CHAPTER 54
Posterior Iliac Crest Bone Graft
Patrick B. Morrissey,1 Robert A. Nadeau,2 and Eric P. Hoffmeister3
1Department of Orthopedic Surgery, Naval Medical Center, San Diego, California, USA
2Department of Oral and Maxillofacial Surgery, University of Missouri–Kansas City Schools of Medicine and Dentistry, Kansas City, Missouri, USA
3Department of Orthopedic Surgery, Naval Medical Center San Diego; and Uniformed Services University of the Health Sciences, San Diego, California, USA
A method of obtaining large amounts of cortical, cancellous, or corticocancellous autogenous bone from the posterior ilium.
Indications
- When autogenous grafting is desired that requires a high ratio of cancellous to cortical bone (a high volume of osteocompetent cells)
- Hard tissue maxillofacial defects requiring up to 100 mL of uncompressed bone or 5 cm of structural cortical graft
- The presence of a bone void unable to be filled with local tissue-grafting techniques
- The need for augmentation of biologic healing capability (transfer of osteocompetent cells) to fracture or osteotomy sites
- The need for additional osseous structural stability within traumatic or surgical defects
Contraindications
- Local infection at, or adjacent to, the harvest site
- Relative: The obese population is at increased risk for postoperative complications
- Relative: The smoking population is at increased risk for postoperative complications
- Relative: Osteoporotic and osteopenic patients are more likely to sustain intraoperative or postoperative fracture at the site of harvest. The procedure should be approached with caution in this population
Anatomy of the Posterior Ilium
- Osseous structure: The borders of the posterior ilium are the iliac crest superiorly, the posterior superior iliac spine (PSIS) posteriorly, and the greater sciatic notch inferiorly. The bone is slightly concave on its lateral surface with three distinct ridges comprising the posterior, anterior, and inferior gluteal lines.
- Musculature and fascia: The outer surface of the ilium serves as the broad attachment site for the gluteus minimus (between the anterior and inferior lines), the gluteus medius (between the anterior and posterior lines), and the gluteus maximus (from the posterior line to the iliac crest). The gluteus medius and minimus comprise the hip abductors and are innervated by the superior gluteal nerve. The gluteus maximus functions to extend and externally rotate the hip and is innervated by the inferior gluteal nerve. The medial edge of the posterior iliac crest is the attachment site for the lumbodorsal fascia.
- Vasculature: The superior gluteal vessels arise from the posterior division of the internal iliac system and run adjacent to the cortex in the superior aspect of the sciatic notch. They supply the gluteal musculature and are located an average of 63 mm anteroinferiorly from the PSIS and 37 mm inferior to a line drawn perpendicular to the vertical axis at the level of the PSIS.
- Neurologic structures: The superior cluneal nerves originate from the L1–L3 nerve roots and cross directly over the posterior iliac crest. The superior cluneal nerves supply sensory innervation to the superior two-thirds of the buttocks and are located an average of 68 mm anterosuperiorly from the PSIS. The middle cluneal nerves originate from the S1–S3 nerve roots and course from the sacral foramen laterally. The middle cluneal nerves supply sensory innervation to the medial buttock. Excessive traction or laceration to the superior and/or middle cluneal nerves can lead to numbness or symptomatic neuromas.
The greater sciatic notch contains the following nerves: the sciatic, superior and inferior gluteal, internal pudendal, posterior femoral cutaneous nerves, the nerve to quadratus femoris, and the nerve to obturator interuns. The greater sciatic notch is located 6–8 cm inferior to the posterior iliac crest and must not be violated during the surgical approach to the posterior ilium.
Posterior Iliac Crest Bone Graft (PICBG) Harvesting Technique
Posterior Iliac Approach
- Harvesting from the posterior iliac region can be performed with the patient positioned either prone or in the lateral position. For harvesting in a prone position, the patient is intubated supine and then positioned prone, with 210° of reverse hip flexion.
-
Anatomical landmarks are palpated and marked, and include the posterior iliac crest, the posterior superior iliac spine (PSIS), the sacral midline and the site of the proposed incision (Figure 54.3). Local anesthetic containing a vasoconstrictor is injected at the surgical site. The patient is prepped and draped in a sterile fashion.
- A 6–8 cm oblique or curvilinear skin incision (Figure 54.1) originating 3–4 cm lateral to the midline and 1 cm lateral to the posterior superior iliac spine is placed overlying and following the arc of the palpable bony prominence of the posterior iliac crest. The dissection proceeds through skin and subcutaneous tissue until the prominent dorsolumbar (i.e., lumbodorsal or thoracolumbar) fascia is encountered. The dorsolumbar fascia is transected, and dissection continues to the posterior iliac crest. A full-thickness flap, including the dorsolumbar fascia, gluteus maximus muscle, and periosteum, is elevated 1 cm lateral to the PSIS to expose the outer cortex of the posterior ilium (Figure 54.4). Preserving the continuity of this single, stout layer will greatly facilitate closure of the surgical site once the graft is obtained and will minimize postoperative complications. Preserving the PSIS and its attachments (sacroiliac ligaments) will minimize postoperative pelvic instability and will aid in maintaining a safe distance from the sacroiliac joint.
- Subperiosteal elevation continues lateral to the PSIS and inferior to the posterior iliac crest for approximately 4–6 cm, depending on the size of the graft to be harvested. Care is taken with inferior reflection of the tissues to minimize damage to the structures within the sciatic notch and to the superior gluteal vessels.
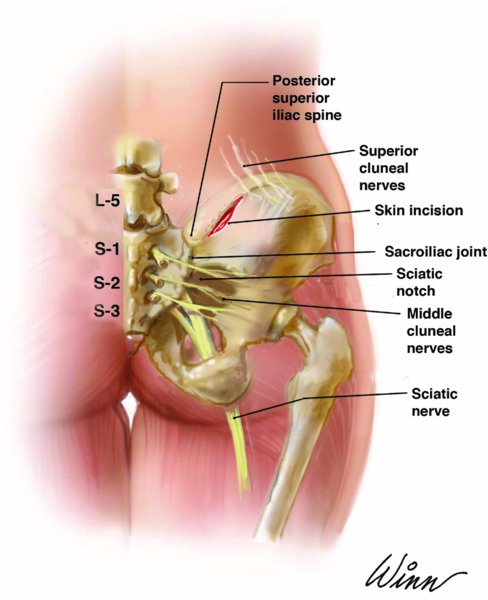
Figure 54.1. Anatomy of the posterior ilium and incision location for posterior iliac crest bone graft harvest.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


