Chapter 13
Treatment of Cysts of the Jaw
- Diagnosis
- Treatment
- Developmental cysts of non-dental origin
- Non-epithelial lined cysts
- Soft tissue cysts
A cyst may be defined as a radiolucency that is usually fluid filled and has a lining. The lining is frequently epithelium and in the mouth is either of dental or non-dental origin. A cyst must be differentiated from other pathology that might mimic it, particularly neoplasia.
The common cysts of the jaw arising from epithelium of dental origin are:
- dental (radicular) or periodontal cysts
- residual cysts
- dentigerous cysts
- eruption cysts
- keratocysts.
Dental (Radicular) or Periodontal Cysts
These form from the epithelial cells or rests of Malassez, which are the remnants of Hertwig’s sheath. They remain throughout life, scattered in clusters, in the periodontal membrane. Chronic infection may stimulate them to proliferate and form epithelial lined cysts in the jaws. These occur chiefly over the apex of a dead tooth, but may occasionally be found on its lateral aspect, when they are called lateral periodontal cysts.
Residual Cysts
These occur in edentulous areas of the jaws and are dental cysts believed to have been present before the dead tooth was extracted and which continue to grow.
Dentigerous Cysts
These form between the reduced enamel epithelium of the follicle around a developing tooth and its crown. The cyst lining is therefore attached to the tooth at the amelocemental junction.
Eruption Cysts
These are cysts forming over erupting teeth and they have a dentigerous relationship also. Those over deciduous or permanent teeth with no deciduous predecessor are believed to originate from the cells of the enamel organ. Where there has been a deciduous predecessor, the epithelial rests of Malassez from this tooth could give rise to one of these cysts.
Cyst Growth
Osmotic Growth
The above cysts of dental origin are believed to increase in size either from continual liquefaction of their shed cells (which forms the cholesterol that gives the contents a characteristic golden appearance) or as a result of the positive osmotic pressure of the hypertonic contents that draws water in from the tissues.
Mural Growth
Direct growth of the epithelium lining the cyst wall from which keratin squames are shed is a characteristic of keratocysts (see below). This ability to grow means that if any lining remains recurrence is more likely.
Keratocysts (Primordial Cysts)
These are said to arise from the dental lamina or from the enamel organ of a tooth germ. Their lining is of well-differentiated epithelium which may show ortho- or parakeratosis. They are believed to increase in size by mural division. Beneath the epithelium is thin fibrous tissue, which is easily torn, and satellite cysts lying outside the main body of the lesion are often found. For these reasons keratocysts are well known to be difficult to eradicate and likely to recur after treatment. The recurrence rate has been reported to be anything between 5 and 60%. The complete removal of all the lining of these cysts to avoid recurrence is of great importance. Their contents have less soluble protein (below 5 g/100 ml) than dental cysts.
Diagnosis
Diagnosis on clinical grounds alone should be treated with caution. Histological confirmation of any diagnosis should be vigorously pursued (Figure 13.1).
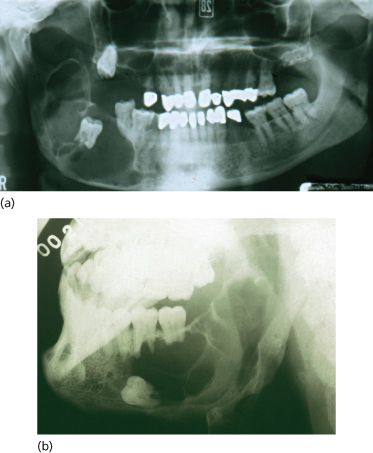
Figure 13.1 Diagnostic difficulties. (a) Histologically this lesion was a dental cyst; (b) this lesion was an ameloblastoma.
Presentation
In many cases the presentation is on routine radiograph. The process of diagnosis follows established routines.
History
The patient often gives no history, as many cysts may escape attention until they become infected. Larger cysts may cause swelling of the jaw or face, which in the edentulous may be associated with difficulty in wearing dentures. In the mandible, pressure on the inferior dental nerve almost never gives rise to mental anaesthesia or paraesthesia, an important point in differentiation from tumours. Occasionally cysts reach such proportions that excessive resorption of bone leads to pathological fracture. Eventually the majority of cysts become infected, with acute symptoms and, in those that have expanded into the soft tissues, an increase in the swelling.
Examination
Uninfected dental, residual or dentigerous cysts are painless and non-tender on palpation. When they are small and enclosed in bone they show no change in the form of the alveolus. Larger cysts cause a marked, smooth, rounded expansion of the bone, which may be reduced to a thin layer of cortical plate. This, if pressed, is resilient but may fracture and give rise to egg-shell crackling. In the mandible this expansion is said to take place buccally only, but occasionally it is seen lingually as well. Where the cyst has invaded the soft tissues the swelling is found to be fluctuant and a definite thrill can be made to pass through it. At this stage, if the mucous membrane covering is thin, it will have a bluish colour (Figure 13.2). An eruption cyst presents as a small blue swelling in the gum over an unerupted tooth. Infected cysts have all the classical signs of acute infection and may present with a sinus discharging pus.
Figure 13.2 A dentigerous cyst around the unerupted lower right third molar. Note the blue colour due to the fluid content of the cyst.

Missing teeth must be charted and the standing teeth carefully examined for caries, periodontal disease and mobility. A dentigerous cyst may be suspected where a tooth is missing from the arch without any history of previous extraction. Dead and root-filled teeth are associated with dental cysts. The vitality of all teeth near the lesion must be tested with an electric pulp tester and the results compared with similar teeth on the unaffected side. If there is any delay between diagnosis and operation these tests should be repeated immediately before operation, for cysts not only arise from dead teeth but their expansion may also devitalise adjacent teeth.
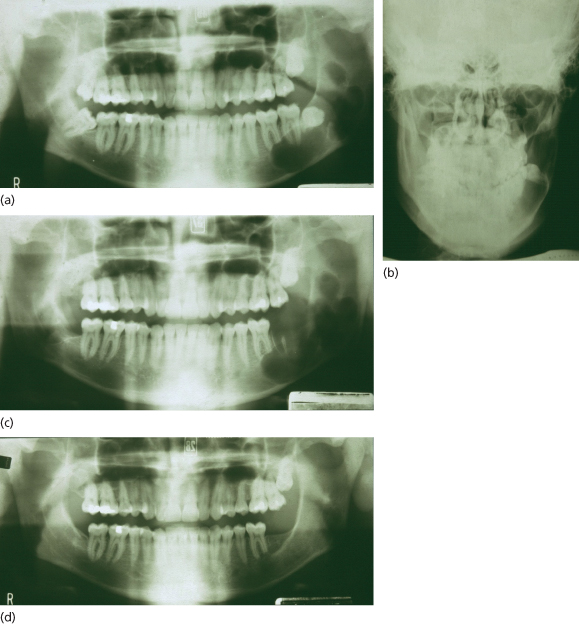
Keratocysts may present like dental cysts but occur most commonly in the lower third molar region or distal to it and invade the ascending ramus extensively. They tend to expand anteroposteriorly in the medullary bone of the mandible and reach some size with minimal expansion of the cortical plate. Diagnosis may result from an infective episode or as a result of discovery on a scanning radiograph (Figure 13.3).
Figure 13.3 Keratocyst. (a, b) At presentation; note resorption of apex of first molar; (c) immediate postoperative appearance; (d) appearance at 6 months showing bone healing. Inferior alveolar nerve function was not affected.
Gorlin–Goltz Syndrome
Multiple recurrent keratocysts are associated with basal cell carcinomas and some skeletal abnormalities in this syndrome. These patients require careful management and appropriate referral when necessary. Recurrence of the cystic lesions in this syndrome requires regular reviews and radiography to identify lesions early and reduce morbidity.
Radiography
Intraoral apical films usually suffice for small dental cysts. Larger ones may need extraoral and occlusal views of the jaws to show their full extent. This is demonstrated by radiographs taken in two planes, as treatment planning depends on a clear understanding of their size and their relationship to those vital structures on which they may encroach.
Cysts appear as rounded, radiolucent areas sharply demarcated from normal bone by a thin, radiopaque, limiting line of compact or cortical bone (Figures 13.1 and 13.3). This line is not usually present on radiographs of apical granulomas and is often absent or hazy round infected cysts. Apical periodontal cysts are associated with the roots of dead teeth and may throw a shadow over or displace the roots of neighbouring teeth, which, though apparently involved, may yet still be vital. Dental cysts, particularly the keratocyst, if loculated may simulate ameloblastoma (Figure 13.1) or central giant cell reparative granuloma.
In the maxilla it is sometimes difficult to tell whether a radiolucent area is a cyst or a locule of the maxillary sinus. Therefore it is necessary to compare the radiographs with those of the opposite side; if a similar locule is present the radiolucent area is probably part of the sinus. If all the teeth are standing and vital, a cyst is unlikely to be present. Finally, where doubts still exist, the area may be aspirated and if air, not fluid, is withdrawn it is certainly part of the maxillary sinus.
CT Scan and cone beam CT (CBCT)
If further imaging information is required computerised tomography (CT) can be very useful, especially in the maxilla. Interference with metal restorations can cause scatter of the rays and a more confusing picture. Cone beam CT (CBCT) can restrict the radiation dose and give very clear local information as regards integrity of surrounding bone. The digital image can be manipulated to give an apparent 3-D picture.
Aspiration
An aspirating syringe with a broad-bore needle is used, as the contents can be quite thick. Uninfected cysts should not be aspirated more than 24 hours before operation to avoid introducing infection. In those covered by thick bone it may be better delayed till, at operation, a flap has been laid back and bone removed.
All cysts of any size should be aspirated if possible before operation. It is an important diagnostic measure that can save the surgeon much embarrassment from accidentally opening a solid tumour, or worse a central haemangioma. Microscopic examination of the aspirate may show the presence of cholesterol.
Further, only in this way may a keratocyst be differentiated from other odontogenic cysts before operation. This is done by electrophoresis of the aspirate, which for keratocysts will show less than 5 g in 100 ml of soluble protein, whereas other dental cysts will have quantities similar to that in the patient’s serum.
Differential Diagnosis
These lesions may all mimic cysts in their radiographic appearance:
- solitary bone cyst
- Stafne’s bone cavity
- aneurysmal bone cyst
- central giant cel/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


