital factors, trauma, or an inflammatory process that leads to the proliferation of granulation tissue that eventually becomes calcified have been implicated. This calcification can cause compression of adjacent structures, including the glossopharyngeal nerve, trigeminal nerve, chorda tympani, and sympathetic nerves within the carotid sheath, resulting in facial and neck pain, particularly when turning the head laterally. These also may be associated with a foreign-body sensation within the throat, dysphagia, or taste disturbances. When these symptoms are present, Eagle’s Syndrome should be suspected. Eagle’s Syndrome commonly is found in adults between the ages of 30 to 50 years, with women being affected more often than men. Treatment of symptomatic patients may require surgical removal of the calcified ligament.
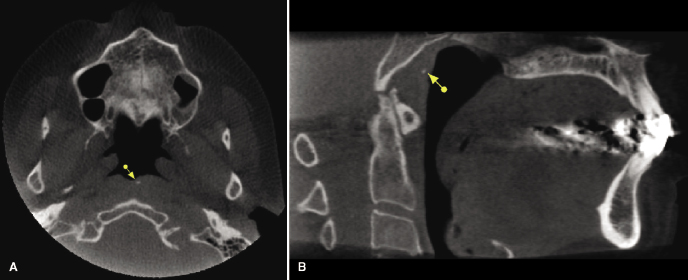
On CBCT imaging, a styloid process greater than 30 mm in length is considered “elongated” and partial calcification of the stylohyoid or stylomandibular ligaments should be suspected (Figure 10.9A,B; Table 10.2). Correlation with clinical examination is important to determine the need for further evaluation and/or treatment.
Calcified Lymph Nodes
Of the approximately 800 lymph nodes in the human body, about 300 are located in the head and neck region. CBCT will identify the presence of calcifications within lymph nodes, which may indicate the presence of chronic inflammation or infection. These usually present as well-defined, irregularly shaped calcifications that may have a cauliflower-like appearance (Figure 10.10; Table 10.2). Occasionally, the presence of calcified lymph nodes may be associated with metastatic disease.
The presence of cervical metastatic nodal disease is a major prognostic determinant for patients with head and neck cancer, associated with a significantly reduced patient survival. Traditionally, contrast-enhanced CT and/or MRI are used to identify and classify the extent and distribution of lymph node involvement in patients with head and neck cancer. Since CBCT presents limited soft tissue visualization, medical CT or ultrasound is recommended if the presence of cervical lymphadenopathy is suspected (Jank et al., 2003).
Phleboliths
A phlebolith represents a calcified vascular thrombus within a vein, venule, or hemangioma that is not contained within bone (Scarfe & Farman, 2010). The formation of a phlebolith appears to be related to the presence of a vascular anomaly, which predisposes the patient to the formation of a thrombus, which ultimately may calcify. On CBCT imaging, these usually are multiple laminated high-density calcifications that may have an onion skin-like appearance. The presence of a phlebolith is highly suggestive of the presence of an underlying hemangioma or the presence of venous malformations (Eivazi et al., 2012). Medical consultation is therefore recommended.
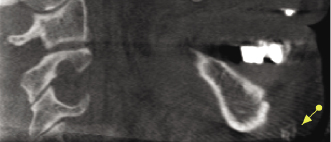
Intradermal Calcifications
CBCT images can reveal small calcium deposits that may form under the skin as a result of an injury or at the site of a previous surgical incision (Figure 10.11; Table 10.2). Multiple skin calcifications also may indicate the presence of systemic disease involving alterations in calcium metabolism. Based on underlying etiology, skin calcifications may be classified as metastatic, dystrophic, iatrogenic, or idiopathic (Walsh & Fairley, 1995). In contrast to dystrophic calcifications, metastatic cutaneous calcifications usually are associated with elevated serum calcium or phosphate levels.
Cutaneous ossification (osteoma cutis) is another intradermal radiopacity that may be observed within the skin and underlying soft tissues. Cutaneous ossification can be divided into primary (15%) and secondary (85%) forms. Secondary osteoma cutis develops within pre-existing neoplastic or inflammatory skin lesions (Cottoni et al., 1993; Fazeli et al., 1999). On CBCT imaging, intradermal calcifications are noted as small, well-defined, single to multiple, high-density areas within the skin or subcutaneous structures (Figure 10.12; Table 10.2).
Airway
Airway Narrowing and Asymmetry
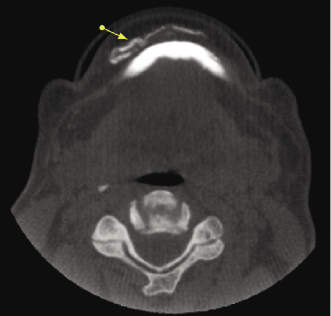
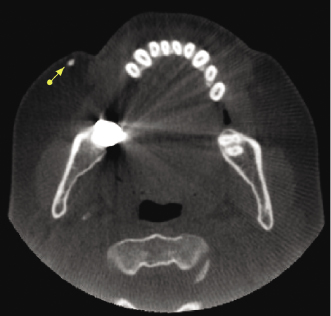
Narrowing or asymmetry of the pharyngeal space noted in CBCT imaging may be artifacts caused by breathing or swallowing during imaging or by the presence of hypertrophic tonsils. This imaging finding also may be associated with the presence of sleep apnea (see also Chapter 13) or benign or malignant tumors originating in any of the adjacent head and neck spaces (Figure 10.13; Table 10.3). A systematic and thorough review of the shape and width of the oropharyngeal and nasopharyngeal spaces of CBCT images in the axial, coronal, and sagittal planes should help to identify the presence and potential cause of airway asymmetry based on the location and direction of displacement. However, the exact cause of airway narrowing or asymmetry cannot be established based on the CBCT appearance alone (Figure 10.14). Clinical correlation and review of the patient’s medical history are essential in order to determine the need for medical consultation or further imaging studies.
