Chapter 16
Surgical Treatment of Salivary Gland Disease
- Presenting complaints
- The minor salivary glands
- The major salivary glands
- Specific conditions
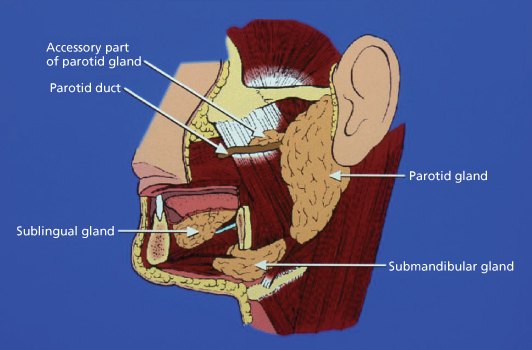
The salivary glands comprise the paired major parotid and submandibular glands located on the side of the face, together with bilateral sublingual glands in the floor of the mouth and the numerous minor salivary glands distributed intraorally (Figure 16.1). Disorders of salivary glands treated by surgery include cysts, salivary calculi, infections and tumours.
Figure 16.1 Diagram illustrating anatomical location of the major salivary glands.
Presenting Complaints
Salivary gland disease may present as acute inflammatory gland swellings, such as a viral or bacterial sialadenitis, recurrent swellings associated with mealtimes due to duct obstruction or stricture secondary to calculi, persistent diffuse whole gland enlargement as seen in Sjogren’s syndrome or sialosis (a non-inflammatory, non-neoplastic enlargement seen in diabetes, alcoholism or anoxeria), or as nodular, intraglandular swellings suggestive of tumour or cyst formation (Box 16.1).
Box 16.1 Classification of Salivary Gland Disorders
| Congenital | Aplasia |
| Hypoplasia | |
| Inflammatory | Sialadenitis – viral or bacterial infection |
| Autoimmune – Sjögren’s syndrome | |
| Idiopathic – necrotising sialometaplasia | |
| Sarcoidosis | |
| Traumatic | Mucocele, ranula |
| Salivary fistulae | |
| Post-irradiation sialadenitis | |
| Obstructive | Sialolithiasis |
| Atresia or ductal stenosis | |
| Tumours | Benign – pleomorphic adenoma |
| Malignant – mucoepidermoid carcinoma, acinic cell carcinoma, adenocarcinoma, adenoid cystic carcinoma | |
| Idiopathic | Sialosis |
If a patient reports the appearance of a mass, the size and growth rate should be recorded, together with how long it has been present and the presence or absence of other symptoms. Rapidly growing, painful masses with symptoms such as facial nerve palsy, trismus and bony destruction are suggestive of malignant tumour progression, while a symptomless, slow-growing swelling is more likely to be benign. In addition, any change in consistency of the saliva or taste sensation should be noted and it is important to ascertain if there is involvement of other systems such as the eyes, liver, lungs or joints.
The Minor Salivary Glands
Cysts
Diagnosis and Presentation
Common sites include the lips, cheeks, floor of the mouth and palate. The cause is usually trauma, especially cheek or lip biting which may lead to stenosis or rupture of the duct and accumulation of saliva. They are common in children and young adolescents. The types include the mucous extravasation cyst and mucous retention cyst. In the former, mucus ruptures through the duct and pools in the adjacent connective tissue; there is no epithelial lining and the saliva is contained by flattened connective tissue. In the latter, mucus is still contained by the epithelium lining the duct, which swells to form an epithelial-lined cyst (Figure 16.2).
Figure 16.2 Salivary mucocele of lower lip.

Signs and Symptoms
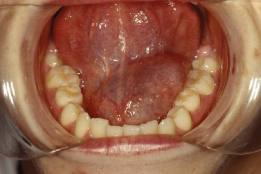
These cysts usually present as painless, smooth, bluish swellings containing fluid. At intervals they burst, discharging their contents, but if untreated they heal and form again. In the floor of the mouth, a cyst may arise from the sublingual gland and grow to a considerable size and is called a ranula (Figure 16.3).
Figure 16.3 Ranula (mucocele) in the floor of mouth.
Treatment of Cysts
Mucocele
Treatment involves delicate enucleation. An incision is made by drawing a scalpel blade lightly over the swelling and through the mucosa for a short distance beyond the lesion on each side. Alternatively an elliptical incision can be made to reduce the chance of rupture. The cyst is gently freed by blunt dissection and the gland concerned is also removed to prevent recurrence. Due to the fragile lining the lesion may burst during surgery. Other glands seen in the wound, which may already be traumatised, should be removed lest their ducts become blocked by scar tissue and give rise to new cysts. Primary closure is achieved by using superficial mucosal sutures.
Ranula
The ranula is more difficult to treat and care must be taken during floor of mouth surgery to avoid damage to the submandibular duct and lingual nerve. It is usual to have to excise the sublingual gland as part of this procedure and surgery is best carried out under general anaesthesia. More rarely, a ranula may extend through the mylohyoid muscle (a ‘plunging ranula’) into the upper neck requiring both intraoral and cervical approaches to facilitate complete removal.
Tumours
(See Chapter 15)
The commonest tumours to arise from minor glands include the benign, but locally invasive, pleomorphic adenoma and the malignant adenoid cystic and mucoepidermoid carcinomas (Figure 16.4). It is worth remembering that malignant tumours arise more commonly in minor salivary glands than in major glands, so intraoral glandular swellings should be regarded with suspicion.
Figure 16.4 Pleomorphic salivary adenoma in the palate. An incisional biopsy has been performed.

Diagnosis
The pleomorphic adenoma occurs most frequently, with many arising as palatal swellings or nodular submucosal swellings within the upper lip or buccal mucosa. It presents as a painless swelling of rubbery consistency, which may be fixed to either the overlying mucosa or the deeper structures. In the palate it is usually found to one side of the midline near the junction of hard and soft palate and may reach a large size.
The adenoid cystic and mucoepidermoid carcinomas may clinically resemble a pleomorphic adenoma but usually display more rapid growth, pain and ulceration of the surface mucosa.
Treatment
The pleomorphic adenoma is treated by excision with a margin of normal tissue because tumour outgrowths may be found within or outside the tumour capsule. Large defects may require a skin or mucosal graft, or rotational flaps or an oversown pack. Adenoid cystic carcinomas may spread far along the perineural lymphatics so that wide resection and reconstruction is necessary. Unfortunately, metastatic blood-borne spread may occur, leading to pulmonary tumour deposits. Mucoepidermoid carcinomas may be of low- or high-grade malignancy but again require wide excision. Radiotherapy is not often used because of the relatively slow growth rate and resultant radioresistance of salivary gland cancers.
The Major Salivary Glands
Disorders of the major salivary glands requiring surgery include obstructions to salivary flow, infections and neoplasms. The surgical procedures available to treat these disorders are listed in Box 16.2.
Box 16.2 Surgery of the Major Salivary Glands
- Removal/Destruction of calculi
- Duct dilatation or repositioning
- Excision of sublingual gland
- Excision of submandibular gland
- Parotidectomy: superficial, total
Investigation of Major Salivary Glands
Presentation and Diagnosis
The clinician should record the presence of pain, swelling, altered salivary flow and a bad taste. The periodicity and duration of the swelling is ofte/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


