Chapter 10
Complications of Tooth Extraction
- Pre-extraction
- During extraction
- Post-extraction
Pre-Extraction
Difficulty in Achieving Anaesthesia
Where breakdown in pain control is encountered during extraction, careful diagnosis of the nerve distribution in which pain sensation remains is essential. In the maxilla, use of the superior posterior alveolar and infraorbital nerve block should become part of the surgeon’s practice. The presence of collateral nerve supply must be anticipated and appropriate techniques such as periodontal ligament injection employed. Tooth extraction under local anaesthesia should be possible in almost all co-operative patients and the surgeon should strive to perfect techniques that ensure the procedure is painless (see Figure 7.1).
Difficulty in Co-Operation
This may be encountered at any time during the procedure, especially in those patients not amenable to reasoning, but careful preoperative assessment should alert the surgeon to such problems. The surgeon should on no account force any patient to accept treatment and an alternative method of achieving the extraction should be sought with as little delay as possible. This might involve the use of sedation or general anaesthesia.
Difficulty of Access
Trismus
Limitation of opening may be due to intrinsic causes (abnormalities in the temporomandibular joint) or extrinsic causes (facial scars and inflammatory swellings). In chronic cases it may be possible to improve the opening with exercisers, but forcing the jaws open when trismus is due to infection will break down the pyogenic membrane and cause spread. The acute phase may be treated with antibiotics and drainage and the extractions delayed until the opening is sufficiently improved, but if there is a risk to the airway there should be no delay in removing the cause and instituting drainage. In this situation admission to hospital for a general anaesthetic and high doses of intravenous antibiotics is often required.
Reduced Aperture of the Mouth
This may be due to congenital malformation (microstomia) or to scarring, making it difficult or even impossible to apply forceps or elevators to the teeth. In extreme cases a surgical approach through the angle of the mouth may be necessary.
Crowded or Misplaced Teeth
These frequently make it difficult to apply forceps or elevators without the risk of loosening adjacent teeth. This may be made easier by using a surgical technique to divide and elevate the tooth to be extracted.
During Extraction
Abnormal Resistance
Where there is no obvious clinical cause for abnormal resistance, such as the position of the tooth or the thickness of the alveolar bone, the operator should make steady and repeated efforts to loosen the tooth, avoiding too much force in one direction. After a reasonable attempt, if there is no movement, a radiograph, if not already available, is taken before proceeding further. This may show abnormalities of the roots in number or in form such as twisted, divergent, bulbous or hypercementosed roots. In age or chronic periodontal disease there may be sclerosis of the alveolar bone. Isolated teeth in occlusion are renownedly difficult to remove owing to narrowing of the periodontal membrane. Unerupted teeth impacting against the roots of the tooth to be extracted (lower third molar against second molar roots) can be a source of difficulty only discovered on a radiograph.
In all cases of abnormal resistance it is advisable to plan removal of the tooth through a transalveolar approach to reduce trauma to bone and soft tissues and avoid fracturing the tooth.
Damage to Other Teeth
Extraction of the Wrong Tooth
This is a common source of litigation and is indefensible because it is avoidable if the proper precautions are taken. Extractions should never be started without checking immediately before operation the patient’s name, address and age, the teeth to be removed and any radiographs available. This applies equally to patients operated on under local or general anaesthesia. The patient or, in the case of children, the parent is asked to confirm which teeth are to be extracted, and any doubts must be settled before the anaesthetic is given.
The notes should be placed so that the operator can see them throughout the operation and can make a final check just before the forceps are applied to the tooth. Should an error occur, the patient must be informed and the surgeon must proceed to extract the right tooth to complete the operation. A decision then has to be made whether to reimplant the wrongly extracted tooth immediately or to accept the situation.
Dislocation of Adjacent Teeth or of Restorations in Adjacent Teeth
Careless application or movements of forceps and elevators may cause this mishap. Forceps can accidentally engage part of the next tooth and so loosen it, or when drawing a lower tooth from its socket without sufficient control they may bang against the upper teeth. Elevators, misused either as class I levers or by employing a neighbouring tooth, and not bone, as the fulcrum, can do similar damage. The watching fingers of the supporting hand can assist in preventing this by feeling that the forceps are in a good position and detecting even slight movement in adjacent teeth. Where misplaced or mildly impacted teeth occur in the arch, a surgical approach may be required to allow extraction without transmitting pressure or force to neighbouring teeth.
The permanent premolars may be luxated when extracting the deciduous molars due to the root formation of the deciduous teeth, which may closely approximate the crown of the permanent tooth, or to infection, which may cause fibrosis or even ankylosis between them. More often it is due to the misapplication of instruments in the extraction of deciduous molars or injudicious attempts to remove their retained roots.
Fracture of Teeth
Where normal extracting methods are used the teeth may frequently be fractured due to advanced caries or large restorations which weaken the crown. In devitalised teeth, in periodontal disease and in the aged, the roots may become brittle, and it is unfortunate that the last two conditions are also characterised by sclerosis and loss of elasticity of the alveolar bone thereby causing undue resistance to add to the difficulties.
Another common cause is ill-fitting forceps, which impinge on the crown or do not fit the root accurately. Forceps may be misapplied, particularly on rotated, inclined or misplaced teeth. The use of excess force or short, jerky movements prevents the surgeon feeling which way the tooth wants to come and frequently results in fracture.
The management of retained roots has been discussed in Chapter 8. However, if certain principles are neglected the attempted removal of such roots may lead to more serious complications. It is essential that a radiograph is available to judge the presence of vital structures such as the antrum or mental nerve. Except where the crown has fractured at or above the level of the alveolar margin, it is bad practice to use forceps up the socket as the limited access makes it difficult to open the beaks sufficiently to grasp the root. If forceps are applied knowing that one or both blades are outside the alveolus, this bone will be severely damaged in order to deliver the root. The use of luxators may further expand the alveolus to allow elevation or safe application of root forceps.
The transalveolar approach must always be used wherever the root is not clearly visible or supporting tissues will be damaged. It is safe, leaves the tissue in good condition and, if regularly practised without delay, is economic in time.
Loss of Tooth or Roots
As the teeth and roots are extracted they should be carefully placed in a special container, and care should be taken not to carry them back into the mouth by accident. At the end of the operation, particularly under general anaesthesia, they should be counted and the number checked against the chart.
Where during extractions a tooth or root is lost, the surgeon should stop operating immediately and conduct a systematic search.
The Mouth
All the recesses of the mouth, under the tongue and recent sockets are examined. In patients under general anaesthesia, the posterior aspect of the tongue and oropharynx are searched too. After this has been done the superficial layers of the throat pack may be drawn forward lest it be lying there. The pack should not be removed completely till the end of the operation.
Spittoon and Suction Apparatus
The spittoon should always have a trap, and the suction apparatus a bottle in the circuit to stop fragments of tooth disappearing down the drain. The suction tip, tubing and other connections should be washed through as they often trap root apices.
Alimentary Tract or Lungs
Roots or teeth may be swallowed or inhaled. Whenever it is suspected that this may have happened, radiographs of the chest should be taken to ensure the tooth is not in one of the bronchi (usually the right). Swallowed fragments seldom give cause for anxiety as they should pass through the gut without incident, but if inhaled into the lungs the patient must be referred, without delay, to a thoracic surgeon for removal by bronchoscopy.
Under the Mucoperiosteum
Roots and occasionally teeth can be displaced under the periosteum, particularly in the posterior maxilla, or the mandible where there has been gross recession of alveolar bone or flaps have been raised past the reflection of the mucous membrane. A finger should be placed at once below the root and kept there to prevent it going deeper. A flap may be raised to expose the root, which can then be lifted out using a blunt hooked instrument. Attempts should not be made to grasp it with forceps as if they fail to grip the root they may drive it deeper into the space.
