1
The Extraoral and Intraoral Soft Tissue Head and Neck Screening Examination
It is paramount that the dental clinician establish a repeatable, logical, sequentially organized, and systematic approach to screening the soft tissues of the head and neck region. It should be understood that this is not an “oral cancer screening,” since all abnormal conditions should be detected. Performing an oral cancer screening means looking for a single condition, cancer, at a single point in time; the dental clinician performs a complete exam, looking for all soft tissue abnormalities at a single point in time. There is no universally acknowledged step-by-step approach; therefore, the following is the one we adhere to and it can be modified as desired. The important point is, whatever sequence is established, it should be strictly adhered to each time to ensure that no step is omitted. A suggested ideal sequence of steps for a complete oral mucosal screening procedure of a new patient includes the following:
- Introduction to the patient
- Patient’s chief complaint
- History of the present illness
- Medical (including social) and dental histories
- Physical examination (to detect the site, morphology, and color of abnormalities)
- Review of data and formulation of a clinical differential diagnosis
- Additional clinical and laboratory tests ordered, as indicated
- Final definitive diagnosis with a treatment/management plan formulated
Certainly, the clinician should establish a pleasant rapport with the patient so that excellent communication and trust are established. Often, the most critical or important piece of information a patient possesses does not get transmitted to the many forms filled out at the initial dental appointment. Once the patient’s trust, confidence, and respect have been secured, the patient’s chief complaint must be established. This can be a specific dental problem or a more generic goal such as “I need a checkup exam.”
If the patient voices a specific reason for the dental appointment, it is very important to gather as much subjective information from him or her as possible. The collective sets of subjective information are the patient’s symptoms. Symptoms include descriptions such as pain, burning, dry mouth, soreness, swelling, roughness, and paresthesia. Whatever the symptom, its specific nature should be questioned, such as onset, duration, periodicity, nature or character, severity, and triggering factors or association. This information helps establish the history of the present illness. The clinician gathers a pocketful of diagnostic clues provided by the patient and combines them with the clinician’s pathology knowledge to guide him or her to ask appropriate and insightful follow-up questions. Thus, the clinician acts as a detective and must possess foundational knowledge of head and neck disease and pathology in order to learn more about the patient and gather more clues for the formulation of a well-honed clinical differential diagnosis. Subsequent chapters of this book provide foundational knowledge—both general and specific—of the most common soft tissue head and neck pathology.
Following determination of the history of the patient’s present illness, the medical history is reviewed with the patient. Typically, the patient has previously completed a detailed form providing the clinician with basic information about childhood diseases; vaccinations; hospitalizations and prior surgeries; any current medical care; date of the last physical examination; and medications (i.e., prescription and over-the-counter, including herbs) being taken or previously used, especially in the past 6 months. Details about the medications, including name, dosage, and duration of use, are recorded. A complete review of systems (e.g., cardiovascular, pulmonary, renal, endocrine, nervous system) is performed to gather more details than the initial “yes” or “no” responses. In addition, the medical history also includes the patient’s psychological and socioeconomic profiles as well as social habits (e.g., tobacco and alcohol abuse).
Next, the dental history, including details of any oral habits, is gathered. It is important to note decayed, missing, and restored teeth as well as any active caries; periodontal disease; history of extractions and other oral surgery procedures; tooth vitality status; and any need for patient premedication. Any previous problems during dental care are discovered and discussed. Oral habits include the patient’s technique and frequency of flossing, brushing, use of mouthrinse, and occlusal disharmonies.
Physical Examination
It is popular to compare the left and right side for bilateral symmetry while understanding that perfect symmetry is often not present within the range of normal. This is particularly important in order to visualize enlarged lymph nodes or parotid glands.
Extraoral Sites
Specific sites include the following:
- Hair and facial skin
- External eyes
- External ears
- Temporomandibular joints
- Facial muscles
- Nasal vestibule
- Thyroid gland (anterior neck)
- Lymph nodes (lateral and posterior neck, supraclavicular notch)
- Parotid gland
Assess the hair for thickness and loss; carefully examine the sun-exposed facial skin for ultraviolet damage and lesion development, as well as the neck, ears, forehead, nasal bridge and alae, malar region, eyebrows/eyelids/eyelashes, vermilion of the lips, and the chin. Next, perform careful palpation of each of these sites to rule out the presence of deeper, mesenchymal and other types of tissue swellings.
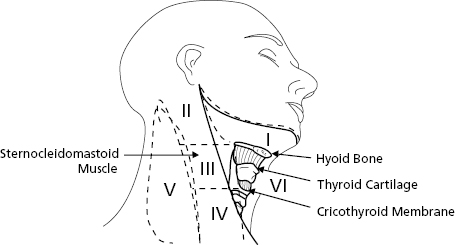
Palpate all lymph nodes and note any enlargement for additional testing since normal lymph nodes are soft and not palpable (Fig. 1.1). Specifically, the subcutaneous tissue is digitally kneaded with a rotating motion in the areas of lymph nodes based on the clinician’s knowledge of anatomy. This process can begin in the submental area, below and lingual to the chin, against the mylohyoid muscles. Next, palpate the submandibular nodes by pressing the tissue below the jaw against the medial side of the mandible or by bimanual palpation with one finger in the mouth and the other externally pushing up. Next, palpate the parotid gland and its associated lymph nodes—look and feel anterior and posterior to the ear. Next, palpate the cervical lymph node chain. The posterior cervical chain is along the back of the neck, and the anterior and deep cervical chain is along the front. An anatomical landmark for the latter nodes is the sternocleidomastoid muscle—trace from behind the ear to the clavicle, kneading deep and medial to it. The postauricular and retrosternomastoid region should also be palpated along with the back of the neck. Lastly, palpate the thyroid gland by placing fingers gently over it and have the patient swallow. Sometimes, in order to discover an enlargement, the grouped fingers are placed on one side of the larynx and pushed laterally while palpating the opposite side.
Intraoral Sites
Specific mucosal covered sites include the following:
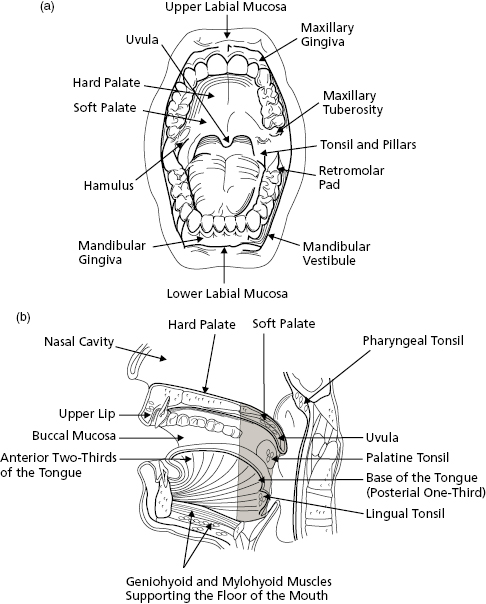
- Oral cavity (Fig. 1.2a,b)
- Tuberosity/hamular notch
- Attached gingiva
- Retromolar pad/trigone area
- Vestibule (also called the mucobuccal fold)
- Buccal mucosa
- Labial mucosa
- Tongue (dorsal, ventral, and lateral surfaces)
- Floor of mouth
- Hard palate
- Submandibular and sublingual glands
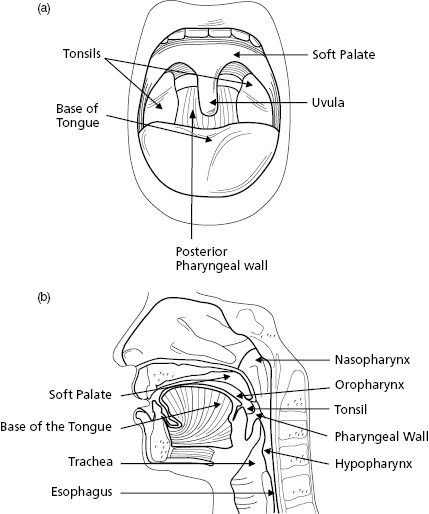
- Oropharynx (Fig. 1.3a,b)
- Soft palate
- Tonsillar pillars and fossa
- Tongue (base)
- Pharynx (lateral and posterior walls)
It is recommended that the same examination sequence be followed each time, first by visual examination and then palpation. As mentioned previously, any sequence can be used as long as it is organized and there is understanding of the findings and the significance of deviations from normal. Palpation should be bimanual or bidigital and, whenever possible, by direct vision. The following is a detailed suggested descriptive narrative:
- Lips—Have the patient slightly part his or her lips to examine the upper and lower vermilion borders and the left and right commissures. Then, with the patient’s teeth occluded, evert both the upper and lower lips to expose the labial mucosa. Observe the maxillary frenum, which at times may exhibit a mucosal tag, a variation of normal. As the upper and lower labial mucosa become dry, observe the minor salivary glands and attempt to express mucin from them. While the lips are everted, the anterior maxillary and mandibular vestibules can be observed.
- Labial and buccal mucosa/alveolar mucosa and attached gingiva/trigone—Slide your fingers posterior on the left and right buccal mucosa as well as the posterior portion of the vestibules. The parotid papilla overlying Stensen’s duct should be of normal coloration. To verify function, dry it, and then have the patient’s mouth wide open so that the cheek is stretched taut. Place four fingers flat on the face over the parotid gland in the preauricular area and milk the gland by using digital pressure to compress it against the masseter muscle or ramus area. Most patients exhibit a subtle white line at the occlusal plane of the buccal mucosa (i.e., linea alba), which is considered a variation of normal. While retracting the cheeks use mirror-assisted indirect vision to examine the tuberosity/hamular notch area and then, with direct vision, use the fingers and a mirror face to retract the buccal and labial mucosa, and observe the facial alveolar mucosa, mucogingival junction, attached gingiva, and free marginal gingiva on the maxilla and mandible as well as on the lingual mandible. Lastly, inspect and then palpate the retromolar pads and trigone area.
- Hard palate—Examine its anterior portion, the rugae (firm folds), and then the posterior, which at times exhibits a subtle pink-white change due to slight amounts of extra keratin on the surface. Laterally, in the posterior hard palate area, many minor salivary glands (mucinous) are present and thus the palate can have a subtle pink-blue appearance. Often, the most posterior extent of the hard palate’s midline has two small paired depressions, the fovea palatine.
- Tongue—Gently hold the anterior tip with gauze and pull forward and to the left and right. While the tongue is in this position examine the lateral and ventral surfaces of the tongue, including the most posterior lateral extent which is occupied by foliate papillae. The anterior two-thirds of the dorsum should demonstrate filiform papillae, and often there is a mild white coating caused by slough of the keratin from the filiform papillae. Note, among the filiform papillae, the larger and fewer dome-shaped fungiform papillae. At the junction with the posterior one-third, the dorsal surface exhibits an upside-down “V” linear series of circumvallate papillae. After freeing the tongue, instruct the patient to protrude the tongue, move it left and right, and touch the hard palate with its tip. In this way, the tongue’s full mobility is confirmed and the latter movement enables further inspection of the tongue’s ventral surface.
- Floor of mouth—Examine the anterior portion with its left and right sublingual plicae (V-shaped caruncula with its vertex toward the face), which contain the opening of the sublingual glands. At the most anterior extent of the plicae, there are raised areas that possess the opening of the submandibular glands (i.e., Wharton’s duct). The posterior portion of the floor is also examined. Palpate both the sublingual and submandibular glands by supporting the external chin with one hand and extending a finger downward in the floor of the mouth. To test salivary flow, dry the lingual carunculae, and then place one or two outstretched fingers under the chin and alongside the inferior mandible. Upward pressure directed to the submandibular gland area should produce saliva from Wharton’s duct orifice.
- Oropharynx—With the patient’s mouth wide open, and using a tongue depressor, ask the patient to say “ah”; at this point the vibrating line (i.e., where the palatal bone ends) at the beginning of the soft palate moves and, centrally and posteriorly, the pendulous uvula should be present. In this area, a circular distribu/>
- Labial and buccal mucosa/alveolar mucosa and attached gingiva/trigone—Slide your fingers posterior on the left and right buccal mucosa as well as the posterior portion of the vestibules. The parotid papilla overlying Stensen’s duct should be of normal coloration. To verify function, dry it, and then have the patient’s mouth wide open so that the cheek is stretched taut. Place four fingers flat on the face over the parotid gland in the preauricular area and milk the gland by using digital pressure to compress it against the masseter muscle or ramus area. Most patients exhibit a subtle white line at the occlusal plane of the buccal mucosa (i.e., linea alba), which is considered a variation of normal. While retracting the cheeks use mirror-assisted indirect vision to examine the tuberosity/hamular notch area and then, with direct vision, use the fingers and a mirror face to retract the buccal and labial mucosa, and observe the facial alveolar mucosa, mucogingival junction, attached gingiva, and free marginal gingiva on the maxilla and mandible as well as on the lingual mandible. Lastly, inspect and then palpate the retromolar pads and trigone area.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