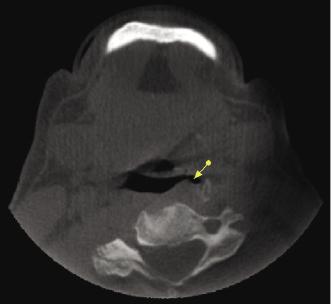
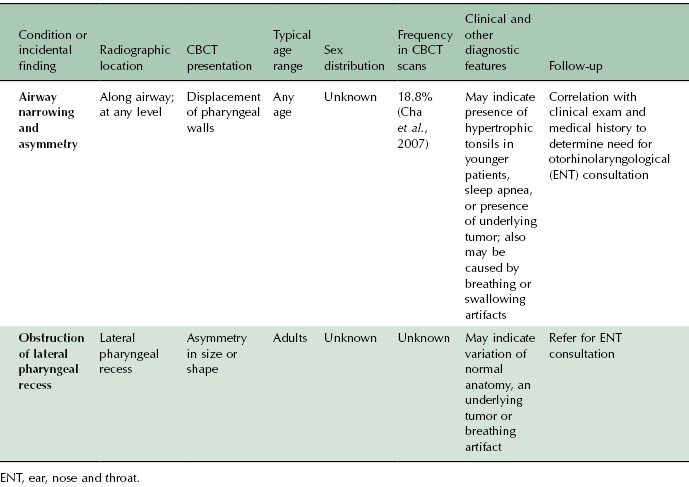
Table 10.3 Summary of CBCT presentation, age and sex distribution, additional diagnostic features, and recommended follow-up of airway findings.
Obstruction of the Lateral Pharyngeal Recess
The lateral pharyngeal recess (fossa of Rosenmuller) of the pharyngeal mucosal space may be asymmetric due to the presence of inflammatory debris and asymmetries in the volume of lymphoid tissue (Harnsberger, 1995). This asymmetric appearance can lead to the impression of a mass in the pharyngeal mucosal space (Figure 10.15; Table 10.3). To rule out this possibility, the adjacent deep spaces (parapharyngeal and retrophraryngeal spaces) must be evaluated. If the soft-tissue planes are maintained, the “mass” probably is not real. However, since the soft tissue contrast resolution of CBCT is limited, depending on the age of the patient and the presence or absence of a history of a recent upper respiratory illness, correlation with clinical evaluation of the mucosa and referral for otorhinolaryngological (ENT) consultation is recommended.
Lesions of the Paranasal Sinuses and Nasal Cavity
The nasal cavity, paranasal sinuses, and nasopharynx comprise functionally interrelated anatomic structures. While divided into separate structures based on defined anatomic landmarks, for all practical purposes, pathological processes in one of these structures predictably affect adjacent structures.
The paranasal sinuses include the bilateral maxillary, frontal, ethmoid, and sphenoid sinuses. Pathology of the paranasal sinuses is a common incidental finding on CBCT scans. In one retrospective review of 166 consecutive CBCT scans of the maxillofacial region taken for the primary purpose of implant treatment planning or for evaluation of TMJ disease, impacted teeth, or jaw pathology, 152 separate and potentially clinically significant findings involving the sinonasal complex were noted (Edwards et al., 2007). In this study, incidental findings that would have been visible readily on a full mouth series of intraoral radiographs or on panoramic views (e.g., antral pseudocysts) were excluded, as were any findings that were related to the primary indication for ordering the scan (e.g., evaluation for maxillary sinusitis in the presence of an oro-antral fistula). Ritter and associates (2012) identified the presence of maxillary sinus pathologies in 56% of CBCTs evaluated, with a trend to higher occurrence in older (>60 years of age) and male patients. Although pathology is identified most commonly in the maxillary sinuses, the remaining paranasal sinuses also are imaged when using large FOV CBCT scans as in orthodontic treatment planning. In another retrospective study, sphenoid sinus pathosis was observed in 11.9% of 227 consecutive dental patients who had undergone CBCT imaging (Bourek et al., 2008).
The most common pathologies associated with the paranasal sinuses are inflammatory in origin, specifically sinusitis and sinonasal polyposis. One study reported that such inflammatory changes of the paranasal sinuses are found incidentally in 33% of dental CBCT scans reviewed (Scanlon et al., 2007).
Sinusitis and Rhinosinusitis
Sinusitis is defined best as inflammation of the mucosa that lines the paranasal sinuses. When the nasal cavity also is involved, which occurs relatively frequently, it is termed rhinosinusitis. The most common causes of acute rhinosinusitis include viral (e.g., following an upper respiratory tract infection), bacterial, and fungal infections (Figure 10.16; Table 10.4). Rhinosinusitis is classified as chronic when both the characteristic symptoms (nasal congestion and/or discharge, facial pain, and dysosmia) and objective evidence of sinus disease confirmed by endoscopic or radiographic examination are present for longer than 12 weeks. Obstruction of the openings between the paranasal sinuses and the nasal cavity (the ostiomeatal complex), by interfering with proper drainage, plays a fundamental role in t/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


