Fig. 1.1
Classification of multiple canals in one root by Weine et al. [6]. The original classification of four types was later expanded to the five configurations shown
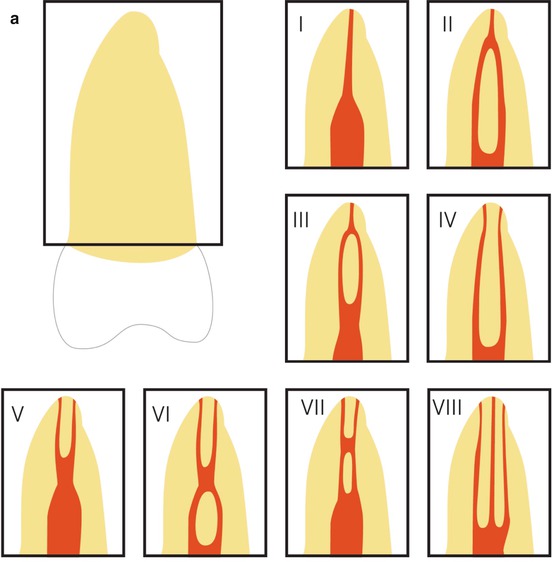
A more detailed classification is recommended to more accurately describing the internal root canal configurations of individual molar roots. One of the most commonly used classifications is the one by Vertucci [7] with eight different canal morphologies (Fig. 1.2a).
However, if there are more than two canals within one root, this classification again is limited. Gulabivala et al. [8] further developed this classification to additional nine morphology types. Especially for describing the root canal formation of the mesial root in mandibular molars types 1, 2, and 3 of this classification is meaningful (Fig. 1.2b).
Another research group [9] extended Vertucci’s classification with additional 14 configurations examining 2800 extracted human teeth. These further developments contribute to the understanding of substantial complexity in root canal configuration.
1.3 Complexity of Root Canal Systems
As Vertucci [1] stated, a root with a tapering canal and a single foramen is the exception rather than the rule. Great complexity of root canal anatomy can be found at every level of the root canal space. It is the result of tooth development mainly after eruption of the tooth to the oral cavity and apical closing [10] due to the apposition of secondary dentin. The primary apposition of root dentin has determined the external shape of the root, and therefore the internal shape will be the very similar: if the external shape is round, the canal will also be round; if the external shape is long oval or kidney shaped, the canal will be long oval or kidney shaped too. Kidney-shaped roots, like in mandibular molars, mainly develop two root canals (Fig. 1.3).
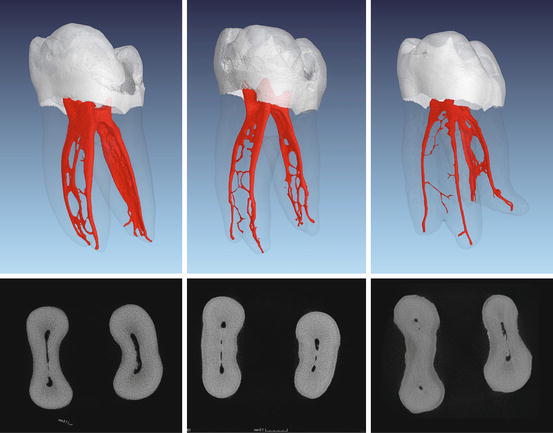
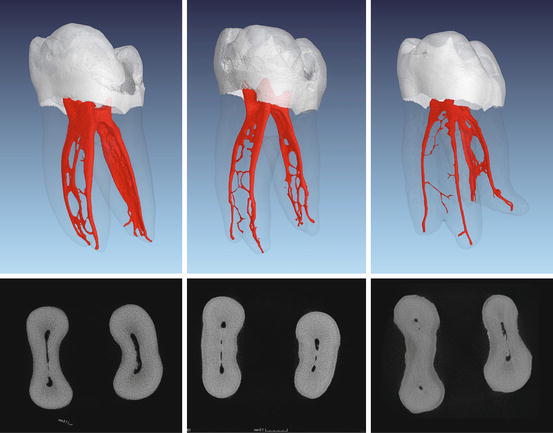
Fig. 1.3
Micro-computed tomography images of extracted teeth from patients of different ages. Three-dimensional reconstructions and corresponding cross sections from the middle third of the roots are shown. Images from left to right: extracted tooth of a young-aged, middle-aged, and older patient, respectively. Note the width of the main canals and the number and size of various ramifications and communications
For example, in mandibular first and second molars the root canal systems were completely defined at 30–40 years of age [10]. Various intercanal communications can still remain and represent one main component of complex root canal anatomy (Fig. 1.3). Others are wide ranges of root canal curvatures, different root canal cross sections, accessory canals, secondary canals, lateral canals, furcation canals, fins and multiple apical foramina, and so-called apical deltas.
