Chapter 10
Case Presentations
Aim
The aim of this chapter is to present “real life” patients to illustrate the principles of orofacial pain (OFP) diagnosis and management.
Objectives
At the end of this chapter, the practitioner should:
-
recognise the diversity of OFP signs and symptoms
-
be familiar with the approach to diagnosis of OFP.
Case 1: “My Pain is so Bad I Want to Kill Myself”
Complaint
A married, 36 year-old male was referred by an ENT surgeon, complaining of right-sided facial pain. The patient complained of severe bouts of right-sided temporal and infraorbital pain that had started six weeks prior to his consultation. He had a history of a temporomandibular disorder (TMD). No specific aggravating or relieving factors were identified. He was hospitalised under the care of the ENT consultant and received multiple assessments from a maxillofacial surgeon, a dental practitioner and a dermatologist. The pain occurred in bouts lasting 90–180 minutes and were associated with visual disturbance. There was no specific temporal pattern, the bouts occurring predominantly during the day but also waking him from his sleep. There was no prior history of facial pain of similar intensity.
Investigations including magnetic resonance imaging (MRI) of the brain and computed tomographic (CT) scans of the sinuses and neck were unremarkable. A right temporomandibular joint (TMJ) steroid injection partly reduced his discomfort.
Clinical Examination
There was a marked restriction associated with the patient’s range of jaw opening. Comfort opening measured 15 mm. There was tenderness associated with the TMJs and associated masticatory and cervical muscles, in particular the masseter, temporalis and sternocleidomastoid muscles.
During the course of the clinical examination, the patient developed a bout of severe right-sided facial pain. This duplicated his principal complaint. He curled up in a ball on the dental chair and rocked his body forwards and backwards. His right eyelid drooped (ptosis) over his right eye and resulted in visual disturbance (Fig 10-1). He was unable to concentrate or converse because of the severity of the pain.

Fig 10-1 A cluster headache sufferer presenting with ptosis of the right eye.
Investigation
A trial of sumatriptan (20 mg/ml) nasal spray was administered. The pain subsided within 10 minutes and the visual disturbance also subsided. He was able to converse intelligibly and reported that over that short period of time his pain reduced from a 10/10 to a 2/10 as assessed by a visual analogue scale (VAS).
Diagnosis
The patient was diagnosed as having episodic cluster headaches. He also had bilateral TMJ capsulitis and myofascial pain that were precipitated by a stress-induced parafunctional behaviour. Once the patient’s headaches were stabilised, his TMD symptoms subsided.
The patient was started on a preventative course of verapamil but was unable to tolerate the side-effects. He was switched to topirimate 25 mg at night. Sumatriptan was used as his rescue medication. Initially he used this four times per week. The frequency of his headaches reduced. After three weeks his pain subsided completely. He continued to take topirimate for a further month and this medication was then tapered off. He remained pain free.
Discussion
Cluster headache is a syndrome with a prevalence of approximately 0.1% and characterised by trigeminal distribution of pain. A significant proportion of cluster headache sufferers attending a dental practitioner for relief go undiagnosed. Many patients are treated for dental pain, TMD or sinus pathology before an accurate diagnosis is made. Usually young males (20–40 years of age) tend to present with this condition. There are three classical features of cluster headache.
-
The pain is intense (graded as a 10/10) and strictly unilateral; unlike migraine, cluster headaches sufferers will want to move about. Often they will rock back and forth, pace the room or even bang their head against the wall. It has been referred to as “suicide headache” because of this intensity.
-
The pain duration is longer that trigeminal neuralgia (seconds–minutes) and shorter than migraine headaches (hours–days). Typically, a cluster headache will last for 15 minutes to three hours. It can have an abrupt onset and cessation.
-
The pain is associated with autonomic features such as conjunctival injection, ptosis, miosis, eyelid oedema, lacrimation, rhinorrhoea, nasal blockage and facial sweating.
Case 2: “Is It All in my Head?”
Complaint
A married 54-year-old female presented complaining of a two-month history of left-sided facial pain. She experienced an intense superficial lancinating pain radiating across her left cheek, leaving a tingling sensation on her face. It was closely associated with the left maxillary and mandibular region and was graded as a 7/10. It had an irregular presentation with no specific temporal pattern. The pain lasted for seconds before subsiding. In general, there was one episode a day. Aggravating factors included speaking, eating and yawning. Relieving factors included jaw rest. There was reduced hearing and a blocked sensation associated with the left ear. As a consequence, the patient would always put the telephone to the right ear, even though she was left-handed.
The patient initially attended her dentist. Two large old amalgam restorations were removed from her maxillary and mandibular first molar teeth. These teeth were dressed with a sedative material. There was no change in her pain. She then attended her medical practitioner. A thorough otoscopic examination was normal.
Clinical Examination
Intraoral examination was normal. Tooth Slooth and vitality testing failed to reveal any abnormality. Extraoral examination was unremarkable. There was no TMJ tenderness. Mandibular movements were smooth and regular. There was no clicking or crepitation. There was no masticatory muscle tenderness. There was no temporal tenderness or swelling. Corneal reflex was intact. Light touch and pinprick examination of the trigeminal divisions was equal and symmetrical. There were no trigger zones.
Investigations
Panoramic and periapical radiographs were unremarkable. A brain MRI was performed (Fig 10-2). This revealed an enlarged mass in the cerebellopontine angle. The patient was diagnosed with an acoustic neuroma, compressing the left trigeminal and vestibulocochlear nerves.
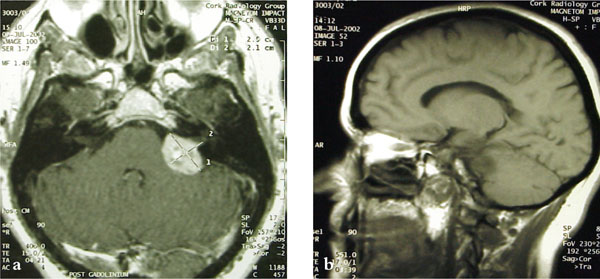
Fig 10-2 Acoustic neuroma as seen in a magnetic resonance image with gadolinium enhancement. (a) The coronal view revealed an acoustic neuroma in the left cerebellopontine angle (b) The sagittal section showed a shadow in the left cerebellopontine angle.
Diagnosis
Symptomatic trigeminal neuralgia caused by the neuroma was the diagnosis.
Discussion
It is estimated that 15% of patients with trigeminal neuralgia have pathology that compresses the trigeminal nerve. This often occurs in the cerebellopontine angle, which is located at the junction of the cerebellum, pons and medulla. The trigeminal nerve exits the brainstem in this region and is intimately related here to the facial nerve, the vestibulocochlear nerve and the cerebellum. An acoustic neuroma, also known as a schwannoma, is a benign slowly-growing tumour arising from the Schwann cells of the vestibular portion of the vestibulocochlear nerve. These tumours infiltrate the internal auditory meatus, gradually enveloping the auditory and vestibular divisions of the vestibulocochlear nerve, the facial nerve and the trigeminal nerve. Because these tumours may become quite large before they are diagnosed, a constellation of symptoms can be produced subsequent to compression of the adjacent cranial structures. These symptoms are listed in Table 10-1. Diagnosis requires imaging, preferably an MRI scan. Treatment is typically surgical.
| Compressed structure | Clinical presentation |
|
Trigeminal nerve |
|
|
Facial nerve |
|
|
Vestibulocochlear n/> |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


