Short Face Growth Patterns
Maxillomandibular Deficiency
• Treatment Indications and Objectives
• The Role of Growth Modification in the Preadolescent Patient
• Postsurgical Orthodontic Maintenance and Detailing
• Complications, Informed Consent, and Patient Education
• Malocclusion after Orthodontics and Orthognathic Surgery
• Temporomandibular Disorders: The Effects of Orthodontics and Orthognathic Surgery
A frequently seen pattern of facial disharmony has the common denominator of a significant degree of vertical and horizontal (sagittal) deficiency in the maxilla and mandible. Measuring the ratio of the lower facial height (i.e., the subnasion to the menton) to the upper facial height (i.e., the glabella to the subnasion) will confirm that the lower height is diminished. The height of the alveolar process in both jaws is reduced.23 The visual presentation of the face includes an apparent redundancy of the soft-tissue envelope of the lower face, thereby creating “chubby cheeks” in the adolescent and a prematurely aged look by early adulthood.
Clinical examination of the individual with a short face growth pattern will generally confirm a pseudoprominence of the nose; an acute nasolabial angle; a measurable and visually perceived short lower facial height with a disproportionate facial width-to-height ratio; and either a prominent pogonion (more frequent with a Class I deep bite) or a weak chin (more common with a Class II excess overjet).3,10,11,20,21,35,39,40 Normally, there is a 1 : 2 relationship between the distance from the base of the nose to the upper lip and the distance from the lower lip to the chin. In the individual with a short face growth pattern, the relationship is closer to 1 : 1.15,42,43,56 The labiomental sulcus is deep and the lower lip is everted, thereby further confirming the degree of mandibular deficiency. The maxillary incisors are often completely covered by the upper lip, which creates an edentulous appearance in repose and an unfavorable “no gingiva” smile. With the teeth in occlusion, the oral aperture appears closed and the upper lip projects forward, often in front of procumbent incisors. Individuals are frequently described as having a sad or unhappy look in repose as a result of the downturned oral commissures and the closed aperture. The reduced lower facial height causes the everted and prominent lips that would otherwise have appropriate shape and volume if the facial height and horizontal projection of the jaws were restored. In the profile view, the nose appears long and prominent. There is often a lateral flaring of the nostrils with a “hanging columella.”
Classically, there is a deep bite with either marked anterior crowding or excessive flaring with less dental crowding.34 There may be a Class II malocclusion with greater than average overjet.50,51 If so, the mandible has greater deficiency than the maxilla, and the pogonion will lack prominence. Individuals with Class I deep bite without excess overjet are more likely to have a retropositioned A-point as compared with the B-point (i.e., a counterclockwise rotated maxillomandibular complex) and a prominent pogonion. The maxillary and mandibular planes are often nearly horizontal, which results in a “square jaw” facial appearance.
Functional Aspects
• Articulation errors in speech and altered swallowing mechanisms that result from the small jaws, the Class II deep-bite malocclusion, and the limited intraoral volume for the tongue are expected (see Chapter 8).
• Difficulties with chewing and with lateral and protrusive mandibular movements as a result of the Class II deep-bite malocclusion are expected (see Chapter 8).
• A spectrum of upper airway sites of obstruction often exists with the short face growth pattern. This includes obstructions at the intranasal, palatopharyngeal (retropalatal), and glossopharyngeal (retroglossal) locations. The incidence of obstructive sleep apnea is increased in this patient population and should be ruled out (see Chapter 10 & 26).
• Detrimental long-term effects on the dentition and the periodontium as a result of any traumatic malocclusion, the crowding of the teeth in the limited alveolar housing, and previous camouflage orthodontic treatment may be seen (see Chapter 5 & 6).
• A higher incidence of temporomandibular disorders in the form of masticatory muscle discomfort as a result of the short facial height and the deep-bite malocclusion has been reported (see Chapter 9).
Clinical Characteristics
• Absence of maxillary tooth show beneath a relaxed upper lip
• Limited tooth and no gingiva show with broad smile
• An apparent fullness of the cheeks and a squareness of the overall face
• An apparent prominent and elongated nose when viewed in profile
• Procumbent everted lips, turned down corners of the mouth, and a closed aperture
• An excessively deepened and elongated labiomental fold
• Soft-tissue bunching that eventually results in perioral creases (i.e., marionette lines)
• Early and deep jowl formation by middle age
• Premature loss of any semblance of an attractive neck–jaw angle
Radiographic Findings
• The total anterior facial height is decreased (i.e., from the nasion to the menton).
• The lower anterior facial height is short (i.e., from the subnasion to the menton).
• Horizontal retrusion is measurable at the A-point and the B-point in both jaws.
• Disproportion in the ratio of the facial width to the facial height is measurable on an anteroposterior cephalometric radiograph or a computed tomography scan.
• Excessive procumbency of the maxillary and mandibular incisors is frequently measurable.
• Excessive flattening (i.e., counterclockwise rotation) of the maxillary and mandibular planes is frequently measurable.
• Decreased alveolar bone height associated with the maxillary incisors is measurable (i.e., the distance from the floor of the nose to the incisal edge).
• Decreased alveolar bone height associated with the mandibular incisors is measurable (i.e., the distance from the short menton to the incisal edge).
Treatment Indications and Objectives
The indications for treatment in a patient with a short face growth pattern may be to improve function (e.g., occlusion, chewing, swallowing, speech, breathing, lip posture), but another compelling aspect is typically the enhancement of facial aesthetics. The visually aesthetic advantages of the surgical lengthening and projection of the short and retrusive lower face toward Euclidian proportions are immediately apparent and do not require quantification.32,33,58
To restore facial proportions and preferred facial aesthetics, there must be both vertical and horizontal expansion of the maxillomandibular complex.54 Accomplishing these objectives will eliminate cheek and lip region bunching and distortion and restore a pleasing soft-tissue envelope. When this is done, a youthful oral aperture is restored. The corners of the mouth are no longer downturned, and the lips will be separated when they are at rest. The upper vermillion increases in volume, and the labiomental fold flattens. The maxillary incisors can be seen in repose, and the gingiva is visible with smile. The nose no longer appears excessively prominent, and the nasolabial angle improves. The jowls diminish, and the length-to-width ratio of the face is restored. The shape of the face changes from square to oval with the restoration of the natural contours and attractive ogee curves. The overall facial aesthetic changes from sad and older appearing to younger looking and more attractive (Figs. 23-1 through 23-7).


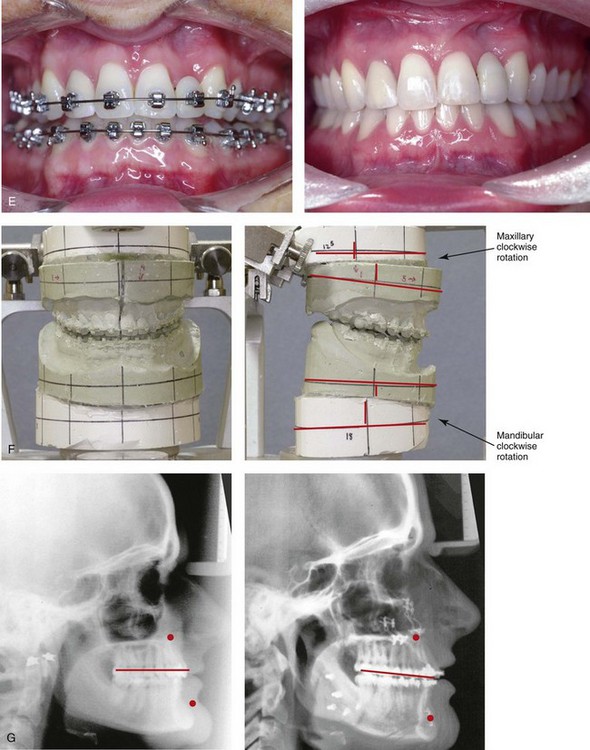
Figure 23-1 A 28-year-old woman arrived for a third surgical opinion regarding a reduction rhinoplasty and reduction genioplasty. The diagnosis of a short face growth pattern was made. Maxillomandibular advancement and vertical lengthening were recommended. The patient agreed to a surgical approach with perioperative orthodontics. Her surgery included maxillary Le Fort I osteotomy in segments (vertical lengthening, horizontal advancement, arch expansion and clockwise rotation) with interpositional grafting; sagittal split ramus osteotomies (horizontal advancement and clockwise rotation); and osseous genioplasty (vertical lengthening) with interpositional grafting. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique facial views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views before and after treatment. Only minimal change in the occlusion was required. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.


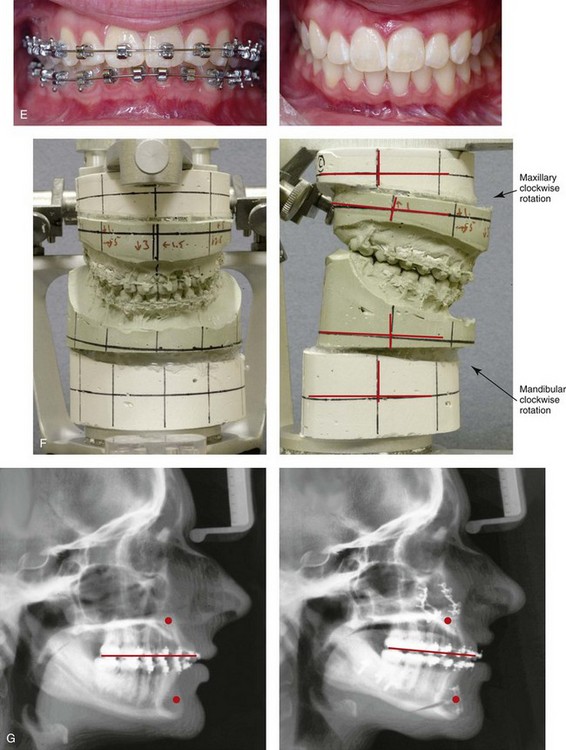
Figure 23-2 A 16-year-old girl arrived with her parents for surgical evaluation. She requested a reduction rhinoplasty and a chin implant. A diagnosis of maxillomandibular deficiency with a Class II excess overjet malocclusion was made. She agreed to a surgical and (redo) orthodontic approach. No extractions were carried out, and a degree of incisor proclination was tolerated. The patient’s surgery included maxillary Le Fort I osteotomy (horizontal advancement, vertical lengthening, and clockwise rotation) with interpositional grafting; sagittal split ramus osteotomies (horizontal advancement and clockwise rotation); and osseous genioplasty (vertical lengthening) with interpositional grafting. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before and after treatment. Only minimal change in the occlusion was required. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.



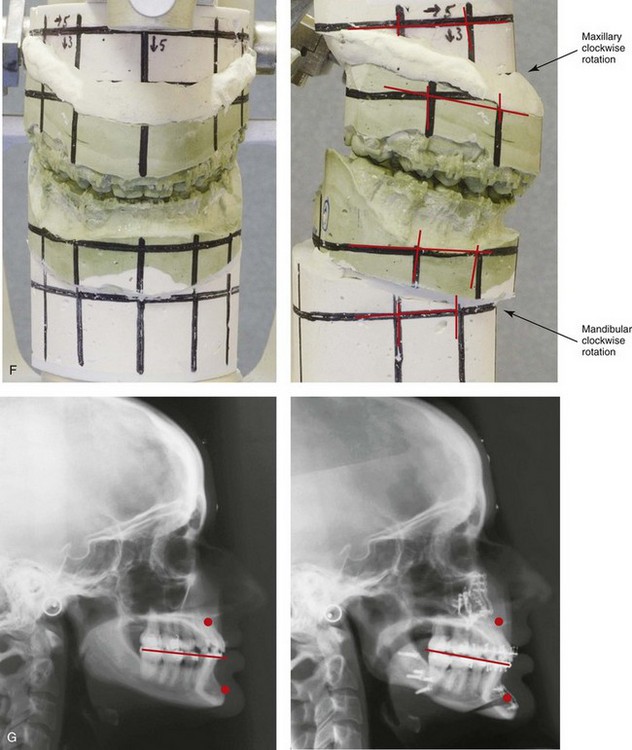
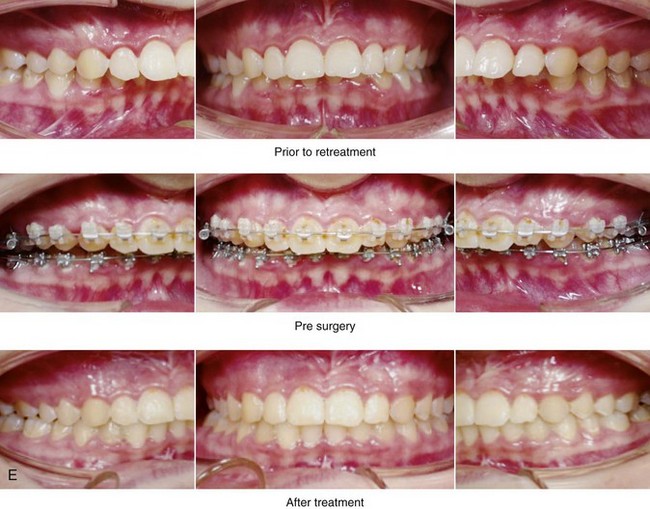
Figure 23-3 A 24-year-old woman arrived for evaluation. She had previously undergone four bicuspid extractions and orthodontics to neutralize her occlusion during her high school years. Analysis confirmed a short face growth pattern that accounted for the apparent large nose, weak profile, obtuse neck–chin angle, and edentulous look. She agreed to a combined (redo) orthodontic and surgical approach. The patient’s surgery included maxillary Le Fort I osteotomy (horizontal advancement, vertical lengthening, and clockwise rotation) with interpositional grafting; sagittal split ramus osteotomies (horizontal advancement and clockwise rotation); and osseous genioplasty (vertical lengthening and minimal horizontal advancement) with interpositional grafting. Minimal change in the occlusion was required. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before retreatment, with orthodontics in progress, and after reconstruction. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.



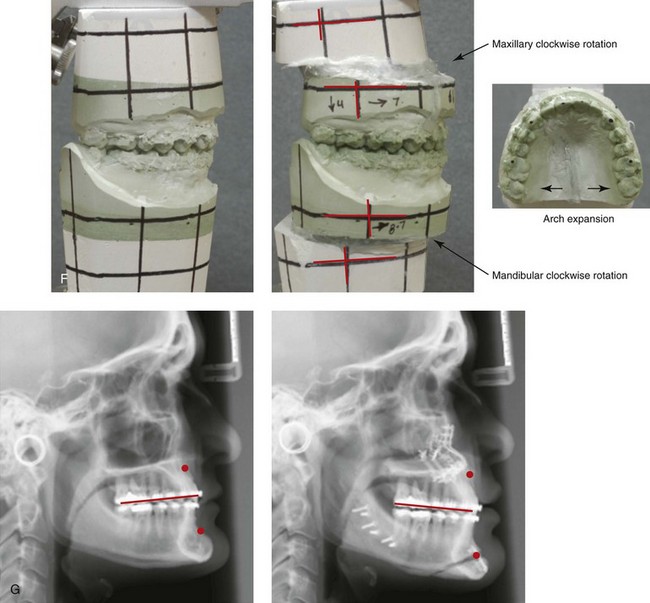
Figure 23-4 A woman in her late 20s arrived for the evaluation of her edentulous look. She had previously undergone orthodontic neutralization of her occlusion during her high school years. Analysis suggested a short face growth pattern that accounted for her apparent large nose, protrusive chin, and edentulous look. The patient also complained of nasal obstruction, restless sleeping, and daytime fatigue. Examination confirmed septal deviation and enlarged inferior turbinates, and an attended polysomnograph documented mild obstructive sleep apnea. She underwent a combined (redo) orthodontic and surgical approach. The patient’s surgery included maxillary Le Fort I osteotomy in segments (horizontal advancement, vertical lengthening, arch expansion and clockwise rotation) with interpositional grafting sagittal split ramus osteotomies (horizontal advancement and clockwise rotation); osseous genioplasty (vertical lengthening and minimal horizontal advancement) with interpositional grafting; and septoplasty and inferior turbinate reduction. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before retreatment, with orthodontics in progress, and 1 year after reconstruction. Minimal change in the occlusion was required. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses