Chapter 1 Cariology and Caries Management
Section A Caries Risk Assessment
Material Options
Dental Caries Treatment Strategies
Restorative Strategies with Minimally Invasive Dentistry
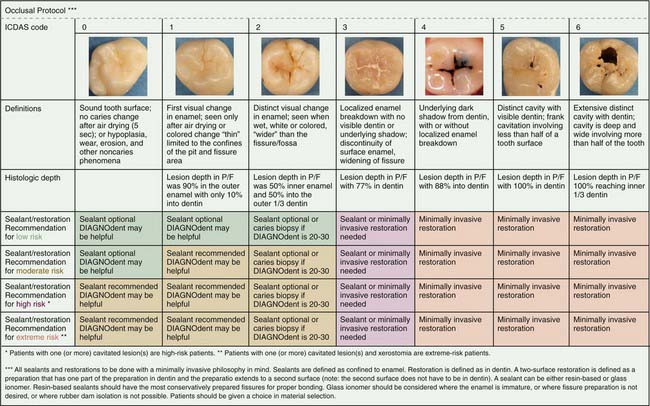
Traditionally dentists identified cavitated lesions using a sharp explorer tip, visual examination, and/or radiographs. The explorer in a given dental practice may not have been sharp, so defining lesions in specific states of cavitation varied from dentist to dentist. Numerous studies report that the use of a dental explorer is not adequate for detecting early occlusal lesions at all and not only may lead to a significant number of undetected lesions, including some false positives, but may, if it is sharp, cause traumatic surface defects in teeth. Radiographs are not useful for early occlusal lesions because of the masking effect of the facial and lingual enamel. New research has suggested the use of a visual ICDAS code system. ICDAS, an acronym for International Caries Detection and Assessment System, can be thought of as a coding system of 0 to 6 that correlates what is seen clinically with a definition and what research has reported histologically. The gradient starts with a code 0, which is a completely intact and healthy occlusal fissure system, and ends with a code 6, a fissure that is cavitated with a frank carious lesion. Recently Jenson and colleagues published various protocols based on ICDAS code and caries risk. Included is how one would use laser detection technology such as a DIAGNOdent (KaVo Dental, Charlotte, North Carolina) in the decision-making process (Figure 1-1).
Other Considerations
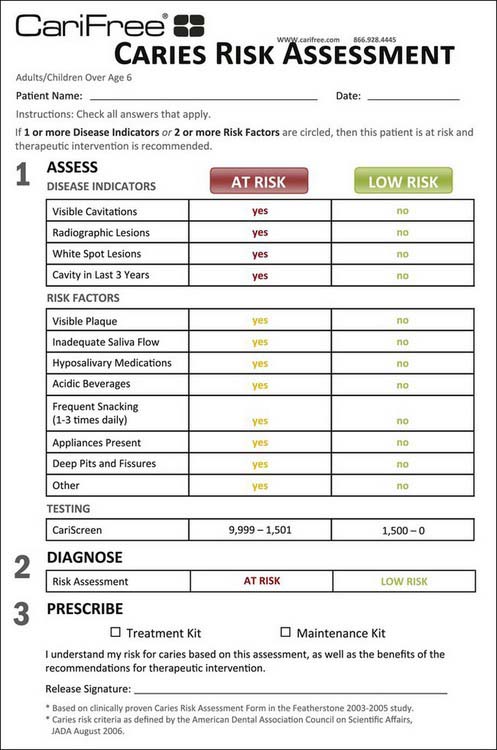
The most important consideration in performing a caries risk assessment and the medical management of dental caries is to use a standardized, validated caries risk assessment form. Several forms and sources are available (e.g., Journal of the California Dental Association, October-November 2007; www.cdafoundation.org; and other resources). In addition, in January 2009 the Scientific Council of the American Dental Association (ADA) endorsed caries risk assessment and provided a form available on the ADA website: www.ada.org/prof/resources/topics/topics_caries_over6.doc. Many forms include disease indicators, risk factors, and protective factors. Some forms stratify patients into high, moderate, or low risk categories; other forms also stratify them into extreme risk categories; and yet other forms include a determination of whether the caries is active or inactive. A simple caries risk assessment form that identifies the patient’s specific caries risk factors is all that is necessary. A simplified version based on a published form is presented in Figure 1-2.
Clinical Techniques
Becker MR, Paster BJ, Leys EJ, et al. Molecular analysis of bacterial species associated with childhood caries. J Clin Microbiol. 2002;40(3):1001-1009.
Beighton D. The complex oral microflora of high-risk individuals and groups and its role in the caries process. Community Dent Oral Epidemiol. 2005;33(4):248-255.
Brailsford SR, Shah B, Simons D, et al. The predominant aciduric microflora of root-caries lesions. J Dent Res. 2001;80(9):1828-1833.
Ekstrand K, Qvist V, Thylstrup A. Light microscope study of the effect of probing in occlusal surfaces. Caries Res. 1987;21(4):368-374.
Featherstone JD. The science and practice of caries prevention. J Am Dent Assoc. 2000;131(7):887-899.
Featherstone JD, Domejean-Orliaguet S, Jenson L, et al. Caries risk assessment in practice for age 6 through adult. J Calif Dent Assoc. 2007;35(10):703-707. 10-3
Fontana M, Gonzalez-Cabezas C. Secondary caries and restoration replacement: an unresolved problem. Compend Contin Educ Dent. 2000;21(1):15-18. 21-4 passim; quiz 30
Fontana M, Zero DT. Assessing patients’ caries risk. J Am Dent Assoc. 2006;137(9):1231-1239.
Heinrich-Weltzien R, Kuhnisch J, van der Veen M, et al. Quantitative light-induced fluorescence (QLF)—a potential method for the dental practitioner. Quintessence Int. 2003;34(3):181-188.
Jenson L, Budenz AW, Featherstone JD, et al. Clinical protocols for caries management by risk assessment. J Calif Dent Assoc. 2007;35(10):714-723.
Katz RV. Assessing root caries in populations: the evolution of the root caries index. J Public Health Dent. 1980;40(1):7-16.
Lussi A. Comparison of different methods for the diagnosis of fissure caries without cavitation. Caries Res. 1993;27(5):409-416.
Lussi A. Validity of diagnostic and treatment decisions of fissure caries. Caries Res. 1991;25(4):296-303.
McCullough MJ, Farah CS. The role of alcohol in oral carcinogenesis with particular reference to alcohol-containing mouthwashes. Aust Dent J. 2008;53:302-305.
Mouradian WE, Wehr E, Crall JJ. Disparities in children’s oral health and access to dental care. JAMA. 2000;284(20):2625-2631.
Penning C, van Amerongen JP, Seef RE, ten Cate JM. Validity of probing for fissure caries diagnosis. Caries Res. 1992;26(6):445-449.
Pitts N. “ICDAS”—an international system for caries detection and assessment being developed to facilitate caries epidemiology, research and appropriate clinical management. Community Dent Health. 2004;21(3):193-198.
Pitts NB, Rimmer PA. An in vitro comparison of radiographic and directly assessed clinical caries status of posterior approximal surfaces in primary and permanent teeth. Caries Res. 1992;26(2):146-152.
Preza D, Olsen I, Aas JA, et al. Bacterial profiles of root caries in elderly patients. J Clin Microbiol. 2008;46(6):2015-2021.
Reynolds EC. Remineralization of enamel subsurface lesions by casein phosphopeptide–stabilized calcium phosphate solutions. J Dent Res. 1997;75(9):1587-1595.
Ricketts D, Kidd E, Weerheijm K, de Soet H. Hidden caries: what is it? Does it exist? Does it matter? Int Dent J. 1997;47(5):259-265.
Takahashi N, Nyvad B. Caries ecology revisited: microbial dynamics and the caries process. Caries Res. 2008;42(6):409-418.
van Houte J, Lopman J, Kent R. The predominant cultivable flora of sound and carious human root surfaces. J Dent Res. 1994;73(11):1727-1734.
Verdonschot EH, Bronkhorst EM, Burgersdijk RC, et al. Performance of some diagnostic systems in examinations for small occlusal carious lesions. Caries Res. 1992;26(1):59-64.
Young DA. New caries detection technologies and modern caries management: merging the strategies. Gen Dent. 2002;50(4):320-331.
Young DA, Featherstone JD, Roth JR. Curing the silent epidemic: caries management in the 21st century and beyond. J Calif Dent Assoc. 2007;35(10):681-685.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses