div epub:type=”chapter” role=”doc-chapter”>
R. Reti, D. Findlay (eds.)Oral Board Review for Oral and Maxillofacial Surgeryhttps://doi.org/10.1007/978-3-030-48880-2_1
1. Dentoalveolar
Impacted teethPell and Gregory classificationWinter’s classificationRood’s criteriaInferior alveolar nerveLingual nerveInfratemporal spaceOroantral communicationSLOB ruleCone beamApically positioned flapLocalizationTrigeminal nerve injuryNeuropraxiaAxonotmesisNeurotmesisModified medical research council scaleCoronectomyThrombinMicrofibrillar collagenAminocaproic acidTranexamic acidEpineuriumEndoneuriumPerineuriumNeurorrhaphyNeuromaNeurolysisEntubulation
Dentoalveolar
Impacted tooth – a tooth that cannot or will not erupt into its normal functioning position.
Management of Impacted Third Molars
-
Frequency of impacted third molars ~25% in most studies when present [1].
-
Third molars are the most common teeth to be missing, followed by second premolars and maxillary lateral incisors.
-
Third molars are the most likely teeth to be impacted followed by maxillary canines, mandibular premolars, maxillary premolars, and second molars.
-
Third molar agenesis is reported between 10% and 41% [2].
-
African Americans develop third molars faster than Caucasians.
-
Age 6–9 – follicles become visible on radiography.
-
Age 9 – molar germ visible.
-
Age 11– cusp mineralization, located anterior border of ramus.
-
Age 14 – crown formation is done.
-
Age 15 – tooth uprighting as roots form.
-
Age 16 – 50% of root formed. Anterior border of ramus resorbs as mandible lengthens.
-
Age 18 – root completely formed with an open apex.
-
Age 24 – 95% of molars in final tooth position.
-
Age 25 – little change in tooth positioning, but minor changes may occur past this age.
-
1.
Differential growth rate of roots causes under- or overrotation leading to impaction.
-
2.
Arch length: Impacted third molars are larger than erupted third molars.
-
3.
Ectopic position: abnormal germ position puts teeth in contact with a denser external oblique ridge.
-
4.
Late mineralization: tooth growth lags behind maturation of jaws due to decreased influence of resorption of jaw.
-
5.
Attrition: softer diet leads to less attrition retaining mesiodistal space.

Pell and Gregory classification. (Reprinted with Permission from Mantovani et al. [13])
-
A: Third molar occlusal plane in line or nearly in line with adjacent second molar.
-
B: Third molar occlusal plane between occlusal plane and cervical junction of the second molar.
-
C: Third molar occlusal plane below cervical junction second molar.
-
1: Mesiodistal diameter of crown anterior to ascending ramus.
-
2: Half of crown covered by ramus.
-
3: Tooth is completely located within ramus.
-
Most commonly used classification system.
-
Angle between the occlusal plane and the longitudinal axis of the third molar.
-
<0° = inverted, rare. As is buccoangular and linguoangular.
-
0° and 30° horizontal impactions, ~10% of impactions.
-
31° and 60° mesioangular impactions, ~45% of impactions.
-
61° and 90° vertical impactions, ~40% of impactions.
-
>90° distoangular impactions, ~5%.
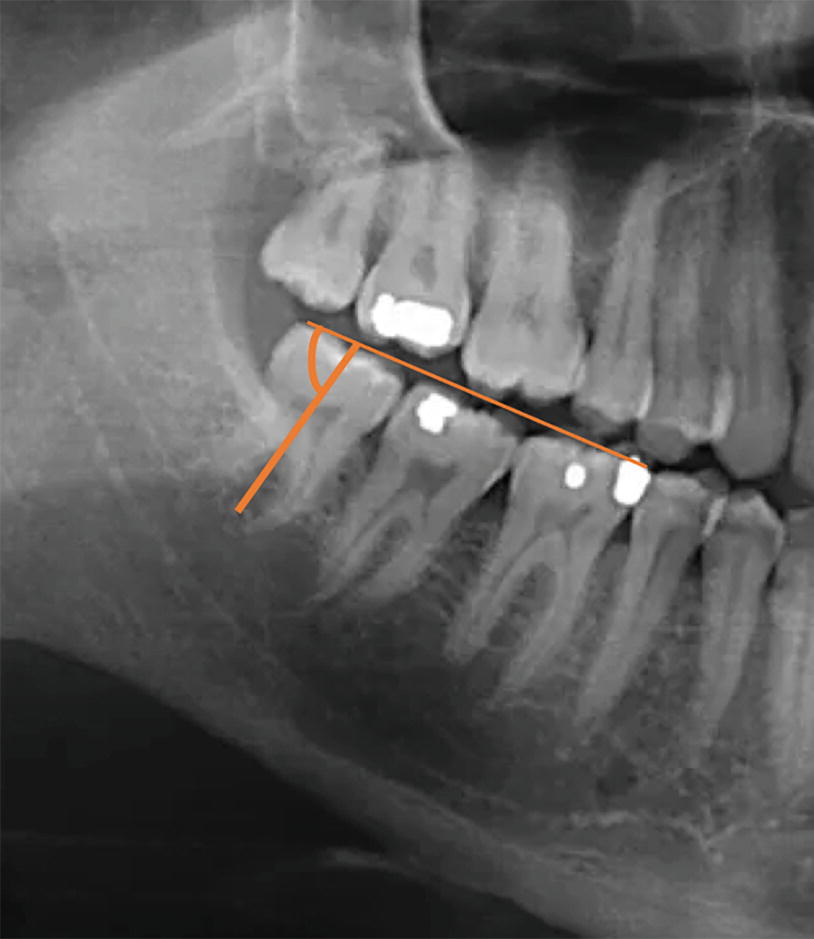
Winter’s classification is based on the angle between the occlusal plane and the longitudinal axis of the third molar
Indication for Third Molar Removal
-
Most common reason over the age of 20.
-
Associated with inflammation of the operculum (a dense fibrous flap of tissue).
-
May be treated symptomatically with irrigation and antibiotics.
-
Removal of third molars is the most predictable treatment.
-
Dental crowding? No consensus if third molars associated with mandibular incisor crowding.
-
Interference with orthodontic treatment may prevent distalization of other teeth.
-
Orthognathic : surgeon may require third molars out 6–12 months prior to surgery to aid in bone fill. This allows an increase in bony area for fixation and may prevent bad mandibular splits.
-
Most common pericoronal pathology is a dentigerous cyst or an enlarged follicle. A pericoronal radiolucency >3 mm is suggestive of a dentigerous cyst.
-
Inability to clean adequately, most commonly on cervical of second molar.
-
Inability to isolate third molar for restorative measures.
-
Access to distal caries on second molar.
-
Presence of third molars creates an area of lowered fracture resistance.
-
Approximately 3× increase in angle fractures with third molar present due to disruption in cortical bone.
-
Special consideration in patients in contact sports.
-
Presence may complicate repair of angle fracture reduction.
-
5% of third molars removed for this reason and often “cures” pain for reasons unclear.
-
Third molars are unpredictable in future position or eruption. There is evidence for pathology to develop if left in place under prosthesis.
-
Up to clinician to remove or to watch but generally recommended to be removed unless 2 mm bone is surrounding the crown.
-
Consider removal if >5 mm pocketing with bleeding on probing or >1 mm attachment loss on adjacent second molar (may lead to future progression of periodontitis).
-
Presence of third molars associated with elevated levels of periodontitis of adjacent teeth.
Pertinent Anatomy
-
Provides sensation to mandibular lower teeth up to midline, chin, and lower lip.
-
Injury incidence reported approximately 1% after third molar extraction.
-
Generally the nerve is located buccal and apical to impacted third molars.
-
Lies on average 2.8 mm below the crest and 2.5 mm medial to lingual cortex.
-
0.6–2.0% reported incidence of lingual nerve damage during third molar surgery.
-
In 4.6–21.0%, the lingual nerve is at or above the crest of the bone.
-
22% reported at lingual plate of bone.
-
Turns toward tongue at region of first and second molars.
Workup
CC/HPI: Reason for removal, is the patient experiencing pain, in progress or planning on orthodontic/orthognathic treatment? etc.
PMHx:
-
Increased healing time and increased risk of morbidity.
-
Bone becomes more sclerotic and less elastic, which makes the removal complicated. This leads to the need for more bone removal.
-
Patients who are 25 years and younger have decreased risk of complications and improved recovery after surgery.
Inadequate age:
-
Unable to predict impaction when there is minimal tooth formation.
-
Ideally remove tooth when there is ½–2/3 development of root formation.
-
Benefits must outweigh the risks.
-
A history of cardiopulmonary disease, immunocompromised states, or coagulopathies could prevent a safe extraction (may be best to watch until symptomatic).
-
Consider treating patients in a more controlled setting should an extraction be indicated.
-
Problems with induction or awakening.
-
History of nausea or vomiting.
-
History of clicking, pain, or locking of joint.
-
Difficulty of opening for long periods of time or limited opening.
-
Delayed healing.
-
Higher risk of dry socket.
-
Reactive airway for anesthesia.
General: Examine distress and anxiety (can help determine if sedative/anesthesia required for procedure). Also degree of difficulty will aid in decision.
-
Customary head and neck exam is part of workup. Examine anesthesia considerations such as large neck, retrognathia, and limited range of motion of neck.
-
TMJ documentation for clicks, cracks, or pops.
-
Maximal incisal opening, ease of access for surgical procedure, and anesthesia considerations.
-
Tongue size: large tongues can fall back and cause airway obstruction.
-
General oral health. Could be higher risk for postoperative infection and delayed healing.
-
Pathology or infection around third molar site? Pericoronitis.
-
Are the third molars visible? Guide to difficulty of extraction.
-
Mallampati score.
-
Tonsil grade.
-
Periodontal probing distal to second molars (>4 mm indication with bleeding on probing (BOP) could be sign of periodontal disease).
-
Teeth are in good functional position and without disease. Direction of general dentist to have them removed based on an algorithmic approach to treatment is inappropriate. Surgeon should conduct a separate evaluation that deems this is a necessary procedure.
-
For overall survey of third molars. Most studies on risk based on orthopantogram. Able to classify difficulty of extraction.
-
Root morphology:
-
Ideally removal when two-thirds roots are developed.
-
Fused roots easier than flared roots.
-
Direction and severity of curved roots increase difficulty and can change the path of tooth extraction.
-
Periodontal ligament space, wider makes for easier extraction.
-
-
Follicular sac – if present, the wider the sac, the less the bone required for removal and the easier to identify tooth crown.
-
Density of bone:
-
Higher density leads to increased difficulty.
-
Patients >35 years of age regularly have increased density appreciated.
-
Higher likelihood of fracture due to lack of expansion and increased force required for removal.
-
-
Radiographic signs on orthopantogram described by Rood and Shehab, aka Rood’s Criteria, describing intimacy of Inferior Alveolar Nerve (IAN) with roots of mandibular third molar [5].
-
1.
Darkening of root
-
2.
Deflection of root
-
3.
Narrowing of root
-
4.
Bifid root apex
-
5.
Diversion of canal
-
6.
Narrowing of canal
-
7.
Interruption in white line of canal
-
-
CBCT
-
Not routine, but can be selected if pathology is suspected or if there is intimacy with anatomical structures.
-
Most software can convert imagery into a reformatted orthopantogram.
-
* The approaches in this book are just a guide. On the board exam you are asked how YOU would perform the procedure. The key is to practice articulating what you do every day in a concise and efficient fashion. Provided is just a guide on how to articulate the procedure. Practice verbalizing your technique.
-
Local anesthetic with vasoconstrictor is administered (via, e.g., IAN, lingual and buccal nerve blocks, PSA, and greater palatine).
-
A 15 blade is used to make a sharp incision to outline a full thickness mucoperiosteal flap. This flap is outlined from the mesiobuccal of the second molar and carried sulcular around the second molar with a distobuccal releasing incision.
-
A periosteal elevator is used to carefully reflect a full thickness flap exposing the bony mandible/maxillae.
-
Using a fissure bur under copious irrigation the bone surrounding the crown is carefully removed exposing the tooth and a buccal trough is created. (Bone in the maxilla is thin and can usually be removed with a molt/periosteal elevator).
-
Once the crown is uncovered, the tooth is luxated (if appropriate)/tooth is sectioned parallel to the mesiobuccal groove two-thirds through the width of the tooth to prevent cortical perforation.
-
The tooth crown and fragments are carefully removed.
-
The granulation tissue and follicle are curetted free of the socket.
-
Bone rasp is used to smoothen the bony lip of the osteotomy.
-
Saline irrigation is used to cleanse the socket. (Distilled water is hypotonic and leads to cell death).
-
Visual inspection to ensure IAN/sinus not compromised.
-
Reapproximate tissue with resorbable suture (e.g., 3-0 chromic gut).
-
Alveolar Osteitis – Incidence reported between 1% and 30%, range due to subjective criteria [6]. Commonly seen at days 3–7 after extraction. Current theory is increased fibrinolytic activity leading to break down of clot. Symptoms include referred pain to ear, eye, and temple region, foul odor, extreme tenderness to palpation. Risk factors: tobacco smoke, increasing age, pericoronitis, birth control, female gender, inexperience of surgeon leading to traumatic extraction, inadequate irrigation, and increased medical comorbidities. Some evidence show that chlorhexidine can reduce incidence. Treatment is commonly with iodoform gauze or gel foam coated with eugenol (commercial pastes are also available) that acts by inhibiting neural transmission. Review panorex and/or CT scan prior to application as should not be used when IAN exposed due to neurotoxic effects of eugenol. If concerned for IAN exposure, consider the use of topical lidocaine in place of eugenol.
-
Root Fracture – Can be left in place if (1) noninfected, (2) small, i.e., <2 mm, (3) and risk of surgery would outweigh benefits.
-
Bleeding – Bleeding report as a result of third molar surgery ranges from 0.2% to 5.8% [7]. Must always rule out coagulopathies such as hemophilia or Von Willebrand disease. In general, postoperative bleeding from dental extractions reported to be at about 1% and about 7% when taking oral anticoagulation therapy such as a vitamin K antagonist. Patients on vitamin K antagonist need not stop it if INR <4. Hemostatic agents are listed in Table 1.1.
-
Displacement of Root into Sinus – Most commonly the palatal root of maxillary first molar; take PA to verify position. Several local measures should be made: (1) suctioning into sinus, (2) pack sinus with xeroform gauze and pull in one stroke (often root will attach to gauze), (3) perform antral lavage, (4) have patient block opposite nostril and blow nose to force into socket, (5) enlarge opening and explore. If attempts fail, fragments 3 mm or less that are non-infected may be left in place and patient be informed. Roots >3mm or those that presented with an infection/peri-apical pathology should be removed via a Caldwell-Luc approach is indicated.
-
Oral Antral Communications (OAC) – Most small OACs will heal by themselves. Openings of 3–6 mm can be managed by placing gel foam and closing with a figure-of-eight suture technique. OAC >6 mm may require tension-free primary closure, excision of the fistulous tract, and inversion into the sinus. Consider treating larger OACs with a buccal fat pad closure, buccal finger flap, or tongue flap. Sinus precautions for 2 weeks (decongestants, antibiotics that cover sinus flora, no heavy nose blowing, saline nasal spray).
-
Displacement of Root or Tooth into Submandibular/Sublingual Space – Lingual cortex thins out in the more posterior region. Displacement is often inferior to mylohyoid muscle. First attempts should be to “milk” root back through cortical hole via manipulation. An attempt at a lingual flap extended anteriorly to premolar with an incision to detach the mylohyoid muscle to gain access and visualization of crown. This can be difficult due to bleeding. Allow 6 weeks for fibrosis. Get a CT scan to localize the root. Patient may require a transcutaneous approach via a submandibular incision for retrieval.
-
Displacement into Infratemporal Space – Likely due to lack of retractor protection with excessive force and poor visualization. Position most commonly lateral and inferior to pterygoid plate. May attempt to manipulate the tooth back manually into incision by placing finger high into vestibule near the plates and applying manual pressure. If good access and lighting, may attempt to extend incision and retrieve with hemostat. If primary efforts fail, allow 4–6 weeks to allow for fibrosis. Obtain a CT scan and use a spinal needle to identify, dissect along needle length. Needle-guided fluoroscopy may also be used. It also has been reported to perform a hemicoronal incision to gain access to infratemporal space. If no functional deficit and asymptomatic, may elect to leave in place.
-
Displacement into IAN Canal – Retrieval attempts may lead to nerve damage, and single attempt with suction should be attempted. If root is not infected and no neurological abnormalities, consider leaving in place. If sensory complications, must retrieve. CT scan should be taken to ensure whether in canal space versus medial to mandible. IAN root retrieval may be attempted by unroofing the extraction site, lateral window intraoral, or via submandibular incision.
-
Aspiration of Foreign Object – Heimlich maneuver may be attempted while patient is in beach chair position. If under anesthesia, deepen the level of sedation and attempt visualization and removal with Magill forceps. Cord pressure may help move objects caudally past the cords. If no respiratory distress, likely ingested, obtain abdominal and chest radiography to rule out. Always presume aspiration and place patient on right side in Trendelenburg. Continue monitoring and watch out for signs of hypoxia and respiratory distress. Refer to emergency room for removal.
Hemostatic agents
|
Surgical packing for tooth extraction sites |
|
|---|---|
|
Product |
Properties |
|
Absorbable gelatin sponge, e.g., Gelfoam® |
Matrix for blood clot formation Gelatin made from purified porcine skin May cause excessive granuloma or fibrosis |
|
Microfibrillar collagen, e.g., Avitene® |
Mechanically broken down bovine collagen Aggregates platelets onto fibrils and acts as a matrix for blood clot formation |
|
Chitosan dressing, e.g., HemCon® and ChitoFlex® |
Polysaccharide from shellfish Positively charged to attract erythrocytes Acts as a scaffold for clotting New dental formulation dissolves in 48 hrs |
|
Thrombin |
Promotes clot formation through activated bovine prothrombin Activates factor IIA Acts as serine protease converting fibrinogen to fibrin |
|
Oxidized regenerated methylcellulose, e.g., Surgicel® |
Binds platelets Negative pH is bacteriostatic and precipitates fibrin More efficient at hemostasis than gelatin sponge Can be packed into socket to aid in pressure hemostasis Does cause some prolonged healing Be cautious when using in lower third molar sockets as Surgicel creates an acidic milieu which can be toxic to the inferior alveolar nerve |
|
Cross-linked collagen, e.g., Collaplug® or Collatape |
Promotes platelet aggregation |
|
Tanin, e.g., found in teabag |
Serves as a vasoconstrictor |
|
Aminocaproic acid mouth rinse |
Stabilizes clot by inhibiting plasmin |
|
Tranexamic acid 5% mouth rinse |
Antifibrinolytic, inhibits conversion of plasminogen into plasmin |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


