1 Basics of the Health History, Physical Examination, and Clinical Investigations
1.0 INTRODUCTION
This chapter sets the foundation for this clinical guide by describing the basic principles and processes of clinical evaluation of the patient. Risk assessment first and foremost depends on obtaining a comprehensive medical history. In addition to physical examination, the clinician must determine whether any other clinical investigations are indicated prior to providing oral health care. These elements provide an essential basis for the clinical guide.
1.1 Obtaining a complete medical history
A wide variety of medical conditions and their treatments have the potential to affect oral health and may require specific considerations prior to providing dental care. In order to adequately assess a patient’s health and determine risk for developing complications, a complete medical history must be obtained and updated on a regular basis. Whether paper or electronic medical records are utilized, this information should be clear and easy to locate. Contact information for the patient’s primary care physician and any relevant medical specialists should also be recorded and accessible. Details of all telephone, email, or mail correspondences with the patient or his/her medical providers, as well as laboratory reports, should be included in the patient’s chart.
While a self-completed health history form can be useful in screening for certain medical conditions and risks, this should be used to guide, rather than replace, the medical interview. The oral health care provider and patient should be facing each other in a comfortable and relaxed manner during the interview, and translators should be used when necessary. When there are any questions or items in the medical history requiring greater detail or clarification, the patient’s primary care physician should be consulted.
1.1.1 Chief complaint
The chief complaint is the patient’s primary reason for seeking medical/dental consultation and should be recorded in his/her own words. Sometimes, a patient’s chief complaint when he/she presents to his/her oral health care provider will be some type of oral pain or a complication of a recent dental procedure. In some cases, the chief complaint may be directly related to an underlying medical condition. Examples include a patient with salivary gland hypofunction and rampant dental caries, or a patient with acute leukemia and acute onset of gingival bleeding.
1.1.2 History of present illness
The history of present illness relates directly to the chief complaint and is told from the perspective of the patient. This is essentially the story describing the chief complaint and should be collected in sufficient detail. Basic elements should include, as relevant to the nature of the chief complaint: history of onset; the duration, nature, quality, and timing of symptoms; complications; pain score; modifying factors; any treatment provided; and whether symptoms are stable, improving, or deteriorating.
1.1.3 Past medical history
The past medical history includes all relevant aspects of a patient’s health history both past and present. Medical conditions for which a patient has received treatment, or is actively being treated, and overall continuity of medical care should be included. Pertinent details of treatment and overall management should be obtained, such as timing of chemotherapy cycles in a patient undergoing cancer therapy, hemodialysis schedule in a patient with renal failure, or glycated hemoglobin (HbA1c) levels in a diabetic patient.
1.1.4 Medications and allergies
All current medications, prescription and non-prescription (over-the-counter, herbal supplements), taken on a regular basis must be listed. The dose, schedule, and most recent dose taken should also be noted, in particular if the medication is immunosuppressive/immunomodulatory, antihypertensive, antiglycemic, antithrombotic, or anticoagulatory. Previous exposure to specific medications, such as antiresorptive agents (e.g., bisphosphonates), is also important and should be selectively collected. If there appear to be any inconsistencies between the patient’s medical history and the list of medications, clarification should be requested. All reported drug allergies must be clearly noted, including the specific allergic reaction. Expected adverse side effects, such as gastrointestinal upset with opioid analgesics, should not be misclassified as an “allergy,” even if reported as such by the patient (adverse drug reactions).
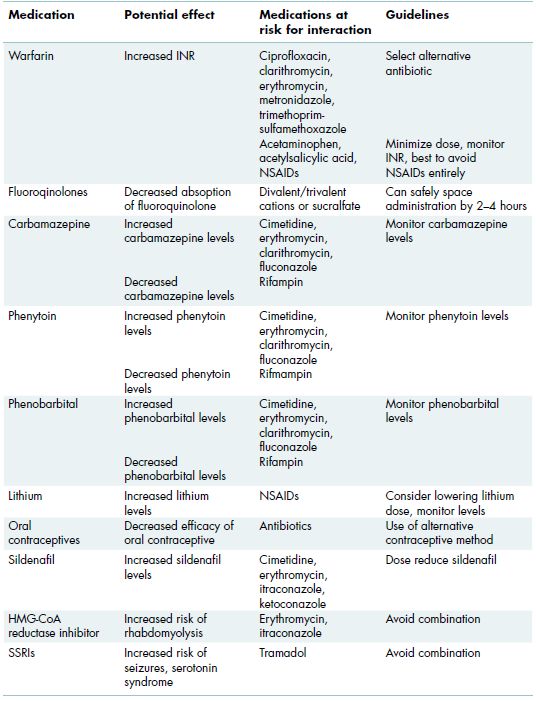
Certain medications have the potential to interact with one another through competitive binding, or through induction or inhibition of the hepatic cytochrome p450 pathway. Some common examples, such as antibiotics, antifungals, and analgesics, are shown in Table 1.1.
1.1.5 Review of systems
The review of systems is an extension of the past medical history that serves more or less as a “checklist” of a patient’s overall health by assessing specific symptoms within each system in a comprehensive manner. Systems include neurologic/psychiatric; ears, eyes, nose, and throat (EENT); cardiovascular/respiratory; musculoskeletal; hematologic; endocrine; gastrointestinal; and genitourinary (Table 1.2). Any positive responses should be followed with additional questioning and the patient should be referred to his/her primary care physician for further evaluation when indicated.
Table 1.1 Cytochrome P450-associated drug interactions.
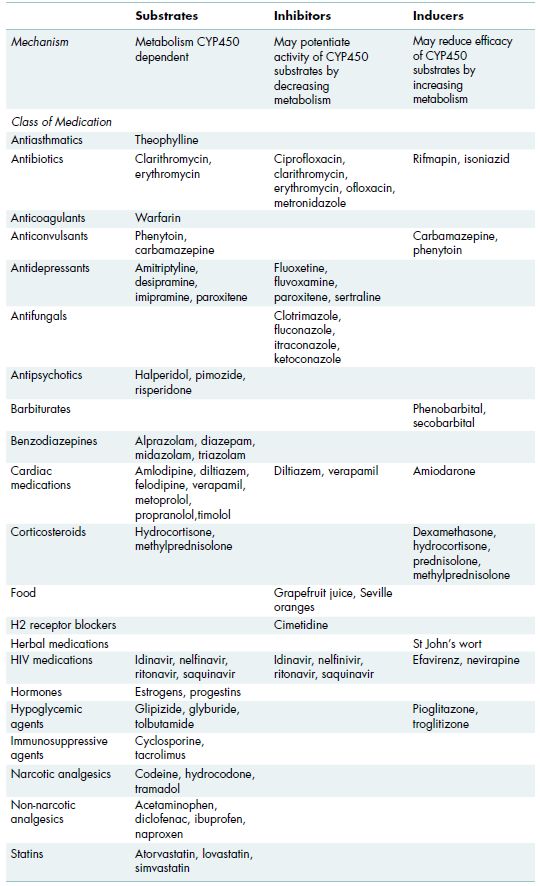
Table 1.2 Potentially serious drug interactions that may interact with medications prescribed by oral health care providers.
1.1.6 Family and social history
The family history should include any significant known medical conditions in first-degree relatives or that have been present in multiple generations. The social history should include whether the patient is single, previously married and/or divorced, or in a long-term relationship, and if s/he has children, as well as any other pertinent details that might impact his/her overall health. In addition, the patient’s occupation is important. For those who are not working, it is important to understand why, as this may be related to an underlying medical condition. Tobacco history should be obtained in pack-years (packs per day times the number of years), and if the patient has discontinued use, for how long; regular use of marijuana should also be ascertained. Alcohol and recreational drug use history should include amount and frequency and whether there is any history of treatment for abuse, addiction, or dependency. These aspects of the social history are important as stress, lifestyle, and psychosocial factors may contribute to disease presentation and may impact management.
1.1.7 Past dental history
A patient’s past dental history provides a great deal of information with respect to future risk of developing dental disease and associated complications. This should include whether care has been routine and preventive, or sporadic and problem-driven, and if so, why. Oral hygiene practices, home care, and diet should be reviewed.
1.2 Physical examination
Vital signs, including at minimum blood pressure and pulse, should be collected on all new patients and on an annual basis for general health screening, with appropriate referral when findings are abnormal (see chapter 2). For oral health care providers, the physical examination is largely limited to the head and neck and the oral cavity, intraorally extending from the labial mucosa anteriorly, to the soft palate, tonsils, and visible oropharynx posteriorly. Limited dermatologic examination, for example, can often be informative, especially when there is a chief complaint of oral lesions and concurrent skin lesions. Similarly, a limited neurologic examination may be warranted in a patient with signs and symptoms suggestive of a central nervous system disorder (Figure 1.1; see Figure 9.2). For proper conduct of a comprehensive examination, nothing more is needed than a good light source, a mouth mirror and gauze, which can be useful for manipulating the tongue and assessing salivary gland function. Normal findings should be summarized and for all positive findings, the size must be recorded as well as a description of color, consistency and contours of tissues.
1.2.1 Extraoral examination
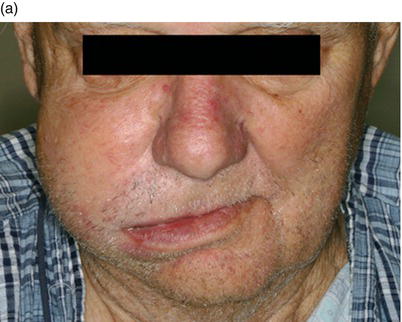
Extraoral examination begins with careful visual inspection for skin changes and any head/neck asymmetry or swelling (Figure 1.2). The head and neck is then palpated for swelling, tenderness, lymphadenopathy, thyromegaly, and any other abnormalities. Temporomandibular joint examination includes observation of opening, closing, and lateral excursions of the jaw, palpation of the muscles of mastication, and evaluation of the joints for sounds and tenderness (see chapter 12). Depending on the chief complaint and history of present illness, a limited or more extensive cranial nerve examination may be included to evaluate for neuromuscular and neurosensory deficits.
1.2.2 Intraoral examination
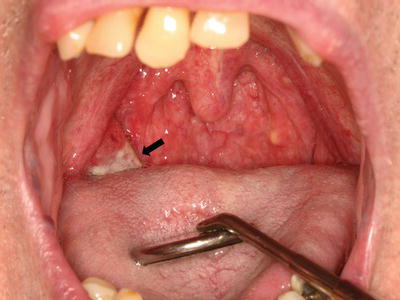
The intraoral soft tissues should be examined thoroughly, including the upper and lower labial mucosa, right and left buccal mucosa, vestibules, gingiva, ventrolateral and dorsal surfaces of the tongue, floor of mouth, hard and soft palate, and the tonsils and oropharynx. Normally keratinized sites include the gingiva, hard palate, and tongue dorsum; these sites have a thicker, paler appearance than the rest of the non-keratinized mucosa that tends to be more pink or red in color. The mucosa should be assessed for red and/or white changes, pigmentation, ulceration, or any other abnormalities (Figure 1.3). These tissues should then be palpated for any subtle inconsistencies or masses. The major salivary glands should be bimanually palpated, and then saliva should be expressed from the glands to assess duct patency and flow, and saliva should be evaluated for amount, consistency, color, and floor of mouth pooling (Figure 1.4). Saliva is expressed and observed by drying the duct orifice and then palpating the gland distally to proximally until saliva flows from the orifice. The dentition and periodontium should be examined, and any removable prostheses inspected for fit and function. The oropharyngeal anatomy, and in particular the tonsils, should be assessed for symmetry, size, color, and the presence of exudates or other abnormalities that might prompt referral to an otolaryngologist for further evaluation (Figure 1.5).
Figure 1.1 62-year-old male with metastatic prostate cancer involving the clivus (affecting cranial nerves IX and XII on the right side) with progressive right-sided tongue and constrictor muscle weakness. Straight protrusion of the tongue (a) demonstrates right-sided muscle flaccidity, whereas excursion to the right side (b) demonstrates minimal movement.

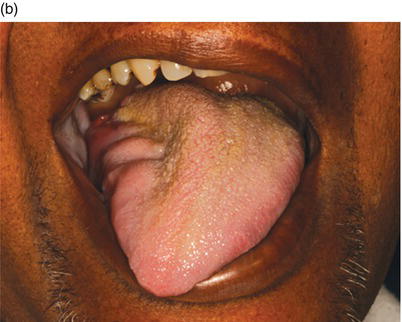
Figure 1.2 68-year-old male with notable extraoral asymmetry and swelling (a), that upon intraoral examination (b), demonstrated a large poorly differentiated carcinoma of the right maxilla.

1.3 Ordering and performing laboratory tests
Laboratory investigations may be necessary to determine a diagnosis or to evaluate for risk prior to dental treatment. How to order laboratory tests and, importantly, what test to order, when, why, and how to interpret the results are critical to the understanding of laboratory medical procedures. Retesting to confirm abnormal findings should always be considered, in particular when the findings are unexpected.
Figure 1.3 Well-defined area of leukoplakia of the anterior mandibular alveolar mucosa, with a distinct white appearance, against a background of normal-appearing pink mucosa.

Figure 1.4 Clear aqueous saliva expressed by palpating the parotid gland extraorally.

Figure 1.5 Squamous cell carcinoma of the right palatine tonsil (arrow), appearing enlarged and erythematous with extensive ulceration.
1.3.1 Basics of ordering laboratory tests
1.3.1.1 Identifying a clinical laboratory
Before a laboratory test can be ordered, a clinical laboratory must be identified. Options include a local hospital or commercial laboratory, such as Quest Diagnostics (www.questdiagnostics.com). The laboratory should be contacted regarding procedures for ordering tests, necessary supplies (e.g., culture kits), and where/how to order the recommended kits.
Alternatively, most testing can be coordinated through a patient’s primary care physician. In many cases, especially for the typical oral health care provider practicing outside of a larger health care facility, collaboration with the patient’s primary care physician may be the easiest option. Specific orders should be sent in writing to the physician’s office and a copy of the results should be requested.
1.3.1.2 Completion of forms
When ordering laboratory tests, the correct requisition forms must be used and fully completed. It can be very frustrating for the provider and patient when an incorrect test is run by accident. Typically an ICD-9 code (see section 1.3.1.3) is required for each test being ordered. By law, all submitted specimens must be accompanied by two patient identifiers (e.g., name and date of birth, on both the labeled specimen and the requisition form), and when appropriate (i.e., with a biopsy or culture) the site should be specified. Questions regarding the completion of requisition forms should be directed to the clinical laboratory.
1.3.1.3 ICD-9 codes
The International Classification of Diseases (ICD) is a coding system created and maintained by the World Health Organization that i/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


