Chapter 1 Introduction
The mouth is an easily accessible part of the body and so can provide health care workers with a window into a person’s oral and general health. Disease that is localized elsewhere in the body can be reflected in the mouth and, as a result, saliva is becoming increasingly recognized as a key diagnostic fluid. For example, oral candidosis (Ch. 9) in previously healthy young adults can be the first sign of HIV infection, while antibodies against a range of viruses can be detected in saliva. Risk factors for general health, such as tobacco habits, alcohol abuse and an inadequate diet, can also have a deleterious effect on oral health while, in an analogous manner, oral disease can also have an impact on the overall health of the individual. Recent studies suggest that severe periodontal disease in some populations might be a risk factor for premature or low birth weight babies, ischaemic heart disease, pulmonary disease and diabetes mellitus (see later, and Ch. 6).
The mouth is one of the key interfaces between the body and the external environment, and can act as a site of entry for some microbial pathogens, especially from the air or via ingestion from the diet. Therefore, it is equipped with a comprehensive array of defence strategies that includes elements of both the innate and adaptive immune system (see Ch. 2). Indeed, the ability of the host to recognise and respond to invading pathogens while simultaneously tolerating a diverse resident microflora (see Ch. 3) remains one of the most remarkable feats of evolution, and the precise mechanisms that permit this level of discrimination are still not fully understood.
The human microflora
It has been estimated that the human body is made up of over 1014 cells of which only around 10% are mammalian. The remainder are the microorganisms that comprise the resident microflora of the host. This resident microflora does not have merely a passive relationship with its host, but contributes directly and indirectly to the normal development of the physiology, nutrition and defence systems of the organism. In general, these natural microfloras live in harmony with humans and animals and, indeed, all parties benefit from the association. Loss or perturbation of this resident microflora can lead to colonization by exogenous (and often pathogenic) microorganisms, thereby predisposing sites to disease.
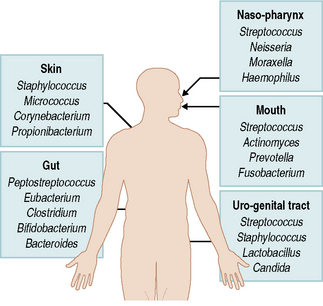
The microbial colonization of all environmentally accessible surfaces of the body (both external and internal) begins at birth. Such surfaces are exposed to a wide range of microorganisms derived from the environment and from other persons. Each surface, however, because of its physical and biological properties, is suitable for colonization by only a proportion of these microbes. This results in the acquisition, selection and natural development of a diverse but characteristic microflora at distinct sites (Fig. 1.1). For example, staphylococci and micrococci predominate on the skin surface but rarely become established in significant numbers in the mouth of a healthy person. Similarly, less than 30 out of over 700 types of microorganism found in the mouth were able to colonize the gastrointestinal tract, despite the continual passage of these microbes through the gut. Furthermore, the predominant species of bacteria can differ markedly at distinct surfaces in the mouth despite these organisms having equal opportunities to colonize each site, and this is due again to subtle variations in key parameters than influence microbial growth and competitiveness (see Ch. 4).
The oral microflora in health and disease
The mouth is similar to other sites in the body in having a natural microflora with a characteristic composition and existing, for the most part, in a harmonious relationship with the host. This microflora is described in Chapter 3 and its intra-oral distribution is presented in Chapter 4. Perhaps more commonly than elsewhere in the body, this relationship can break down in the mouth and disease can occur. This is usually associated with:
Bacteria with the potential to cause disease in this way are termed ‘opportunistic pathogens’, and many oral microorganisms have the capacity to behave in this manner. Indeed, most individuals suffer at some time in their life from localized episodes of disease in the mouth caused by imbalances in the composition of their resident oral microflora. The commonest clinical manifestations of such imbalances are dental caries and periodontal diseases (see Ch. 6), both of which are highly prevalent in industrialized societies and are now on the increase in developing countries; other acute and chronic infections occur but less frequently (see Ch. 7). Dental caries is the dissolution of enamel or root surfaces (demineralization) by acid produced primarily from the metabolism of fermentable carbohydrates in the diet by bacteria colonizing the tooth surface (dental plaque). Dental plaque is also associated with the aetiology of periodontal diseases in which the host mounts an inappropriate inflammatory response to an increased microbial load (due to plaque accumulation) around the gingivae, resulting in damage to the supporting tissues of the teeth.
Caries and periodontal diseases pose distinct challenges when it comes to determining their microbial aetiology. These diseases occur at sites with a pre-existing diverse, natural resident microflora, while even more complex but distinct consortia of microorganisms are implicated with pathology. It is necessary, therefore, to determine which microbial species are implicated directly in active disease, which are present as a result of disease and which are merely innocent bystanders. Numerous studies have shown that these common diseases are caused by shifts in the balance of the resident microflora, in which some minor components of dental plaque become predominant due to a change in local environmental conditions. These shifts in dental plaque composition in caries and periodontal disease are described in detail in Chapter 6.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses