Fig. 4.1
The radiographic presentations are shown of a deep caries lesion versus an extremely deep lesion. (a) The deep lesion involves the pulpal quarter with a radiodense zone separating the translucent zone from the pulp. (b) The extremely deep lesion defines a penetration that involves the entire primary/secondary dentin, either with no radiodense zone separating the demineralized dentin from the pulp or with a radiodense zone located within the pulp chamber indicative of tertiary dentin
A pulp exposure is defined relatively broadly being the result of a pathological change in the hard tissue of a tooth caused by caries, a mechanical factor, or trauma [10]. Here, a classification of pulp capping procedures is introduced separating two scenarios: direct pulp capping Class I (pulp exposure has been made accidently) and direct pulp capping Class II (pulp exposure is expected, as part of caries excavation and while using a microscope). This chapter aims to align updated treatment guidelines on best clinical evidence for vital pulp therapy in molars including the indirect pulp therapy approach.
4.2 The Benefit of Having a Vital Pulp
4.2.1 Apexogenesis
In injured teeth with incomplete root formation, it is essential to keep a vital pulp for the final formation and completion of the root complex, described as apexogenesis. Much focus has been given in the past to this topic [11], because the tooth has a better prognosis, if the roots are fully matured. Some of the problems associated with incomplete root formation of teeth after pulpal necrosis are briefly listed in Box 4.1 but also discussed in Chap. 7 of this book.
Box 4.1. Vital Pulp Therapy Aims at Apexogenesis for the Prevention of the Following
-
An open apex (a challenge to create a stop and establish a good seal)
-
Thin dentinal walls (more prone to fracture)
-
The incomplete apical development (in general making instrumentation and sealing more difficult)
-
Root fracture
4.2.2 Tertiary Dentinogenesis
The stimulation of tertiary dentinogenesis is a main objective of the vital pulp therapy. The classification and definition of tertiary dentin has in the past been described by many synonyms [12, 13]; here, it is presented in the context of dentinogenesis in general (Box 4.2). Tertiary dentin defines new hard tissue produced in relation to an external injury [14]. The subdivision of tertiary dentin into reactionary dentinogenesis and reparative dentinogenesis introduces a biological platform with more emphasis at the cellular origin [15, 16], as well as causes for the upregulation of the aged odontoblast secretion [17–19]. The reactionary dentin can be interpreted as the elevated growth of dentinogenesis, related to early caries lesions [20], and the odontoblast cells are stimulated by dentin matrix proteins released during caries demineralization [21, 22]. These upregulated primary odontoblast cells [18] are involved directly, but also a mixture with new beginners of secondary odontoblast-like cells can be observed in natural caries development [23]. In case of a pulp exposure, a complete new dentin formation leads to the reestablishment of a dentinal bridge formation, defined as reparative dentinogenesis (Box 4.2). Initially, it is composed by a layer of atubular mineralized matrix, described as fibrodentin [14], followed by a tubular dentin formation, presumably laid down by new secondary odontoblast-like cells.
Box 4.2. Classification of Dentinogenesis
-
Primary dentinogenesis: dentin produced before the tooth erupts
-
Secondary dentinogenesis: dentin physiologically produced after the tooth has erupted, eventually reducing the size of the pulp cavity
-
Tertiary dentinogenesis, dentin produced as a response to external stimuli and can be further divided into:
-
Reactionary dentin (new tubular dentin):
- (a)
Produced by upregulated odontoblasts or a mixture of these odontoblast cells and new secondary odontoblast-like cells
- (a)
-
Reparative dentin (two layers of hard tissue = dentinal bridge):
- (a)
Initially a layer of atubular dentin = fibrodentin (nonodontoblast origin)
- (b)
Followed by a layer of tubular dentin produced by new secondary odontoblast-like cells
- (a)
-
A significant portion of the dental literature has been dealing with the study of a newly formed hard tissue barrier and the status of the pulp after vital pulp therapy. A simple parameter for examining new pulp-protective agents has been to confirm whether or not tertiary dentin is present following pulp therapy. A recent systematic review has argued [24] that these microscopic analyses of histological sections on newly formed hard tissue may be considered a surrogate endpoint, which is difficult to interpret in the clinic. Future hard tissue studies following vital pulp therapy should analyze in more detail how well newly formed tertiary dentin reacts as a barrier, in order to avoid late invasion of microorganisms, and what is the structural integrity of newly formed hard tissue.
The formation of reparative dentin might be beneficial in terms of blocking potential bacteria from invading the pulp due to the atubular interface, as opposed to the structure of the primary tubular dentin. However, it should be remembered that the reparative dentin might contain more organic material and be less mineralized than primary dentin. The more organic material the dentin comprises, the more permeable it will be, and therefore the reparative dentin represents an inferior type of dentin as compared to primary dentin [12]. Also it is important to note that reparative dentin with or without so-called tunnel defects, cannot keep away the bacterial invasion from untreated progressing caries and/or a leaking coronal restoration. The optimal endpoint for evaluating vital pulp therapy would be to determine the long-term clinical outcome of the pulp, i.e., function, healthy state, and capacity of preventing a secondary infection [24].
4.2.3 Inflammation and Tertiary Dentin
Most experimental studies on pulp capping and protective agents have been carried out in healthy teeth, which in reality makes it difficult to transform information into the clinical situation, where the exposed pulp most often is expected to be associated with various grades of inflammation. Severity of pulp inflammation may influence tertiary dentin. At the extreme, inflammation will lead to pulp necrosis, hence stop or even absence of any tertiary dentinogenesis. In contrast, milder degrees of pulp inflammation may seem beneficial for tertiary dentinogenesis [25]. Taken together, some treatment principles can be aligned for the vital pulp therapy promoting apexogenesis and tertiary dentinogenesis (Box 4.3).
Box 4.3. General Principles for Vital Pulp Therapy
-
Removal of (i) bacterial infected dentin and (ii) clinically judged inflamed pulp tissue
-
The application of a pulp protective agent stimulating reparative dentinogenesis
-
To secure apexogenesis by the vital radicular pulp tissue
-
Performance of a coronal seal for preventing secondary infection of the reparative dentin and hence the development of infected pulp necrosis associated with apical periodontitis
4.3 Clinical Evaluation of Inflammation
Before the principles of vital pulp therapy are laid out, it is important to recall that a precise clinical diagnosis of the degree of inflammation in the pulp is not possible [3]. Little or no correlation exits between the histological findings of pulp pathosis and clinical symptoms [26–28]. Moreover, in a clinical setting a diagnostic device is not yet available for objectively measuring a threshold of reversible pulp inflammation being beneficial or not for tertiary dentinogenesis. The diagnoses are based on interpretation of data from the pretreatment examination, the clinical examination, as well as the radiographic examination [29], rather than histopathological findings. Clinical data are shown for case selection that divide the condition of the pulp into so-called reversible pulpitis and irreversible pulpitis (Box 4.4).
Box 4.4. Reversible and Irreversible Pulpitis
-
Reversible pulpitis:
-
A clinical diagnosis – based of the evaluation of subjective, clinical, and radiographic findings.
-
Suggest that if the external stimuli are removed the pulp will return asymptomatic and vital after long term evaluation.
-
Thermal changes (air, liquid) may produce a sharp transient pain.
-
In case of pulp exposure hemostasis can be obtained.
-
The diagnosis does not indicate the precise histological status of the pulp.
-
-
Irreversible pulpitis:
-
It is a clinical diagnosis associated with subjective and objective findings indicating presence of pain (spontaneous and or prolonged unbearable pain/disturbed night sleep).
-
Temperature changes may produce lingering pain.
-
In case of pulp exposure hemostasis cannot be obtained.
-
The diagnosis does not indicate the precise histological status of the pulp.
-
Figure 4.2 shows a clinical example of an extremely deep caries lesion with direct exposure of the pulp prior to excavation. The patient arrived to the dental office with prolonged pain and disturbed night sleep. The clinical diagnosis “irreversible pulpitis” is further confirmed by the color of the blood being dark red. In this case also pus is apparent associated with a frank cavitation, and hemostasis is not possible to achieve, and root canal treatment is initiated.
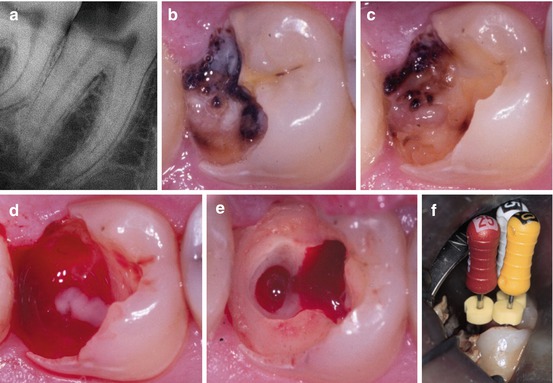
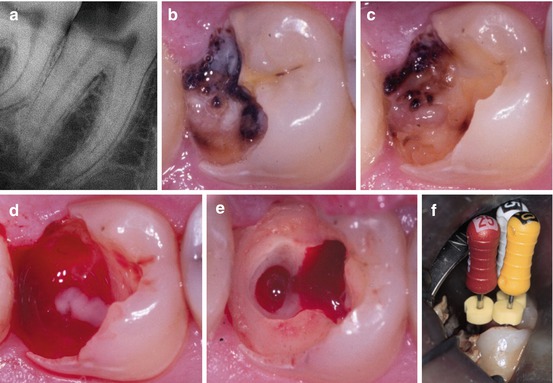
Fig. 4.2
(a) Preoperative periapical radiograph showing extremely deep caries lesion in the mandibular second molar with apical periodontitis. (b) Tooth shown before treatment. Clinically the tooth is vital and the combined diagnosis is “irreversible pulpitis” and apical periodontitis. (c) Following excavation an exposure of the pulp is present with pus. (d) During further access to the pulp cavity focal areas of pus are noted within the bleeding inflamed pulp. (e) Complete excavation performed before placement of “endodontic working” restoration and preparation of an aseptic working field. (f) Root canal treatment is initiated and determination of working length is about to be accomplished
4.4 Indications and Treatment Concepts for Vital Pulp Therapy
The principal indications for performing vital pulp therapy are carious lesions, mechanical iatrogenic injury, and trauma. In the context of molar endodontics, the most frequent cause for endodontic treatment including vital pulp therapy has, in the general practice environment, been caries [30]. Therefore, the aligned treatment guidelines are described within the “scenario” of a carious pulp exposure. From the literature, it is often unclear whether the clinicians are creating a pulp exposure by accident or whether it is the intention to do a pulp exposure; moreover the depth of the carious pulp exposures are seldom defined in clinical studies [31]. The following vital pulp therapy guidelines will include these aspects.
4.4.1 Direct Pulp Capping Class I (Accidental Pulp Exposure)
No additional enlargement is made of the exposed pulp. Typically, the exposure has just occurred following a trauma or an accidental perforation during a preparation procedure (Fig. 4.3). It is a prerequisite that the pulp is healthy. Clinically, this means that the pulp is vital and the patient is without subjective pain prior to treatment, and hemostasis can be expected. The exposure of the pulp is less than 1 mm in diameter and should be located in the coronal third, but preferable in relation to a pulp horn. The pulp protective agent can be placed directly at the pulp exposure and the cavity can be sealed efficiently. It may also take place during excavation of caries, but in an area not directly related to the carious dentin, because the pulp exposure has been made by accident.
Fig. 4.3
(Left) Direct pulp capping Class I: an accidental pulp exposure has occurred during preparation. No additional enlargement is carried out. (Middle) The cavity is irrigated with saline. (Right) Calcium hydroxide capping material is placed prior to permanent restoration
4.4.2 Direct Pulp Capping Class II (Intentional Pulp Exposure)
This modality includes the mandatory use of an operating microscope during caries excavation [32]. The potential implementation of carious dentin into the pulp during excavation can better be limited by the use of magnification. If hemostasis can be achieved it should be seen as the clinical interpretation of an acceptable and treatable pulp, but the exact extent of pulp inflammation is currently impossible to predict objectively in the clinical setting. No global consensus is available for this approach, and it may be argued that a pulp exposure shall be avoided by an indirect pulp therapy where less invasive excavation procedures are introduced (see below).
It has been shown in cases with deep or extremely deep caries that if the bacterial invasion zone penetrates the pulp close to reparative dentin, the subjacent pulp is severely inflamed [33], making both vital and indirect pulp therapy unpredictable treatment options. When irreversible inflammation in the pulp is present, hemostasis is typically not possible to obtain; therefore pulp capping is contraindicated in deep or extremely deep caries. However, when hemostasis can be controlled, such lesion depths may be successfully treated (Fig. 4.4). The result of apexogenesis following treatment of a deep carious lesion is shown in (Fig. 4.5).


Fig. 4.4
(Left) Preoperative radiograph of a 12-year-old child showing first mandibular molar with extremely deep caries. (Middle) After excavation and carious exposure and MTA application. (Right): Postoperative 1-year follow-up. Tooth vitality present and well-defined lamina dura in the apical region. Note the formation of tertiary dentin (Courtesy of Dr. G. Bogen)
Fig. 4.5
(a) Preoperative radiograph of a 7-year old child, showing first mandibular molar with deep caries. (b) After excavation and carious exposure and MTA application. (c) Postoperative 3-year follow-up. Tooth vitality present and completed root formation (Courtesy of Dr. G. Bogen)
4.4.3 “Partial” Pulpotomy
As opposed to direct pulp capping, an additional removal of suspected inflamed pulp tissue is performed, and for providing a better seal of the pulp protecting agent, which may be a problem with complicated crown fractures [34]. The definition between a direct pulp cap procedure Class II and the partial pulpotomy appears to overlap in carious pulp exposures. In particular where the treatment is carried out under the conditions of “reversible pulpitis” [35–37], the argumentation of avoiding pulp exposure in the first place is in principle the same as indicated for direct pulp capping Class II. In contrast, a “several-day-trauma” tooth with exposed pulp represents the classical indication for this treatment modality, where the tissue is expected to be superficially and inflamed. In this situation, a superficial removal of pulp tissue is highly beneficial [34]. The completion of an incomplete root complex is shown following a partial pulpotomy (Fig. 4.6).
Fig. 4.6
(a) Preoperative periapical radiograph showing deep carious lesion in the mandibular first molar. (b) Postoperative radiograph taken immediately after treatment with partial pulpotomy and MTA. (c) Tooth: 16 months after treatment. Notice dentine bridge formation in the mesial side of the tooth (arrow). (d) Tooth: 26 months after treatment. Notice the well-formed dentinal bridge (arrow) and the physiological continuation of root formation (Reprinted from Barrieshi-Nusair and Qudeimat [37]; with permission)
4.4.4 “Full” Pulpotomy
In single rooted teeth, the definition includes the surgical amputation of the coronal portion of an exposed pulp, whereas in molar it covers the removal of the entire pulp tissue in the pulp chamber down to the orifices (1–2 mm into in the root canals). The rationale is to completely remove the inflamed pulp tissue. As the prognosis of the vital pulpectomy is very high (see Chap. 8) why then attempt a “full” pulpotomy?
In children it seems advisable to try a conservative pulp-preserving procedure, even in deeply carious permanent teeth with signs of “irreversible pulpitis,” whereby ideal conditions can be established, as already discussed the loss of the vital pulp function is so devastating in teeth with immature apices (Box 4.1). If failure then occurs, apexification or regenerative techniques can still be options. It has been speculated that a full pulpotomy could be a more permanent treatment option in cases of “irreversible pulpitis,” but with established hemostasis, but only case series and case report are available [38, 39].
4.4.5 “Emergency” Pulpotomy
Often “emergency” treatments are closely associated with the practical aspect of lacking time, as the patient arrives unexpected to the dental office and being in acute pain. Thus, a simple treatment is urgently needed to reduce the level of pain in the first place and then a treatment session can be scheduled for completing the final pulpectomy, when proper time is available. An “emergency” pulpotomy has shown to be able to reduce pain in relation to acute “irreversible pulpitis” and without the need of additional medicaments [40]. It is a temporary treatment, but with the surgical pulp approach being the same as the “full” pulpotomy, except for the temporary seal.
4.5 Brief Comments on Capping Agents
For decades the capping agent to promote healing and maintaining viability of the remaining pulp tissue has been a calcium hydroxide-containing material applied either as a base or as a liner. Within the last 20 years, calcium silicate-containing materials have gained more and more focus. In particularly, MTA (mineral trioxide aggregate, Dentsply Tulsa Dental, OK, USA) has been investigated and used intensively. More recently other bioceramic cements have been introduced such as Biodentine (Septodont, Saint Maur des Fosses, France) or iRoot BP (Innovative BioCeramix, Vancouver, BC, Canada). Only limited clinical information is actually available to show potential clinical differences. The reason for selecting the silicate containing materials is therefore based mainly on laboratory studies, where it is shown that these materials may create a better quality of the hard tissue laid down, without so-called tunnel defects. Interestingly, a recent randomized clinical trial [41] showed no differences between the two classic pulp agents, i.e., the calcium hydroxide containing liner Dycal (DeTrey Dentsply, Skarpnäck, Sweden) and MTA. This may also underline that other variables such as patient age and irreversible pulp inflammation may determine the prognosis accounting for problems leading to failure or not. Finally, larger studies may be needed to show actual differences, when it comes to the choice of the very best pulp agent.
4.6 Treatment Guidelines for Vital Pulp Therapy in Molars
4.6.1 Direct Pulp Capping Class I
Pretreatment Data
-
Patient information: subjective evaluation of the region having the present symptom by questioning the patient on the area in focus, intensity, duration, stimulus, relief, and spontaneity. Absence of any signs of “irreversible pulpitis” is mandatory to permit direct pulp capping (Box 4.4).
-
Objective extraoral examination as well as examination of the intraoral soft and hard tissues.
-
Clinical examination showing a tooth that is vital with no lingering or persistent prolonged pain following thermal testing. Other tests such as palpation, percussion, and mobility should have negative findings.
-
Radiographic examination: radiographs showing the involved tooth, furcation, periapical area, and the surrounding bone. No apical pathosis is present.
Diagnosis
-
Reversible pulpitis
Treatment Protocol
-
The tooth is isolated with rubber dam (mandatory for all types of vital pulp therapy).
-
The cavity and the pulp exposure area are gently flushed with saline in order to remove detritus and to establish a clean nonbleeding pulp wound.
-
Direct flush at the exposure should be avoided.
-
Firm pressure with a cotton pellet should be avoided as the removal tends to reactivate bleeding.
-
Hemostasis should be reached within 5 min.
-
The site of the perforation should be noted in the file of the patient for the future plan of restoration.
-
Pulp capping agent is applied at the exposure site and in contact with the tissue (e.g., calcium hydroxide containing base material or mineral-trioxide aggregate (MTA)) followed by a layer of glass-ionomer (Ketac Molar; 3 M ESPE, Glostrup, Demark))
-
A permanent restoration is placed immediately or within a few days in order to prevent secondary bacterial infection.
-
After 6 months, the tooth is checked with respect to subjective symptoms and tooth vitality; in case of absence of any response, a radiographic examination is performed to diagnose potential apical pathosis.
Contraindications
-
If hemostasis is not achieved, direct pulp capping is not done and pulpectomy is indicated (see Chap. 6)

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