More than two decades ago when rotary Nickel-Titanium instruments were introduced to the endodontic market, root canal curvatures have been stated as one of the most common endodontic complexity [11]. With the further development of these instruments and the experience gained by the practitioners, the difficulties of shaping even severely curved root canals have mainly been overcome over the past few years (Fig. 1.4). Taking into consideration that complex root canal systems require proper cleaning and disinfection, the main challenge remains to debride the spaces of the root canal system that cannot be reached by mechanical instrumentation. Especially in mandibular and maxillary molars, the above-mentioned components of complex root canal anatomy are a common finding. In a literature review about tooth survival after nonsurgical root canal treatments [12], the tooth type or specifically nonmolar teeth were found to significantly increase tooth survival.
Fig. 1.4
Micro-computed tomography images of an extracted mandibular and a maxillary molar. Note the severe canal curvatures in both roots of the mandibular molar and in the MB root of the maxillary molar
1.4 The Anatomy of Maxillary Molars
A sufficient root canal treatment in maxillary molars is based on an optimal access to and preparation of all existing root canals. The goal of the treatment is to present the existing anatomy as comprehensive as possible and to widen the root canal system to enable a sufficient disinfection and filling. The anatomy of maxillary molars is very complex and the root canal treatment of this particular group of teeth represents a major challenge for dentists [1]. Carabelli documented the particular anatomy of maxillary molars as early as 1844 [13]. Numerous subsequent publications discussed the complexity of maxillary molar anatomy; most often the mesiobuccal root and the occurrence of a second mesiobuccal (MB2) canal have been in the main focus. In 1917, Walter Hess [14] presented the anatomical complexities with multitude of branches and accessory canals by illustrating in detail the number and formation of root canals. He was the first to relate age and gender of the patients to root canal complexity.
Many studies have shown the anatomy of the upper first molar and especially the presence of a MB2 canal using different techniques [15]. Failures in root canal treatment of this tooth type are often based on untreated MB2 canals [6, 16]. The clinical prevalence of the MB2 canal in maxillary first molars and in second molars is reported up to 93 % and 60 %, respectively [17].
Results from laboratory micro-computed tomography (micro-CT) studies are of special interest for molar anatomy, because this technique allows a three-dimensional presentation and analysis of the root canal system without damaging the tooth structures [18]. Due to modern treatment methods like the use of dental microscopes, options for a successful therapy of difficult root canal anatomies have significantly improved [19]. The location of MB2 canals during root canal treatment of maxillary molars is much more likely by applying the dental microscope and through the use of specialized tools than without [17].
The first maxillary molar is the most voluminous of all teeth: it has four pulp horns and the pulp chamber has usually a rhomboid cross-sectional shape [1]. The second maxillary molar in principle is of similar shape (Fig. 1.5a). However, the pulp chamber is often more long oval, sometimes it is ribbon shaped (Fig. 1.5b).
Fig. 1.5
(a) Micro-computed tomography images of an extracted first (right) and second maxillary molar (left). Note the in general similar shape but the overall smaller volume of the second maxillary molar. Typically, the buccal roots of the second maxillary molar seem to be fused. (b) Clinical images of cases after preparation of all canals in a first (right) and second (left) maxillary molar with rotary instruments. The access cavities provide an overview of all four canal orifices. Note the ribbon-shaped pulpal floor in the second maxillary molar, the entrance of MB2 is located very close to the palatal orifice, a common finding in these kinds of teeth
A maxillary first molar has typically three separate roots and in only about 4 % of the cases just two roots are found. Two or more merged roots occur in about 5 % of all cases. The presence of four roots is extremely rare [15]. In second maxillary molars, merging of roots is much more common. Interestingly, the distobuccal (DB) root canal in second maxillary molars is often difficult to negotiate because an S-shaped DB root is a quite common finding.
Cleghorn et al. [15] evaluated laboratory studies from the years 1914 to 2004 in a literature review of the anatomy of the first maxillary molar. The occurrence of a MB2 was reported to range from 25 to 96 %. Pooled data of 21 studies gave an overall prevalence of roughly 60 %.
It should be taken into consideration that literature data from laboratory studies on the prevalence of the MB2 canals are subject to strong variations due to differences in the experimental design. Thoroughly studying the description of the methods used in these publications is an absolute requirement if someone wants to rely on the found percentages of MB2 canals. Properly designed histological and micro-CT studies could be seen as a gold standard when examining the prevalence of the MB2 canal in extracted teeth. Considering such studies, a prevalence of more than 90 % MB2 canals in the first and more than 55 % MB2 canals in the second maxillary molars should be accepted as clinical reality. Figure 1.6 shows the clinical negotiation of MB2 in a retreatment case with corresponding CBCT imaging.
Fig. 1.6
(a) Clinical image during endodontic retreatment of a first maxillary molar with untreated MB2. The location identification of MB2, the access, preparation, and also filling of the canal system after retreatment of MB1 is shown. (b) Corresponding CBCT scan prior to retreatment of the first maxillary molar is shown in (a). Note the unprepared and unfilled MB2 depicted in different slices of the original dataset (arrows)
This division of the mesiobuccal root canal can take place at different levels and initiate various configurations. Again, it is the result of the apposition of secondary dentin after the formation of the mesiobuccal root. After root formation, the cross section of the mesiobuccal canal resembles a kidney shape with a larger buccal and a smaller palatal part. This explains the smaller diameter of the MB2 canal after the deposition of secondary dentin [20]. Neaverth and coworkers found the prevalence of a second mesiobuccal canal in under 20-year-olds significantly lower than in an age group of 20–40-year-old patients [21].
Due to the secondary dentin apposition, a third mesiobuccal (MB3) root canal could develop (Fig. 1.7). Most often, two of the three canals join somewhere on their travel to the apex (Fig. 1.7a). In the literature, three mesiobuccal root canals have been described to occur up to 7 % in first maxillary molars [22].
Fig. 1.7
(a) Micro-computed tomography images of three extracted first maxillary molars with three mesiobuccal root canals. Note that two of the extracted teeth show MB2 and MB3 joining on their travel to the apex (left and middle), while one of the extracted teeth shows a separate portal of exit (right). (b) Two clinical examples showing the mesiobuccal aspect of access cavities after preparation of three mesiobuccal root canals with rotary instruments
If there are two or more MB root canals, the location on the pulp chamber floor varies greatly; however, the orifice of MB2 is consistently located mesial to or directly on a line between the MB1 and the palatal orifices within about 3.5 mm palatally and 2 mm mesially from the MB1 orifices [23] (Fig. 1.5b).
Very often, the orifice of the MB2 canal is covered by a mesial shelf of dentin, which then needs to be removed to reveal access to this canal (see Chaps. 5 and 6). Below this ledge, the canal path leads toward mesiopalatal before curving back to the center and apically.
This makes the insertion or the negotiation of these canals very challenging. By removing these obstructions and carefully tracking the canal structure toward mesial and apical using ultrasonic tips or long-shank round burs (“troughing or countersinking”), a straight access to the MB2 canal is possible. It could be necessary to extend troughing 0.5–3 mm deep, which risks perforating the pulpal floor toward the furcation area [24]. During initial instrumentation and shaping of MB2 canals, there is the risk of a strip-perforation because of the cross-sectional shape of the MB root (Fig. 1.8). A brushing movement toward the mesial aspect of the root is recommended [24].
Fig. 1.8
Cross-sectional micro-computed tomography images of an extracted first maxillary molar before (upper panel) and after (lower panel) preparation with rotary instruments on four different root levels. Note the shape of the mesiobuccal root and limited radicular wall thickness before and after preparation (arrows)
Once we successfully manage to initially instrument the canal, a further challenge could be to reach the apical foramen in MB2 canals because of two reasons. First, these canals are often very narrow and curved. Second, the chance to encounter a Vertucci class V, VI, or VII in MB root systems is not uncommon (Fig. 1.2a). It remains a challenge for the clinician to recognize a deviation of the MB2 canal in the middle or apical third to the palatal aspect and to successfully prepare such deviations.
According to Vertucci [7], distobuccal roots of maxillary molars show one canal in 100 % of the cases. Other authors described the occurrence of a second distobuccal canal in first maxillary molars with an incidence of 1.6–9.5 %. However, in up to 98 % of these cases, the two canals merge in one apical foramen and only 2 % show two or more canals at the apex of the distobuccal root [15].
1.5 The Anatomy of Mandibular Molars
The mandibular molars, in particular the mandibular first molar, are the most frequently endodontically treated teeth. Their treatment offers a variety of anatomical challenges. These complexities include multiple canals, isthmuses, lateral canals, and apical ramifications. Additionally, the distal dentinal wall of the mesial root is thin and known as the so-called danger zone [27, 28] (Fig. 1.9).
Fig. 1.9
Cross-sectional micro-computed tomography images of two extracted first mandibular molars before (upper panel) and after (lower panel) preparation with rotary instruments at a root level called the danger zone. Note the kidney shape of the mesial roots and radicular wall thickness before and after preparation (arrows)
Harris et al. [28] scanned 22 first molars using micro-CT and showed that 1.5 mm below the furcation in the mesial root radicular wall thickness toward the furcation was smallest with values of 0.81–1.22 mm. Comparable results were obtained by others [29] showing an average dentin thickness of 1.2–1.3 mm measured also 1.5 mm beneath the furcation area.
Using the data from Harris et al. [28] regarding the pulp chamber floor, the shortest and longest distance between the orifices of the mesial canals averaged between about 1.4 and 3 mm. All scanned teeth in that study showed a single distal canal openings at the measured level 1.5 mm coronal to the furcation area, while there are two canals more apical more frequently [30]. The buccolingual dimension of the distal canal was about 2 mm. The average tangential distance from the mesial to the distal canals beneath the pulpal floor was about 4.5 mm.
1.5.1 Additional Roots in Mandibular Molars
In the Caucasian population, the majority of mandibular molars have two roots. An additional root is described as an exception. The presence of an additional distolingual root (radix entomolaris, Fig. 1.10) in mandibular first molars was observed and has been described occasionally [31].


Fig. 1.10
(a) Micro-computed tomography images of an extracted first mandibular molar with a radix entomolaris configuration (left in clinical view, right in approximal view). Note the root canal curvature in the approximal view. (b) Another example of micro-computed tomography images of an extracted first mandibular molar with a radix entomolaris (left in clinical view, right in approximal view). Note the root canal curvature in the approximal view. (c) Clinical retreatment case showing CBCT images of an untreated radix entomolaris with periapical pathosis. The patient was in severe pain at the first office visit. After negotiation and preparation of the untreated root, the patient was free of any symptoms
An additional distolingual root was mentioned first by Carabelli in 1844 [13]. In a review, Abella et al. [32] described a frequency of 14.4 % regarding distolingual roots in mandibular first molars. There was an association to specific ethnic populations. The additional root was found more frequently in populations with Mongolian origin, like Chinese, Inuit, and Native Americans [32]. Cantatore et al. [33] determined frequencies between 5 % and more than 30 % in a population with Mongolian origin. Gu et al. [34] found an occurrence of 32 % in a Chinese population.
Gender-specific differences in the prevalence of an additional root were not recognized. The distolingual root is described either as separate or as partially merged into the other root. The distolingual root was classified according to their root curve in the buccolingual plane [32]:
-
Type I: A straight root
-
Type II: An initial curvature with a subsequent straight course
-
Type III: An initial curvature in the coronal third of the root canal, followed by a second curvature in the middle portion, which proceeds to the apex (Fig. 1.10)
The radix entomolaris is usually smaller than the distobuccal root and has in general a larger angle and a smaller radius of curvature. This makes the preparation of these canals often a difficult task (Fig. 1.10c).
Three-rooted mandibular first molars exhibit usually four separate root canals and accessory canals in the mesial and DB root are found quite often [35]. The most common canal configuration was Vertucci type I for the distal root and Vertucci type IV for the mesial root [32, 35]. A recommended method for identifying a radix entomolaris was described as applying a mesio-eccentric (25°) periapical radiograph or a CBCT [32]. The conventional triangular access cavity should be modified to a trapezoidal shape in the presence of radix entomolaris to facilitate a straight access to the mostly curved root [31]. The average distance between the distolingual and the distobuccal canal opening was 2.93 mm and the average distance between the distolingual and mesiolingual canal opening was 2.86 mm [34]. The mesiobuccal, mesiolingual, and the distobuccal canal exhibited a more oval canal shape, whereas the distolingual canal revealed a relatively round canal shape [35]. The occurrence of an additional mesiobuccal root is called radix paramolaris. The frequency of a radix paramolaris is described with less than 0.5 % [33].
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses