MARIUS STEIGMANN
Chapter XIV
SOFT TISSUE MANAGEMENT FOR AN ESTHETIC ASPECT IN IMPLANT DENTISTRY
However, in our clinical experience, we have found that the interproximal bone presence is an important factor for papillary collapse in a single-tooth environment, depending on the bone mass available and the integrity of the attaching fibers of the adjacent teeth. In the case of multiple implants, the fibrous attachment is lost in the interproximal space and the papilla disappears (this may be prevented by successive extractions).
14.2 Preservation of the alveolus
Dental extraction leads to changes in the size of the alveolar ridge contour. The ridge resorption is more marked on the vestibular surface of the post-extractional socket than on the lingual surface. Preservation of the alveolus at the time of tooth removal is supported in order to minimize the resorption of the alveolar ridge horizontally and vertically, and to facilitate the ideal placement of the implant and consequently the esthetic reconstruction. Various approaches have been described to preserve and improve the ridge contour after subsequent dental extractions, including immediate implants. These may be performed using different graft materials, such as allografts, xenografts, or synthetic biomaterials. Two scenarios have been described in the literature for the preservation of the alveola. The majority have been classified according to the shape of the defect, absence or presence of the buccal plate, and thickness of the vestibular bone plate. However, in the esthetic zone, preserving the alveolus is not enough for the ideal insertion of the implant, from both prosthetic and esthetic points of view. These cases require the so-called alveolar transformation9 in order to create more “bone” buccally than the existing vestibular plate. The grafted bone should be maintained for a long period of time. Consequently, the graft material should be carefully selected (for non- or slow resorption).
In the posterior mandibular and maxillary area, the vestibular plate is thicker than 2 mm.2 These cases do not require grafting for alveolar preservation. The expected bony mass volume makes the ideal placement of the implant possible.
Case 1: Immediate implant insertion without augmentation

Fig 14-1 Persistent temporary molar on the upper arch.
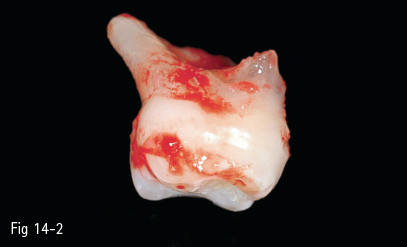
Fig 14-2 Extraction of temporary molar, its roots are resorbed.
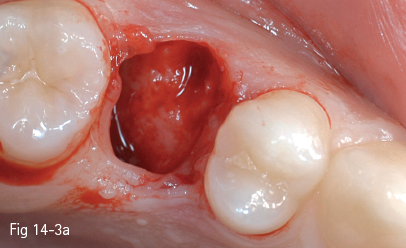
Fig 14-3 a Exploration of the postextraction socket evidences the bone in the interradicular septum. It is possible to insert an implant.
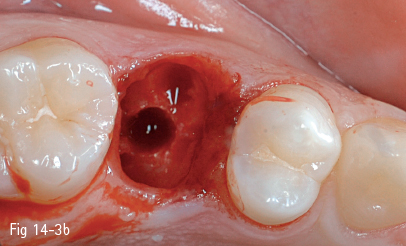
Fig 14-3 b Position is marked for osteotomy.
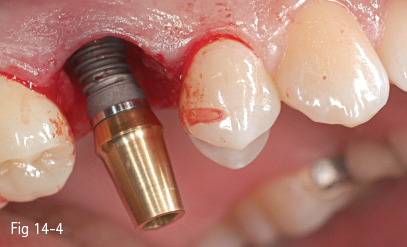
Fig 14-4 Before the final insertion of the implant, its mesiodistal position is checked to ensure that there is sufficient bone thickness to the neighboring teeth, even after a mild circumferential resorption.
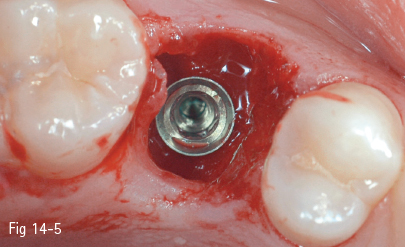
Fig 14-5 Occlusal view of the implant in its final position.
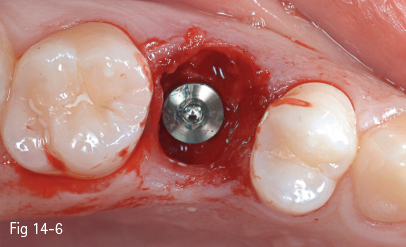
Fig 14-6 The healing cover screw of the implant during the osteointegration period.
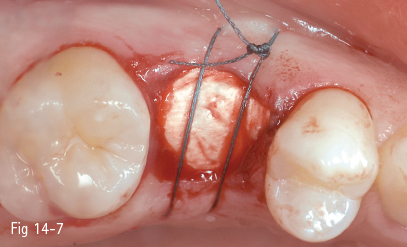
Fig 14-7 The alveolus is covered by a resorbable collagen membrane without any other augmentation material. Criss-cross suture to maintain the membrane in place.
Fig 14-8 a Image immediately after provisional restoration performed 8 weeks after implant insertion – two black triangles may be seen in the interproximal spaces. They will disappear and the papillae will reach the contact point.

Fig 14-8 b Image taken 1 year after prosthetic load – the papillae fill the interproximal spaces down to the contact point.
The thin vestibular plate
When the vestibular plate is thinner than 2 mm, its partial or total resorption may occur.4,5,6 In order to partially prevent the resorption of a thin vestibular plate or the corresponding volume loss, it is necessary to preserve the alveolus. A technique has been described by Sclar (Bio-Coll technique). He describes the filling of the socket presenting defects in the four walls with xenograft and collagen band. No flap or soft tissue manipulation is necessary.9
Case 2: Immediate implant insertion with augmentation

Fig 14-9 Radiograph evidences a deep caries lesion. The tooth is proposed for removal, as it presents crown and root fractures.

Fig 14-10 Tooth is removed by root separation.
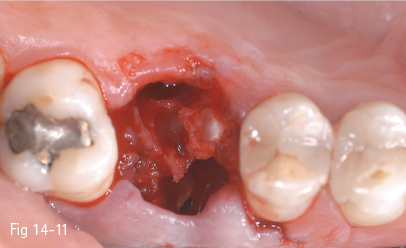
Fig 14-11 The implant insertion point is marked in the interradicular septum.
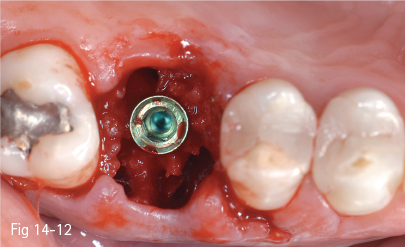
Fig 14-12 The implant in its final position – an increased amount of autologous bone placed around the implant may be noted.
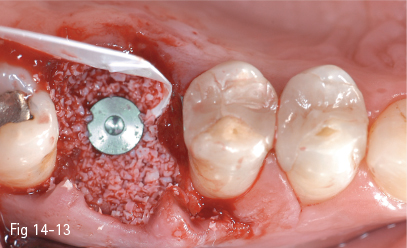
Fig 14-13 In order to prevent the resorption of the vestibular plate, the empty spaces are filled with xenograft and unresorbable membrane.
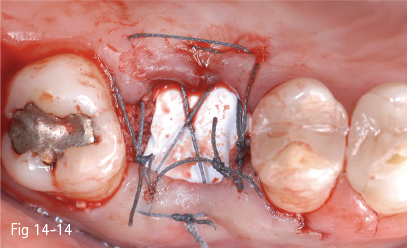
Fig 14-14 The membrane is kept in place by a position suture. Closure is not the objective.
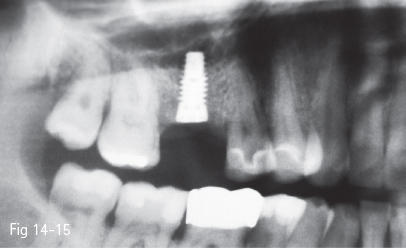
Fig 14-15 Radiograph taken 4 months postoperatively shows good bone regeneration.
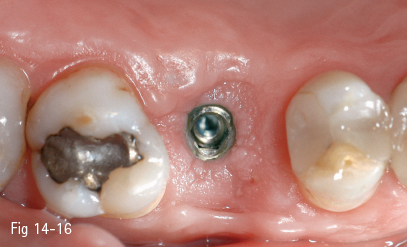
Fig 14-16 Preservation of buccal-palatal dimensions maintained.
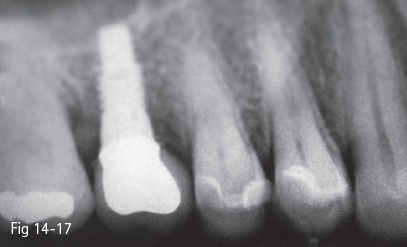
Fig 14-17 Final restoration in situ.

Fig 14-18 Final crown restoration shows an oversized vestibular plate.
The absent vestibular plate
When the vestibular plate is missing, the ridge may be preserved using various types of augmentation materials covered by a membrane, and by manipulating soft tissues for primary wound closure. For cases in which the vestibular plate is absent, Elian et al30 describe the ice cone technique: a membrane is introduced under the soft oral tissue, the socket is obturated with graft material and the membrane is folded to cover the alveolus. The membrane is fixed to the palatal soft tissues by sutures. The technique does not require the primary closure of the socket. Other authors8 prefer an early implant and simultaneous graft. At the time of the tooth removal, no graft material is put into the alveolus. After 6 to 8 weeks of healing, the increase in volume of the soft tissue will help cover the graft associated with the implant insertion.
Jung has proposed the technique of alveolus sealing and excision of soft tissues, in association or without graft materials, in order to preserve the ridge size.10
When the implants are inserted immediately, one of the above-described scenarios may be applied, by adding an implant into the alveolus.
Tooth removal leads to alterations not only of the horizontal dimensions of the hard and soft tissues, but also of the vertical dimensions. The extent of the alterations is important for the treatment planning and restoration of the function and esthetics. In a systematic analysis of the changes of the hard and soft tissues at the level of post-extraction alveloli in humans, data in the literature3–5,6,12 evidences that horizontal bone alterations are followed by anatomical changes of the soft tissues after tooth removal. In the case of a single tooth, soft tissues do not follow bone resorption proportionally to the underlying bone. When several teeth are removed, the soft tissue follows bone resorption proportionally, and consequently new methods of soft tissue preservation should be applied. There is not much in the literature regarding multiple extractions of adjacent teeth.
14.3 The immediate implant insertion
The advantages mentioned in favor of the immediate insertion of the implant are the significant shortening of the healing time, the reduced number of surgical procedures,7 and the optimal availability of the existing bone mass for providing stability to the implant. Moreover, at a microscopic level, it is believed that postextraction osteogenic activity may improve the bone-implant contact when treated implants are used.1,12 Another study, which examined the changes of the hard tissue immediately after implant placement, partially supported the fact that bone defects around the immediate implant could heal. The authors pointed to the fact that although new bone was apparent at the clinical examination, the microscopic examination evidenced a layer of connective tissue. From this it is concluded that an osteointegration process takes place between the bone and the implant.13 In addition, the buccolingual positioning of the immediate implants should be carefully chosen, because, contrary to previous knowledge, the protocol of immediate implants does not prevent the buccolingual resorption of the vestibular bone plate.14
Another drawback of this technique is that a fair amount of bone is necessary, since grafting and augmentation of large amounts of hard and soft tissues are not possible. If the hard and soft tissues are affected by various conditions,8 this technique is not recommended. Certain studies on immediate implant insertion have shown that bone remodeling, bone apposition, and healing also take place in the implant neck area. This is thought to be the reason why no other factors occur to influence the final esthetic result.5 The conclusions of a clinical study performed over 1 year – during which 35 immediate implants were inserted – confirmed that the protocol of immediate insertion may lead to good results regarding the peri-implant soft tissues and esthetic aspect.15
A recent analysis of the clinical results of immediate or early implant insertion concluded that immediate insertion may be successful regarding the implant survival rate. However, the esthetic result may be questionable as there is a high risk of esthetic failure, apart from well-selected cases. Therefore, the authors suggest that these protocols should be used by highly experienced implantologists.16 Immediate restoration could improve the soft tissue outcome.11 This conclusion is in accordance with our own experience; namely, that there is no ideal synchronization between tooth removal and implant insertion, as every patient requires individual assessment. As a general rule, the immediate insertion protocol may be applied for the posterior segments, while late insertion should be preferred for the anterior segments.
Case 3: Immediate implant insertion with augmentation in the anterior zone

Fig 14-19 Tooth 11 is mobile and presents crown lengthening. The firm periodontal biotype, square teeth, flat periodontium, and apical contact points suggest a thick vestibular bone plate.
< div class='tao-gold-member'>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses