Introduction to Restorative Dental Materials
Objectives
After reading this chapter, the student should be able to:
< ?mpslid E1?>< ?mpslid S2?>
< ?mpslid E2?>< ?mpslid S3?>
< ?mpslid E3?>< ?mpslid S4?>
4. Define the differences between direct and indirect restorations, and give examples.
< ?mpslid E4?>< ?mpslid S5?>
< ?mpslid E5?>< ?mpslid S6?>
< ?mpslid E6?>< ?mpslid S7?>
7. Describe the role of restorative materials in the prevention of oral disease and trauma.
< ?mpslid E7?>
Key Terms
Abutment teeth
Bridge
Caries
Complete denture
Endosseous dental implants
Extracoronal restorations
Fixed partial denture
Intracoronal restorations
Maryland bridge
Pontics
Removable partial denture
Restorative dental materials are used to prevent or repair damage to teeth caused by oral disease or trauma. The restoration of teeth is critical to the well-being of any individual. Tooth damage, loss, or dysfunction contribute to malnutrition, speech disorders, and deterioration of the temporomandibular joint or alveolar bone, and may inflict significant pain. Furthermore, the teeth dominate an individual’s facial appearance, and missing or damaged teeth often compromise social well-being and self-esteem. Emerging data support links between oral health and systemic diseases such as heart disease, diabetes, arthritis, and abnormal pregnancy. Restorative dental materials are among the tools used by the dental team to prevent disease and alleviate pain, inflammation, and infection caused by disease, thereby improving the patient’s total health. The dental auxiliary plays an important role in the delivery of care to repair damage to teeth from oral disease and trauma.
Dental Disease and Restorative Materials
Caries
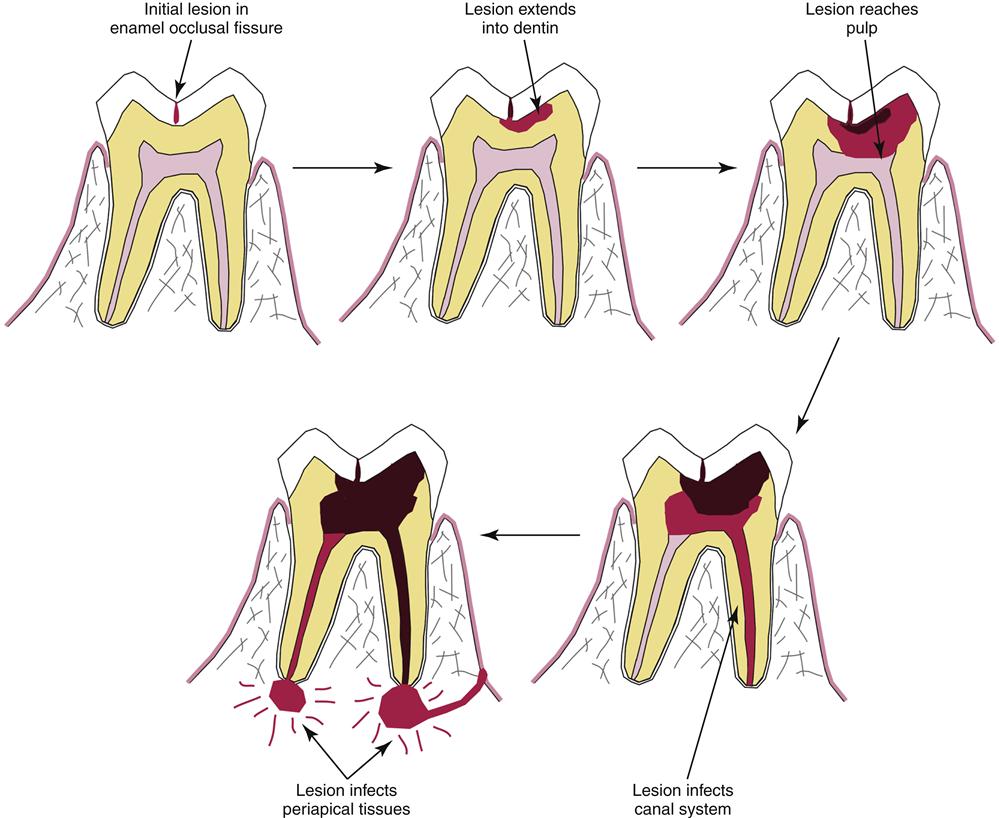
In spite of tremendous strides in its prevention, caries remains a major global problem in all countries and leads to significant destruction of teeth, pain, systemic infection, and tooth loss (Figure 1-1).
Caries is caused by bacterial plaque, which accumulates on teeth in areas where patients do not remove it (see Figure 1-1). A complex community of bacteria in plaque adheres to teeth and secretes acids and enzymes that dissolve the enamel, dentin, and cementum. Carious lesions occur on any tooth surface but are most common in areas where plaque accumulates unchecked—in the pits and fissures, along the gingiva, and interproximally. Caries also is a significant problem on the roots of the teeth of older individuals, where it rapidly destroys the softer cementum and dentin. As caries progresses over a period of months, more and more of the coronal tooth is destroyed, and the bacteria infect the pulp of the tooth and ultimately the periapical tissues as well. If left unchecked, an infection caused by caries can be fatal, but extraction of the tooth is a more common outcome. Dental restorative materials are used at every stage of the caries disease process to prevent or repair damage (discussed later).
Periodontal Disease
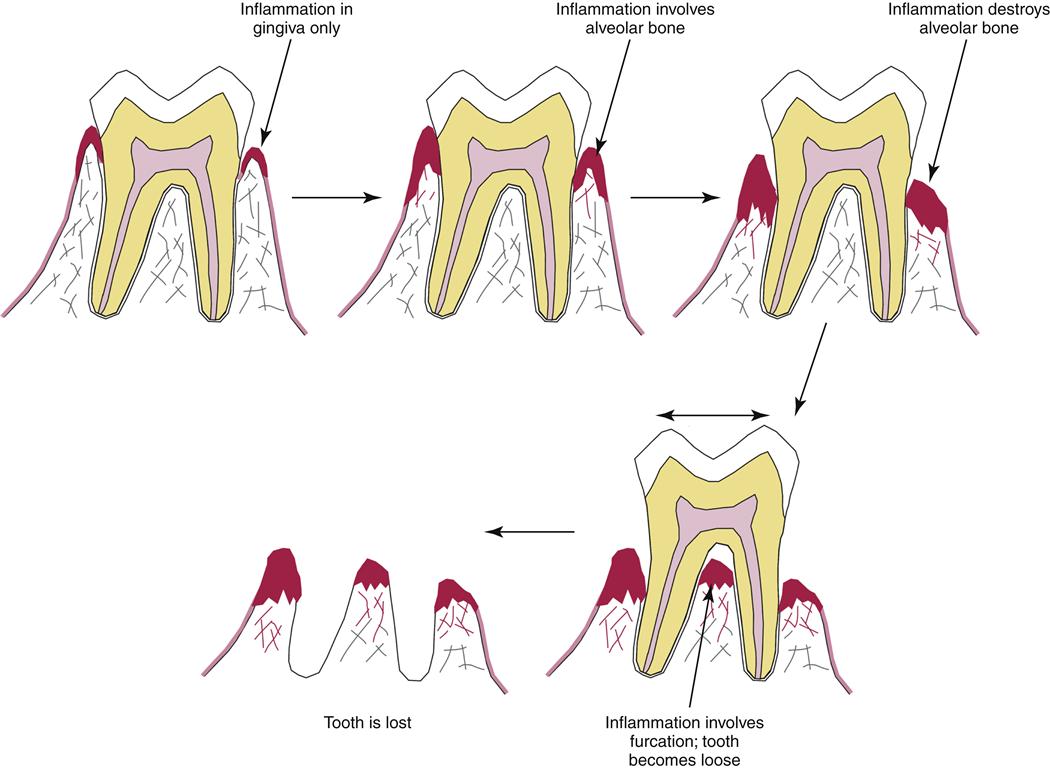
Unlike caries, periodontal disease affects the tissues supporting the teeth, including the gingiva, periodontal ligament, cementum, and alveolar bone (Figure 1-2). Periodontal disease also is caused by bacterial plaque, although the strains of bacteria are different from those that cause caries, and the progression of the disease occurs over many years rather than months. Initially, toxins secreted by bacteria in the plaque inflame the gingiva (gingivitis), but the hard tissues (cementum or bone) are not involved. Over time, the chronic inflammation induced by the bacteria causes irreversible destruction of the alveolar bone, periodontal ligament, and cementum (periodontitis). Destruction of these tissues results in deep pockets around the teeth that harbor plaque with even more damaging species of bacteria that grow in an anaerobic (low or no oxygen) environment. As the supporting tissues are lost, the tooth becomes mobile, and root surfaces and furcations become exposed. Exposed root dentin is often very sensitive (dentin hypersensitivity) to cold, toothbrushing, or sweets, leading to even poorer cleaning. Ultimately, the support for the tooth becomes so compromised that the tooth is lost. Periodontal disease increases the risk of caries or pulpal infection by giving cariogenic bacteria access to the tooth root or the periapical structures. Restorative dental materials are used to limit tooth mobility or replace function of lost teeth by distributing occlusal forces to healthier remaining teeth. Materials also are used to reduce sensitivity associated with exposed root surfaces.
Trauma, Systemic Disease, and Genetic Disorders
Trauma may cause diverse and significant damage to teeth and other oral structures, and restorative dental materials play a major role in repairing trauma-induced damage. Trauma may fracture only the enamel or dentin or may cause a fracture of the tooth that involves the pulp or alveolar bone. Teeth may be completely lost (avulsion) or displaced in any direction. Restorative materials are used to repair teeth, stabilize them until the supporting tissues heal, or replace them.