The Tissue Spaces
In the mandible, roots or teeth can be lost in the tissue spaces of the floor of the mouth either above or below the mylohyoid muscle. The lower third molar roots can be pushed down lingually through the bottom of the socket if this is deficient, as does occasionally occur; the root then lies below the mylohyoid. During the extraction of the unerupted lower third molar it can be elevated lingually into the tissue spaces. In all these cases the grave danger is that the tooth will pass into the deeper planes of the neck as a result of gravity and movements of the muscles. Without delay a finger must be placed either extra- or intraorally to stop the tooth moving. A flap may then be raised to explore the tissue space when the tooth may be ‘milked’ out or removed as described for those under the periosteum. When the tooth is lying superficial to the mylohyoid, removal is better delayed to allow an extraoral approach, followed by a blunt dissection up to the tooth.
The unerupted upper third molar can be elevated distally into the soft tissue space behind the tuberosity of the maxilla to lie in the pterygomandibular space. This is explored through an incision made down the anterior border of the ascending ramus of the mandible.
Bone Cavities
The roots of the maxillary second premolar, first, second and third molars, and occasionally the first premolar are related to the maxillary sinus, into which they can be displaced during extraction. Unerupted and supernumerary teeth may be related to the floor of the nose. Lower apices can be pushed into the inferior dental canal. In both jaws roots can be driven into pathological cavities such as cysts or abscesses. Where it is suspected that a root is lost in a bone cavity the operation is stopped and radiographs are taken in two planes at right angles to each other in an effort to localise the lost root or tooth.
Roots displaced into the inferior dental canal are removed by a transalveolar approach, care being taken not to damage the inferior dental nerve. They should not be left as they may give rise to infection or pressure symptoms of paraesthesia or anaesthesia. Roots pushed into the nose, if they lie under the mucous membrane, are usually easily recovered through the socket, or through the anterior nares if they are lying in the nasal cavity.
Oroantral Communication
The relationship of the apices of the maxillary premolar and molar teeth to the maxillary sinus is variable and depends on individual anatomy and the age of the patient, as pneumatisation of the sinus continues throughout life. Often the antrum dips down between the roots of the molar teeth, which virtually form part of the antral floor.
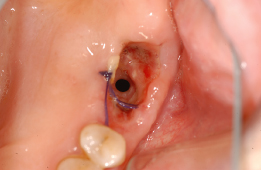
Occasionally the uncomplicated extraction of a tooth may fracture the thin floor of the sinus and cause an oroantral communication (OAC). Apical infection can destroy the bone over the apex, bringing an apical granuloma into contact with antral lining, which is then torn by the extraction of the tooth. Infection in the maxillary sinus may also predispose to the establishment of a fistula. More commonly the communication is produced by attempts to remove retained apices so that the antrum floor is perforated or the apex displaced into it. An oroantral fistula (OAF) is established if the communication becomes epithelialised (Figure 10.1).
Figure 10.1 Oro-antral fistula.
Signs and Symptoms
The patient will complain of air passing from the nose into the mouth and the operator will be able to see this bubbling through the communication, particularly when the patient is asked to breathe out. Blood from the wound and mouthwashes used to rinse the mouth may pass through the sinus into the nose. A blunt probe passed very gently into the socket will be found to penetrate into the maxillary sinus. This last test should rarely be performed as it may create a communication. Established fistulae tend to reduce in diameter but the track from mouth to sinus frequently fails to heal spontaneously and becomes epithelialised. When this is large the patient complains that drinks pass from the mouth into the nose, that cigarettes are inhaled with difficulty, and that air passes into the mouth. As the hole shrinks it remains a pathway for infection, but fails to provide adequate drainage for the sinus so that often the symptoms of acute sinusitis are superimposed on those of a fistula. The aim of treatment is to re-establish the normal drainage />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


