1
Vascular Response to Injury
The vascular response to injury is a reactionary process that sets up the “delivery system” of inflammation. What is needed at the site of an injury is a way to deliver supplies and materials for defense. By initially opening up the vascular delivery system, more supplies and materials are shipped into an area than would normally pass that way. Without something else, however, the supplies would rapidly pass right on by. Therefore, the system builds in a slowing-down process once the supplies are on location. Finally, the system must get the supplies unloaded from the delivery system and across the country to the injury site.
Injury to an organ or tissue results in progressive changes in the damaged area. The main signs of such a response are redness, heat, and swelling. These signs are the result of vascular alterations in the area of injury. The redness and heat result from an increase in blood flow, which in turn is the result of vasodilatation, first involving arterioles, and then capillaries and venules. Swelling is the result of alterations in vascular permeability leading to exudation of fluid, plasma proteins, and white blood cells.
Quick review
Certain blood vessels are involved in the response to injury. These vessels constitute the microvasculature. Since numerous references will be made to these vessels in the first section of this book, a quick review is in order (Fig 1-1).
Arteriole: Smaller than an artery, it consists of an inner layer of endothelial cells, a middle layer in which there is at least one layer of smooth muscle, and an outer layer of adventitia.
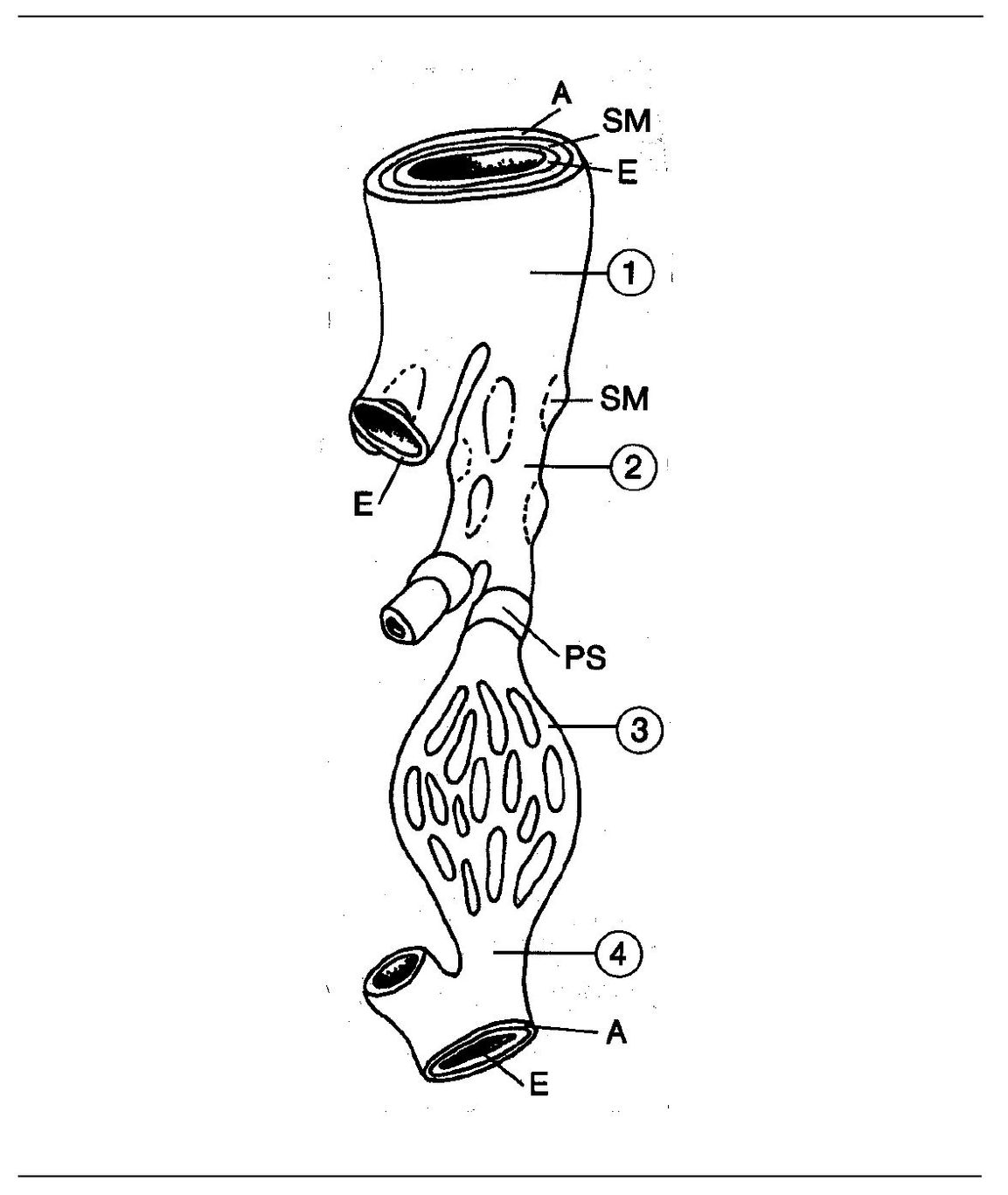
Fig 1-1 Microvasculature. (A) Adventitia; (SM) smooth muscle; (E) endothelium; (PS) precapillary sphincter; (1) arteriole; (2) metar-teriole; (3) capillary; (4) venule.
Metarterioles: Branches of arterioles that are similar to capillaries except for the presence of muscle fibers that encircle the lining of endothelial cells. The muscle fibers do not form a continuous layer but tend to occur in groups.
Precapillary: May arise from either an arteriole or a met-arteriole and is distinguished by the presence of a few muscle fibers that form a sphincter around the underlying endothelial cells.
Capillary: The structural unit of the circulatory system. Except for the capillaries, the blood is normally contained within relatively heavy-walled, impervious tubes. Even in the capillary network the plasma and cells of the blood are sepa-rated from the tissues they serve by a thin sheet of endothelial cells that form the capillary wall. Fluid and metabolites are transported through the walls of the capillaries and reach the tissues by diffusion. Capillaries are surrounded by a basement membrane.
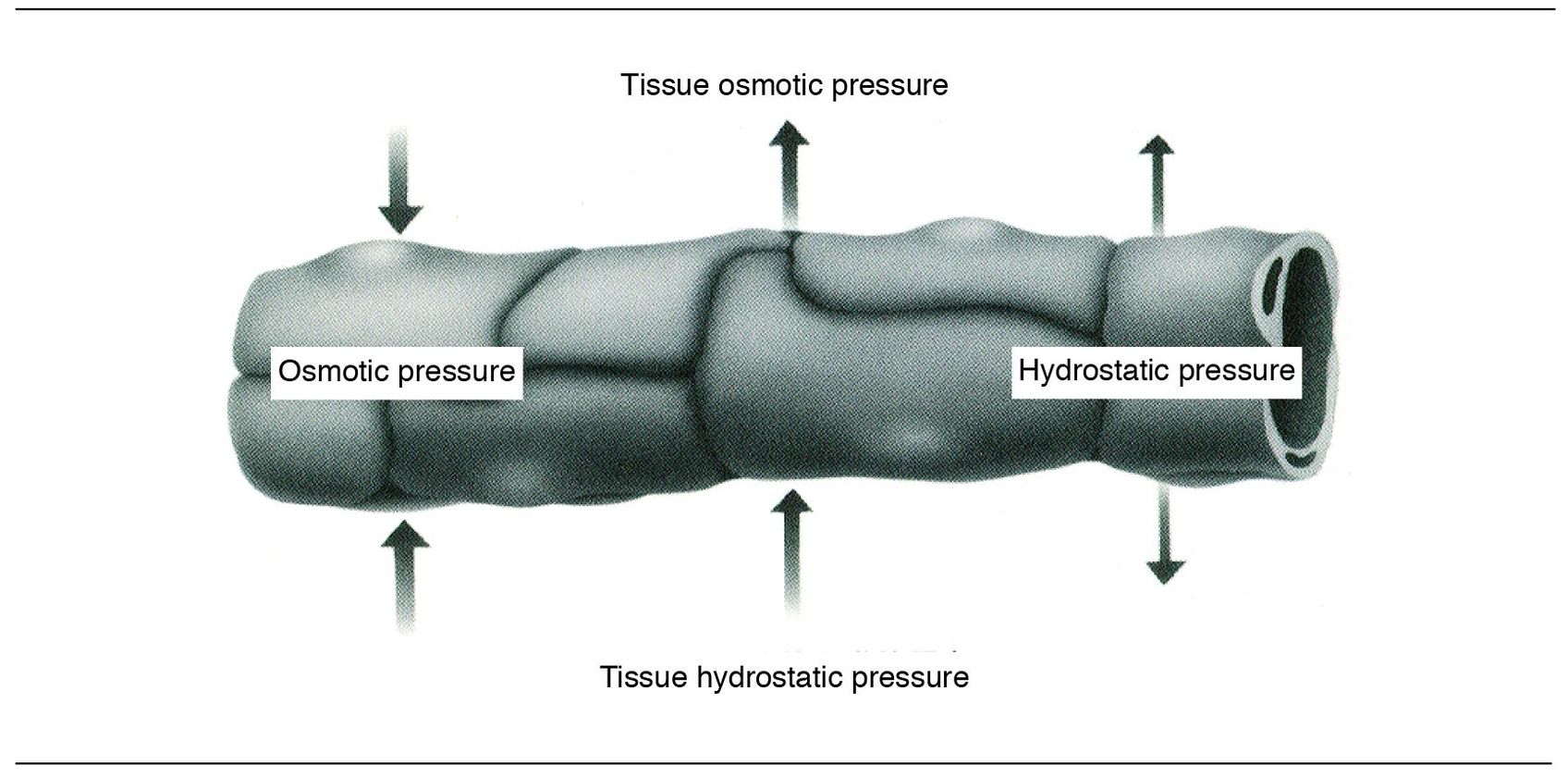
Fig 1-2 Fluid exchange across walls of small blood vessels.
Venules: Blood is drained from the capillaries by these vessels. They possess a basement membrane and an adventitia but lack smooth muscle fibers.
Starling’s law
The movement of fluid in and out of arterioles, capillaries, and venules is regulated by the balance between intravascu – lar hydrostatic pressure, which tends to force fluid out of the vessels, and the opposing effects of osmotic pressure exerted by the plasma proteins, which tend to retain fluid within the vessels (Fig 1-2). This is often referred to as Starling s law.
The vascular events
Vasodilation
Following a very brief period of vasoconstriction, the arterioles dilate (vasodilation, Fig 1-3) and the microvasculature at the site of injury becomes filled with blood (congestion). Thus, the process of increased “delivery” is set in motion. This process is known as active hyperemia.
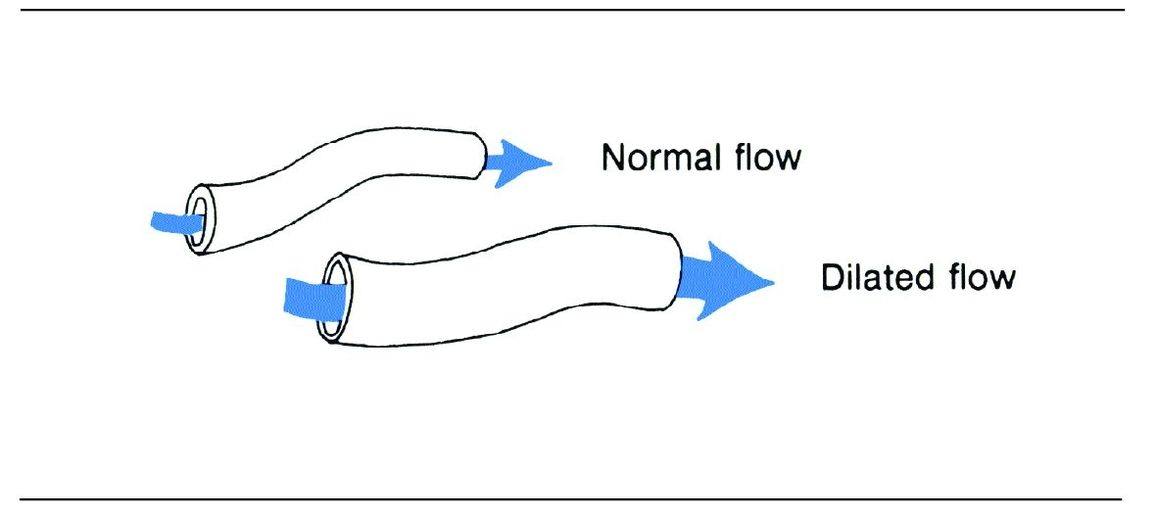
Fig 1-3 Vasodilation.
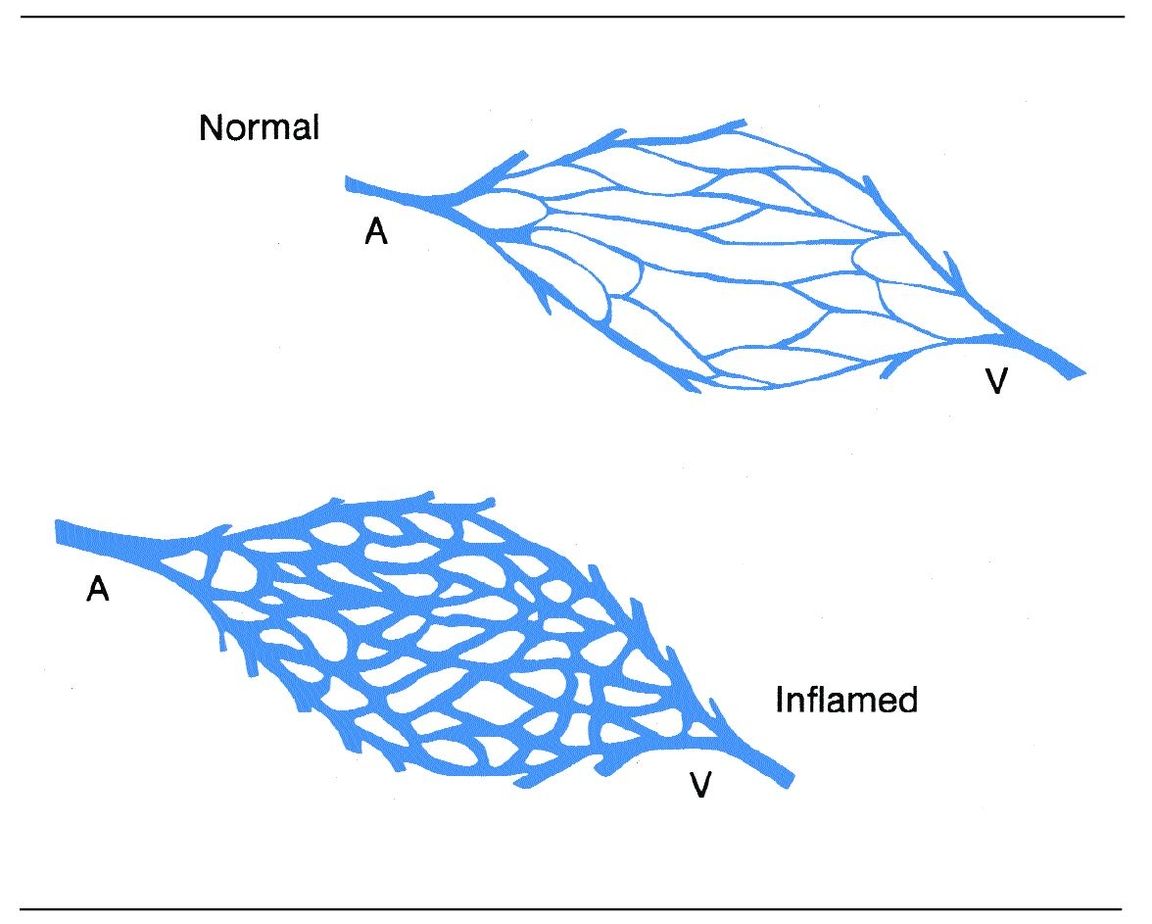
Fig 1-4 Increase in blood flow associated with inflammation. (A) Arteriole; (V) venule.
Vasodilation results from a relaxation of the smooth muscle layer of arterioles and the sphincter of precapillaries. This opens previously inactive capillaries and may result in as much as a tenfold increase in blood flow in the injured area (Fig 1-4). Postcapillary venules dilate as more blood flows in through the capillaries.
Increased vascular permeability
From the thousands of letters we have received about vas – cular permeability it is clear that you want to know why a vessel becomes leaky. Your long wait is over….
Vessels become leaky for a couple of reasons (more detailed discussion later). For now, you should know that first the vessel dilates. The cells of the endothelium, which make up the inner layer, then contract. (This happens only in small postcapillary venules.) When the endothelial cells contract and draw away from each other, gaps form between the cells through which fluid and plasma proteins can move (Fig 1-5).
Another mechanism by which vessels may become more leaky is through an injury that causes destruction of endothelial cells but does not damage the basement membrane that surrounds the vessel. (If the basement membrane remains intact there is no hemorrhage.) Now this is more of the use – ful information we promised to deliver. Next time you see a bruise on your squash partner s leg, you can comment with assurance, “Oh . . . I see your basement membrane was not intact!” As he tries to figure you out, you can probably nail down a couple more squash points. This destruction of endothelial cells can occur in capillaries and arterioles, as well as in venules.
- In mild injury it is principally the postcapillary venules that become more permeable.
- In moderate injury the capillaries as well as the small venules become more permeable.
- In very severe injury the capillaries, venules, and arterioles may all become leaky.
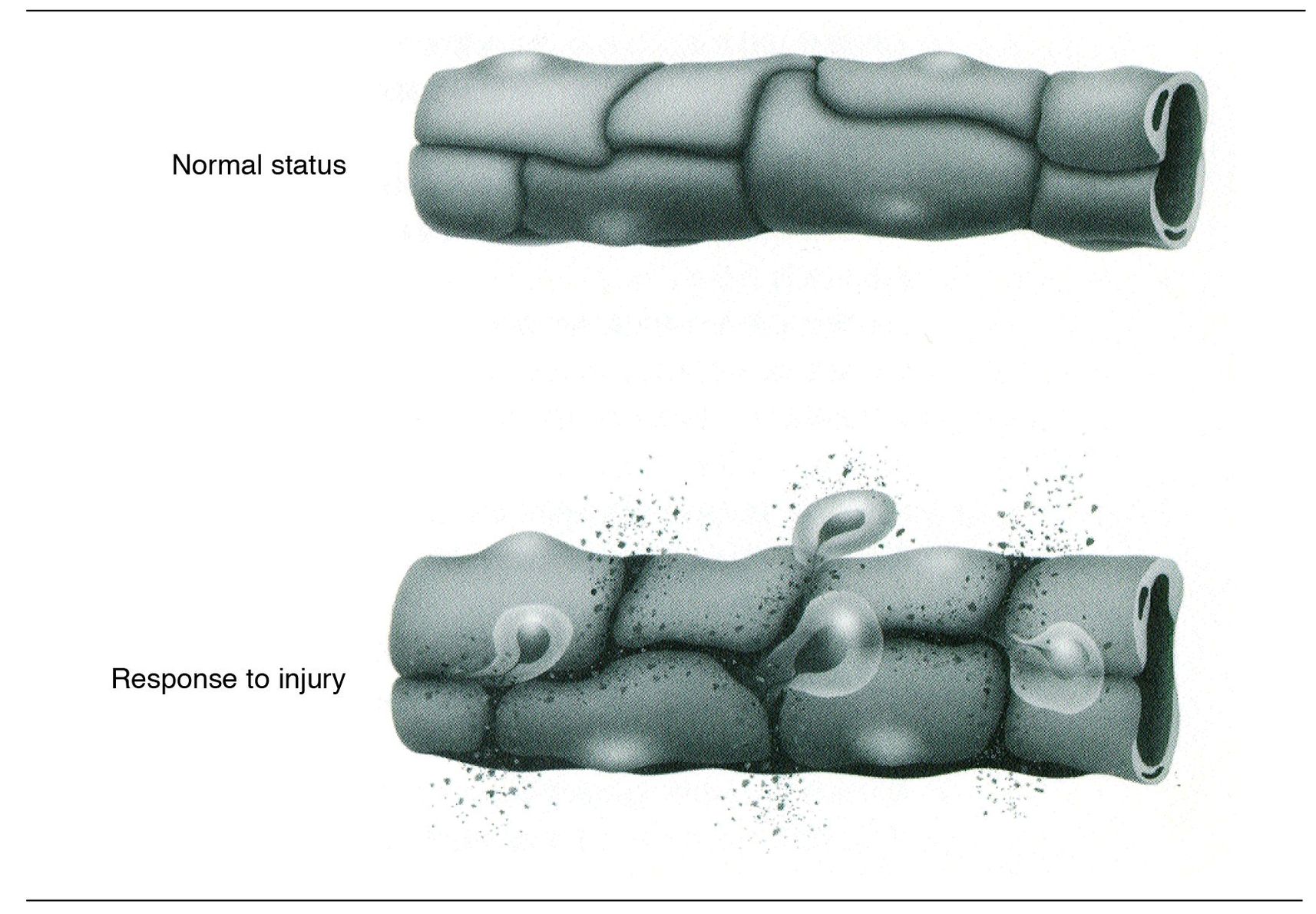
Fig 1-5 Intercellular gaps.
Now you can see why the pattern of vascular permeability is known to be related more to the intensity of the injury than to the nature of the injury.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