Systemic disease sometimes destroys teeth and oral tissues, and restorative materials are used to repair this damage. Cancer of the head and neck region may require that a large segment of the maxilla or mandible or associated oral structures be removed for the patient to survive. Dental prostheses restore function or esthetics for these unfortunate patients. Osteoporosis compromises the bony support for teeth, leading to edentulism and the need for major oral restoration. Diabetes accelerates and exacerbates periodontal disease. In older individuals, systemic disease often amplifies oral disease. For example, many older individuals experience decreased salivary production, which limits the body’s oral immune response and promotes both caries and periodontal disease. Fluorosis, resulting from natural or iatrogenic excess ingestion of fluoride when the teeth are forming, disfigures and discolors tooth enamel and requires esthetic treatments or restoration.
Genetic disorders are another significant cause of oral disease that requires the use of restorative dental materials. In several genetic diseases, teeth may be congenitally missing. Other diseases, such as amelogenesis imperfecta or dentinogenesis imperfecta, cause major loss of tooth structure from defective enamel, dentin, or the bonds between enamel and dentin. In these patients, nearly every tooth will require restoration.
Restoration of Damaged Teeth
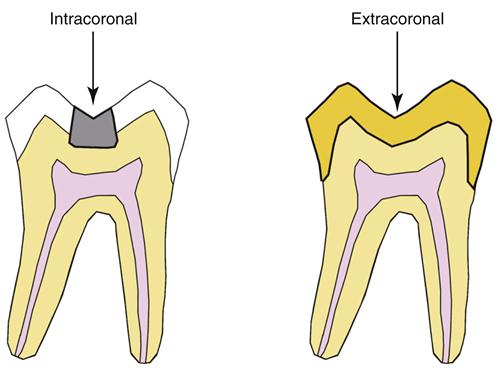
Regardless of the source of damage, teeth are repaired using two basic types of restorations: intracoronal and extracoronal (Figure 1-3). If the damage to the tooth involves the pulpal or periapical tissues, then endodontic restorative treatments are used in addition to these restorations.
Intracoronal Restorations
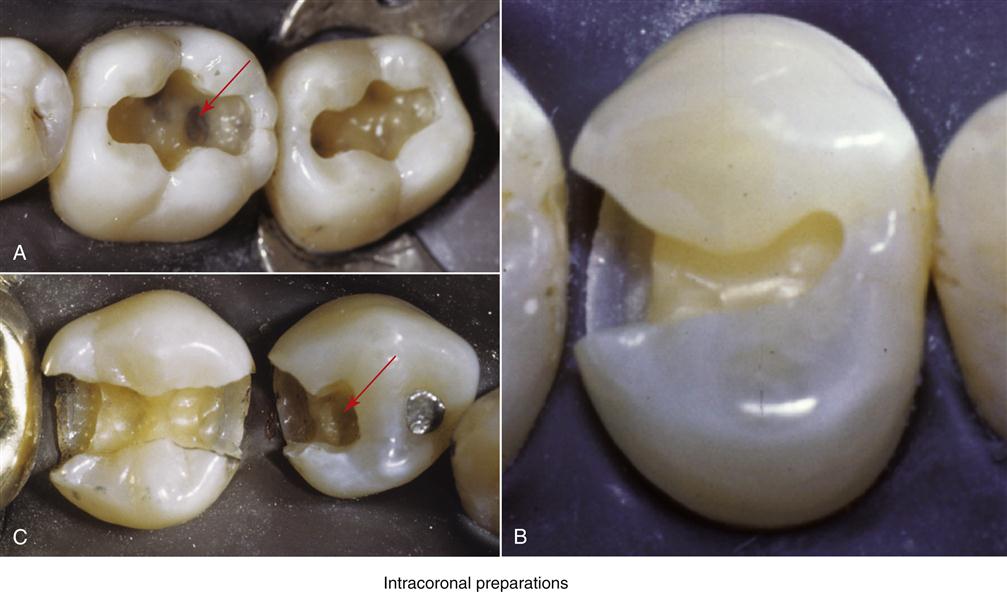
Intracoronal restorations are used to repair damage that is restricted to the internal parts of the tooth (see Figure 1-3). Damage of this nature is nearly always caused by caries but is occasionally caused by trauma. For intracoronal restorations, the tooth is first surgically prepared to receive the restoration, a process commonly referred to as cavity preparation (Figure 1-4). Cavity preparation removes diseased or damaged tissue and creates a space that is accessible for restoration and able to stably retain the restoration. Many complex factors govern the surgical cavity preparation, although a thorough discussion of the “principles of cavity preparation” is beyond the scope of this text. Cavity preparations may be restored (Figure 1-5) with materials such as amalgam (Chapter 5), resin composites (Chapter 4), cast alloys (Chapters 11 and 12), ceramics (Chapter 14), or less often by gold foil (Chapter 11).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses