Individualized Orthodontic Diagnosis
Flavio Andres Uribe, Taranpreet K. Chandhoke, Ravindra Nanda
The term diagnosis is defined as the identification of a disease by careful investigation of its symptoms and history.1 While not a true disease per se, malocclusions are the “disease” processes of orthodontics and the central focus of orthodontic diagnoses. Malocclusions can have esthetic and functional implications, and an accurate diagnosis is required to best understand their etiology and the treatment options for managing the abnormality. From an esthetic standpoint, there are psychological implications associated with malocclusions related to social acceptance and success.2 From a functional standpoint, mastication, speech, and protection of the structures in the entire stomatognathic system can contribute to or be the result of the malocclusion that is present.
To define the abnormal or pathological characteristics of the malocclusion, there needs to be an appreciation of what is defined as “normal.” This is a particular challenge because what is considered normal falls within a wide range. Variability is found throughout nature, so defining the limits of the normal range can be difficult. While esthetic perceptions vary through history and among individuals, races, and cultures, ideal occlusion and its functional implications are characterized by strict morphological features. Thus the definition of a normal occlusion involves both objective and subjective components.
Extensive research has determined the characteristics of normal functional occlusion. Concepts such as cusp-to-fossa or cusp-to-interproximal space occlusion, lateral and anterior guidance, and mutually protected occlusion are described comprehensively in other textbooks.3 However, the criteria for ideal occlusal function are better defined in comparison to ideal esthetic values. Most of the occlusal concepts accepted today are derived from the assumed premise that good anatomy (i.e., good occlusal interdigitation) is analogous to proper function (Fig. 1-1).
From the esthetic standpoint, orthodontists base their judgment on cephalometric norms obtained many decades ago from population samples with vaguely defined parameters of esthetics. In general, these studies assumed that good occlusion was directly related to good facial esthetics. Although these measurements provide some objective guidelines that can be used to start defining how each patient differs from the norm, there are limitations to these analyses. Furthermore, it is not the absolute numeric amounts and their variation that dictate treatment but the accurate interpretation of these and all data obtained from the clinical examination and other patient records.
To accurately diagnose a malocclusion, orthodontics has adopted the problem-based approach originally developed in medicine.4 Every factor that potentially contributes to the etiology, might contribute to the abnormality, or might influence treatment should be evaluated. Information is gathered through a medical and dental history, clinical examination, and records that include models, photographs, and radiographic imaging. A problem list is generated from the analysis of the database that contains a network of interrelated factors. The diagnosis is established after a continuous feedback between the problem recognition and the database. Ultimately, the diagnosis should provide some insight into the etiology of the malocclusion (Fig. 1-2).

Figure 1-2 Steps in diagnosis and treatment planning.
The diagnosis and problem list is the framework that dictates the treatment objectives for the patient. Once formulated, the treatment plan is designed to address those objectives, from the mechanics to the sequence that will be used.
From the treatment objectives perspective, one or more treatment options can be developed to address each objective. Each treatment option will have advantages and disadvantages for the patient. During the process of obtaining informed consent from the patient, clear descriptions of the advantages, disadvantages, and risks of each treatment plan should be presented and the patient will ultimately determine the final treatment plan. The treatment plan then dictates the mechanics plan designed to achieve the desired goals with the greatest efficiency and fewest side effects.
This chapter discusses some of the objective measures that define the range of normality, both from an occlusal and a dentofacial standpoint. It is important to know that although emphasis is placed on the entire dentofacial complex, there are limits to the amount of correction that can be achieved with orthodontic treatment.
The clinician has to work within certain constraints and understand the limitations of the various treatment options. For example, the soft tissue envelope allows for only a certain amount of correction. If major movements are needed, they may require other treatment options such as surgery or skeletal anchorage, which, although able to achieve a wider range of movements, are limited by the boundaries of the soft tissue envelope. The primary goal should be to achieve the best possible facial balance and functional occlusion.
Finally, while great care is taken in formulating a detailed treatment plan, it is important to realize that the diagnosis and treatment plan are dynamic processes. As the plan is executed, continuous monitoring and effective evaluation of the objectives are needed. Appropriate reassessment, adjustment, and corrective measures to the original plan are crucial if all specific goals and not only the occlusal goals are to be achieved.
As described above, very precise collection of data is needed to achieve a proper diagnosis. The database should include a thorough medical and dental history, a set of models, the necessary radiographs, and a clinical examination accompanied by extraoral and intraoral photographs.
Clinical Examination
Medical and Dental History
“What is the patient’s chief complaint?” This question is the basis of the anamnesis. At a minimum, the treatment plan should aim to address this important fundamental component of the patient’s initial screening. The clinician is responsible for accurately understanding and addressing the chief complaint. Some patients will have very specific goals for treatment while others will provide more generalized expectations. Clear communication is the key to understanding a patient’s objectives. With young patients, it is usually the parents who voice their complaint about the child’s teeth. Commonly, the child is lacking in motivation or is too shy to express himself or herself. The parents’ concerns should be a major consideration but the child should also be involved through a set of simple questions that will guide the clinician in discovering the child’s motivation for treatment, if any.
The medical history gives pertinent information about the physical well-being of the patient. Numerous medical conditions can affect treatment in one way or another (Table 1-1).5 For example, a history of a cardiac malformation or anomaly may be an indication for premedication before certain orthodontic procedures.6 A history of rheumatoid arthritis can have direct implications on the temporomandibular joint (TMJ) and thus on the occlusion. A patient with hemophilia may opt for a nonextraction treatment approach. All of these conditions may affect the delivery of treatment in the various phases: pre-treatment, treatment, and post-treatment.
TABLE 1-1
Medical Conditions to be Considered in Orthodontic Treatment
| Medical Condition | Implications | Action |
| Allergies | Allergic reaction | Determine material causing allergy and substitute a nonallergic material |
| Asthma | Root resorption | Monitor every 6 months for evidence of EARR |
| Coagulation disorders | Bleeding risk | Avoid treatment plans involving extractions if possible |
| Diabetes | Periodontal disease | Monitor adequate control of diabetes. Manage with a periodontist |
| Epilepsy | Gingival hypertrophy (medications) | Monitor excellent plaque control. Manage with a periodontist for possible surgical intervention during treatment |
| Heart valve conditions | Endocarditis | Premedication when fitting bands |
| High blood pressure patient taking calcium channel blockers | Gingival hyperplasia secondary to medications | Monitor oral hygiene. Complement brushing with chlorhexidine |
| HIV | Periodontal disease, opportunistic infections | Consult with physician about patient’s general condition. Monitor oral hygiene and periodontal status |
| Leukemia | Mucositis, oral infections | Remove appliances until remission (consult physician) |
| Osteoporosis | Bisphosphonate-related ONJ, delayed tooth movement | Determine formulation of medication and explain potential limited outcomes of treatment to patient |
| Physical or mental handicap | Gingivitis, relapse (muscle hyperactivity or hypoactivity) | Electric toothbrushes may aid in oral hygiene. Consider mechanics plan in which manual dexterity is not needed (noncompliance mechanics) |
| Rheumatoid arthritis | TMJ degeneration | Monitor TMJ. Manage with an oral surgeon if severe arthritic degeneration |
| Transplant patient | Gingival hyperplasia related to immunosuppressant drugs | Monitor oral hygiene. Consider chemical complement to brushing such as chlorhexidine |
| Xerostomia (primary or secondary) | Caries | Monitor for loose appliances. Consider fluoride rinses as an oral hygiene supplement |
EARR, External apical root resorption; HIV, human immunodeficiency virus; ONJ, osteonecrosis of the jaws; TMJ, temporomandibular joint.
Any metabolic disorder, such as diabetes, should be well-controlled before and during treatment, as healing is greatly hindered in uncontrolled types of diabetes.7
Another common medical condition of concern, especially in young patients, is asthma, not only because of the respiratory implications, but also because there is some evidence that patients with asthma who undergo orthodontic treatment have an increased incidence of root resorption.8
The above are some of the more common medical conditions, but it is important that all medical conditions be reviewed and further investigated (e.g., with a phone call to the patient’s physician) if needed, as they may affect the treatment directly or indirectly. A more extensive review of these and other common medical disorders related to orthodontics can be found elsewhere.5
Another part of the medical history review specific to female patients is pregnancy. It is usually best to delay treatment until the pregnancy is over. The three basic reasons for postponing treatment are that radiographs usually are not recommended during pregnancy, there is an increased possibility of gingival hyperplasia due to hormonal influence, and in some instances the future mother’s nutrition may be compromised as pain is elicited by tooth movement.
Other important information related to the medical history is the list of medications the patient may be taking and the existence of any allergies. Medications such as phenytoin (anticonvulsant), nifedipine (calcium channel blocker), and cyclosporine (immunosuppressive) need special attention, as they have the potential to cause a hyperplastic gingival response.9 Some medications may also influence the progress of orthodontic treatment. Among these are oral bisphosphonates, which are used to treat osteoporosis in perimenopausal women through inhibition of osteoclastic activity, thereby reducing bone resorption. Proper osteoclastic activity is necessary to ensure physiological tooth movement. Local administration of bisphosphonates has been shown to significantly delay tooth movement and space closure in rats.10,11 Studies have shown that patients taking bisphosphonates have increased treatment times, especially in extraction cases, and potentially compromised outcomes due to difficulty in achieving root parallelism and complete space closure.12 There is an increased risk of osteonecrosis of the jaws (ONJ) with bisphosphonates, specifically with an intravenous formulation. However, this risk is significantly lower in patients taking oral bisphosphonates.
Potential allergies to the alloys used in orthodontics should also be identified. Hypersensitivity to nickel has been reported with a prevalence of up to 28%.13 Allergies to other metals used in orthodontics, such as chromium and cobalt alloys, have also been reported.14 It is important to know the nature of the reaction to each allergen. Allergies related to the airway are also a significant finding, as they impair normal nasal breathing thus potentially affecting the growth and development of the jaws.15
The use of tobacco should also be ascertained from the medical history. It is not uncommon to encounter adolescent and adult patients who smoke. Smoking can have an adverse effect on the periodontal condition of patients,16 is a risk factor for periodontal disease, and has been shown to delay wound healing.17 Health providers also have an important duty to dissuade teenagers and adults from tobacco use.
With more adult patients seeking orthodontic treatment, it is critical to determine whether these patients are periodontally stable for fixed treatment. Fixed appliance therapy will likely aggravate an underlying peridontal problem due to poor oral hygiene and activation of bone remodelling.18 The orthodontist should take the necessary steps to minimize deleterious effects and also set realistic expectations for these patients. A full mouth series should be evaluated prior to the start of treatment and a focused clinical exam should be done to determine the periodontal status. Collaboration with a periodontist may be necessary to determine whether the patient is periodontally healthy for orthodontic treatment. If the patient has periodontitis, further periodontal therapy is indicated, which may involve a combination of therapies of scaling and root planing or open flap debridement depending on the severity of the disease.19 It may also be indicated to increase the frequency of prophylaxis and monitoring by a general dentist or periodontist during fixed appliance treatment to ensure that the periodontal status remains stable.
Growth and Development
A specific section in the medical and dental interview should be dedicated to growth and development information. Most pediatricians keep a growth record of every child from birth (Fig. 1-3). A growth chart classifies the child under a height and weight percentile for comparison to the established norms for gender and chronological age. More importantly, the growth chart highlights any accelerations or peaks of growth that may have occurred. With this information, the objective is to evaluate the skeletal maturational level of the patient. The underlying rationale for this information is to properly time orthodontic treatment to the period that would be most efficient and effective.20 This implies that treatment will rely not only on tooth movement, but also on modifying growth to achieve a wider range of movement, thereby correcting larger dentofacial discrepancies.
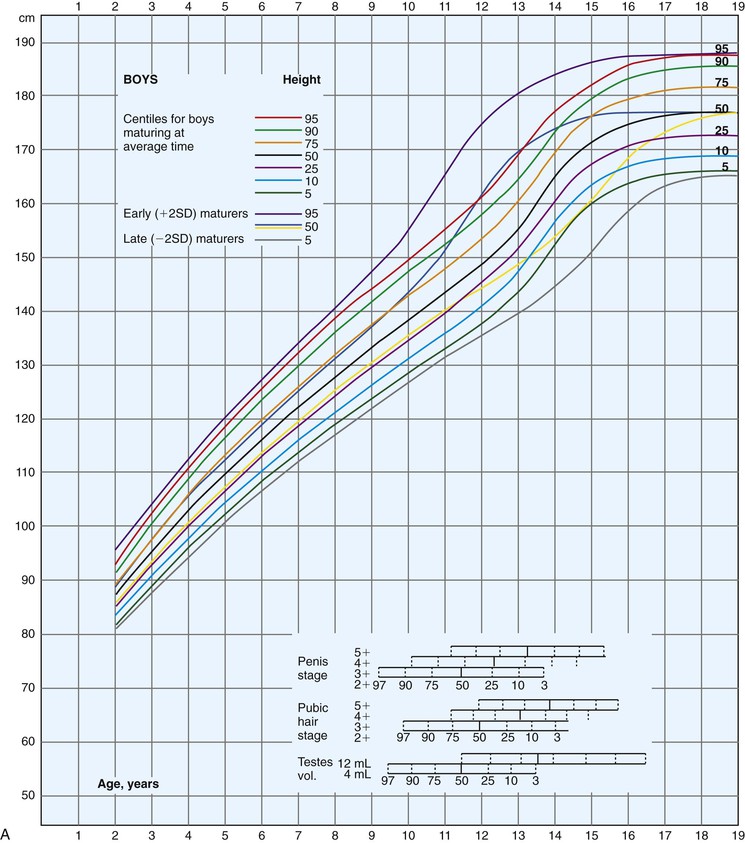

Figure 1-3 Growth curves for (A) boys and (B) girls (height and weight). SD, Standard deviation. (Modified from Tanner JM, Davies PS. Clinical longitudinal standards for height and height velocity for North American children. J Pediatr. 1985;107:317–329.)
The pubertal growth spurt is associated with a differential maxillomandibular growth that involves a more anterior positioning of the mandible (Fig. 1-4). The timing of this spurt has been of interest to orthodontists. During this period the orthodontist should be able to influence growth of the mandible and the midface by mechanically affecting the environment. Experiments in animal models have shown the possibility of mandibular growth enhancement during this period.21 Unfortunately, there is no clear evidence that this additional mandibular growth enhancement is predictably achievable in humans.22 Although clinical studies have shown impressive results at the occlusal level, the results may be the sum of a combination of small orthopedic and dental movements.23,24 Some of the orthopedic movements involve remodeling within the temporal bone that is difficult to quantify with traditional research methods.25
Chronological age, dental development, and eruption sequence are not good indicators of skeletal maturity. Biological indicators, such as menarche (females), voice change (males), hand-wrist ossification sequence, metacarpal ossification sequence, cervical vertebrae morphology, and statural growth curves, have been used to evaluate general skeletal craniofacial maturity.20,26–28 Studies have shown a close correlation between peak height velocity and maximum acceleration in growth in the maxilla and mandible.21,26,28,29
Currently, there are no methods that can accurately predict the extent of craniofacial growth that a patient will ultimately achieve. This predictive inability becomes a problem in young patients with significant maxillomandibular discrepancies. For these patients a decision between a surgical approach or a growth modification approach is not simple. Moreover, these treatment strategies (surgery and growth modification) differ in timing, objectives, and often the direction of tooth movement. Some studies suggest that weak correlations can be drawn between final craniofacial form of growing children and their parents and other siblings.30,31
Although the absolute amount of growth cannot be predicted accurately, the direction of growth is more predictable. It has been shown that facial patterns are maintained.32,33 Skieller et al. also published findings related to the morphology of the mandible in the prediction of growth patterns.34 Some controversy relates to their findings, as their sample was made up of individuals with extreme patterns of vertical growth. Therefore the applicability of these predictive methods to individuals with less severe aberrations in their growth pattern might be limited.35
Finally, information regarding the timing of active growth cessation is important for young patients needing maxillofacial surgery. Radiographic films can be used to evaluate this feature. Use of cervical maturation indicators and hand-wrist films can provide further information on the stage of the patient’s growth and is discussed later in the chapter. The best method to confirm that no further growth will occur in the craniofacial region is to take two sequential lateral head films with a 6- to 12-month interval; the superimposition of these radiographs should reveal no bony changes.36
Factors Influencing Craniofacial Growth
It is well known that many conditions affect the growth and development of the craniofacial complex. Knowing the etiology of the malocclusion is of prime importance for the diagnosis and eventual success of treatment. The etiology of the malocclusion is often multifactorial. In general, the etiologic factors can be categorized into genetic factors, environmental factors, or a combination of the two. Genetic information can be gathered from the interview with the guardian of the child patient or from the adult patient. This information is more important in patients where syndromes or extensive craniofacial deviations are present. Also, as mentioned, the parents’ information may give some insight into the craniofacial form at the end of growth. The genetic component is also of further importance as it relates to abnormalities of tooth development and morphology, such as canine impaction, congenitally missing teeth, and abnormalities in tooth shape.37,38
Numerous environmental factors have been attributed to the etiology of malocclusions. The classic example is the habit of thumb-sucking. A long-term applied force (pressure) has been shown to affect skeletal hard tissues. The tissues of the musculature can apply constant low forces and result in adaption of the adjacent bony structures.39 Muscular dysfunction by either hyperactivity or hypoactivity in certain disease processes also may affect the normal growth and development of the jaws.40 If the forces exerted by the muscles are not in equilibrium, the net effect will be reflected in the hard tissues in the form of displacement and eventually conditions leading to malocclusion and maxillomandibular skeletal discrepancy.41,42
Frontal View
Traditionally, orthodontists have paid little attention to facial analysis from the frontal view and instead have focused mostly on anteroposterior changes (i.e., Angle classification). With the surge in three-dimensional (3D) imaging technology more information from the frontal view, especially relating to the soft tissue analysis, will be available in the future.43
When describing a patient from the frontal view, an overall assessment of the patient’s symmetry is made. Attractiveness and pleasing facial esthetics have been linked to certain proportions and symmetry.44,45 Minor asymmetries exist in all patients, even those who are visibly symmetrical, likely due to skeletal and soft tissue compensations during growth (Fig. 1-5).

Figure 1-5 Cone beam computed tomography (CBCT) images from normal, Class I adolescent patients. Minor skeletal asymmetries are evident in these patients when examined in 3D.
Ideal facial proportions have been described since ancient times by Roman and Greek artists. Horizontal as well as vertical lines are used as reference planes to evaluate these proportions. The horizontal planes, such as the interpupillary, interauricular, alar base, and occlusal planes, should be parallel to each other and special attention should be paid to the presence of cants (Fig. 1-6). The proportions between these horizontal planes can also be evaluated on the profile view. From the frontal view the vertical reference lines are more important since it is only from this view that the transverse dimension can be evaluated (Fig. 1-7).

Figure 1-6 Maxillary cant evidenced at smile. More gingival display is appreciated in the upper right buccal segment than in the left buccal segment.

Figure 1-7 Vertical reference lines used to evaluate symmetry. The face is divided into six portions in the transverse analysis. The yellow line is an estimate of the facial midline.
Midline
The frontal view is also helpful in the evaluation of the relationship between the facial and dental midlines. It is important to note that analysis of the facial midline can be difficult, especially in patients with deviated nasal septums (Fig. 1-8, A). Thus the commonly used technique of placing a piece of dental floss vertically through the facial midline to relate it to the dental midline can be deceiving. A better method is to assess the relationship between the Cupid’s bow and the dental midline (Fig. 1-8, B).46 Hence the dental midline can be related to an adjacent well-defined midsagittal anatomic structure. A more detailed analysis of the dental midline is included below since many other factors must be considered.

Figure 1-8 A, Patient exhibiting facial asymmetry, including a deviating chin and vertical discrepancy in the eyes. B, Same patient showing a coincident dental midline in relation to the philtrum.
Finally, the chin is evaluated for any deviation in relation to the facial midline (Fig. 1-9, A). A view taken from above the patient (coronal) enhances the ability to detect any deviations (Fig. 1-9, B). Similarly, observing the patient from the lower (ventral) aspect of the mandible can complement this analysis (Fig. 1-9, C). This part of the clinical examination is very important, as a large chin deviation is an indication for further analysis, perhaps with additional radiographic imaging.

Figure 1-9 A, Patient with asymmetrical mandible. B, Coronal view to evaluate mandibular asymmetry during the clinical examination. C, Ventral view complements the assessment for mandibular asymmetry. In this patient the ventral view provides better information about the asymmetry. Arrows show the asymmetry between the left and right sides in the lip region.
Lips
A good analysis of the patient’s lips is done at rest position or with the upper and lower lips lightly touching (Fig. 1-10, A). Indications of any muscle strain on lip closure should be noted (Fig. 1-10, B). Upper and lower lip lengths can be assessed in the frontal and profile views. Upper lip length when noted alone is not as important per se as its relationship to the upper incisors at rest and when smiling. The proper relationship between the upper lip and the amount of upper teeth exposure is a key factor in modern esthetic smile construction (Fig. 1-11). Full display of the upper incisor crown upon smiling has been linked to youthful smiles.47 A differential diagnosis between a short or long lip and a maxillary vertical excess or deficiency is valuable in patients with an inadequate upper incisor display (Fig. 1-12).

Figure 1-10 A, Patient showing incompetent lips at rest. B, Upon lip contact the mentalis strain is noted.
Buccal Corridors and Smile Line
Other important relationships that can be evaluated only in the frontal view are the buccal corridors and the curvature of the smile line (relationship to lower lips). The buccal corridors and smile line concepts have been discussed extensively in the prosthetic literature.48 The ideal esthetic parameter in smile design in the transverse dimension has been related to wide dental arches and narrow buccal corridors (Fig. 1-13). Some authors have described upper first molar display on a full smile as a feature of an attractive smile.49 Although this does seem to be an attribute of beautiful smiles, its validity and applicability is doubtful. Anatomic structures limit the amount of transverse expansion needed to reduce the unattractive wide buccal corridors. The long-term periodontal health of teeth with expansion is not well understood. Computed tomography (CT) scans have shown that indiscriminate expansion of the maxillary arch results in buccal root dehiscences as these extend beyond the cortical plates.50 Another important reason to avoid indiscriminate expansion relates to long-term stability.51 Skeletal tissues (bones and teeth) are usually in equilibrium with the surrounding musculature; long-term stability might be compromised when teeth invade the neighboring muscle confinements.41,42

Figure 1-13 Esthetically pleasing smile. Patient exhibits the upper first molars with narrow buccal corridors and wide dental arches.
Another concept that has been related to esthetic smiles is the parallelism of the curve of the upper anterior teeth to the lower lip curvature on smiling (Fig. 1-14). Although this does seem to be an ideal objective, it should be noted that there are different types of smiles and the lower lip posture varies accordingly.52 Moreover, this smile arc is a result of the occlusal plane inclination and second-order crown angulations in the upper anterior teeth.53 Thus there are some limitations to achieving this ideal smile arc in every patient. A reasonable objective is to prevent a flat or reverse smile line (Fig. 1-15, A) and to obtain some degree of curvature that resembles the one found in the lower lip (Fig. 1-15, B).

Figure 1-14 Ideal parallelism between the incisal edges of the upper anterior teeth and the lower lip. The contact between the incisors and the lip is very slight.

Figure 1-15 A, Reverse relationship between the upper incisors and the lower lips, which is frequently found in patients with a finger habit. B, Correction of the reverse relationship after treatment. A better esthetic relationship to the lower lip was achieved.
Symmetry has always been linked to beauty. Not surprisingly, it has also been ascribed as one of the characteristics of a beautiful smile. This symmetry can be related to the size and shape of the teeth on both sides of each arch (see Fig. 1-11, A). Also, it is related to the relationship of the intraoral tissues to the lips on both the right and left sides. Therefore the same amount of gingival display should be seen upon smiling, on both sides of the arch. Reasons for any asymmetry include a cant in the maxillary skeletal base, different amounts of tooth eruption on the right and left sides, or asymmetrical smiles. It is estimated that 8.7% of normal adults have asymmetrical smiles (Fig. 1-16).54

Figure 1-16 Asymmetrical smile with more tooth structure display on the right side. A reverse smile curve is also evident.
The last feature related to symmetry in the smile is the dental midline. The ideal relationship of the dental midline to the facial midline was mentioned above. The upper dental midline has been considered more important than the lower dental midline in esthetic smile design. It has been shown that a discrepancy of <2 mm (to the right or left) between the upper dental midline and the facial midline is not readily perceived (Fig. 1-17, A).55,56 However, any type of unparallel relationship between the interproximal contacts of the incisors related to the facial midline (incisal cant) is more easily perceived (Fig. 1-17, B).57 Two further characteristics of an attractive smile are the gingival heights of the anterior teeth and the tooth shade. The gingival heights of the six upper anterior teeth are similar. The central incisors and the canines are at the same level, while the lateral incisors’ free gingival level is approximately 0.5 mm incisal to the level of the canines and central incisors (Fig. 1-18). Moreover, the gingival heights of the premolars and molars should be approximately 1 and 1.5 mm less than the canines, respectively (Fig. 1-19).58 The significance of tooth shade in the esthetic smile has been reviewed extensively in the prosthodontic literature.49 Light shades have always been considered one of the most important characteristics of an esthetic smile. Therefore procedures such as tooth bleaching may be considered after orthodontic appliance removal. Tooth shade also becomes an important factor in patients where canine substitution for missing upper laterals is considered. Differences in the tone between the canines (dark yellow) and incisors may be an indication to opt to restore the laterals prosthetically instead of closing the edentulous space (canine substitution).

Figure 1-17 A, Patient with upper midline deviated approximately 2 mm to the right of the facial midline. B, Patient with upper midline deviated approximately 1 mm from the facial midline. The inclination of the line described by the interproximal contact area accentuates the midline discrepancy.

Figure 1-18 Proper gingival heights. The upper central incisors and canines have the same gingival height; the lateral incisors’ gingiva is 1 mm below the canines and central incisors.

Figure 1-19 A, Gingival heights from the canines to the molars decrease gradually. B, Abrupt change in gingival heights between the canine and the second premolar. This situation is commonly seen in upper first premolar extraction.
The last notable factor in the ideal smile is tooth shape. Incisors are the predominant teeth in the smile, especially the upper central incisor. The ideal proportion of this tooth is found when the width approximates 75% to 80% of the height (Fig. 1-20).59 Similarly, lateral incisor size is often small in the mesiodistal dimension and should be considered in determining final occlusion and overall treatment outcome. Tooth shape is discussed further later in the chapter.
Profile View
Orthodontists spend more time evaluating patients from the profile view. Most of the literature is based on analysis from lateral cephalometric films. The classification of malocclusions is also based on the anteroposterior dimension (i.e., Angle classification). Even though the vertical dimension can be analyzed from this view, interest in this dimension has lagged. Later chapters describe the importance of the vertical dimension in the treatment of various malocclusions by an application of sound biomechanical principles.
Anteroposterior Dimension
The anteroposterior dimension is the backbone of most contemporary orthodontic analyses. In this dimension the soft tissue convexity is initially assessed by observing the spatial relationship between the forehead, maxilla, and mandible. These are separate but interrelated anatomic structures with independent timings in development. Each structure provides feedback to the others to maintain a normal facial growth pattern.60 Normally these three structures maintain a slight convexity that is reduced during puberty as a result of differential jaw growth.33 During the pubertal growth spurt the mandible has a greater anterior displacement compared to the maxilla. It is important to note that at the end of growth there are also gender differences in the convexity of the profiles. On average the female profile is more convex due to a smaller chin projection.61
Once the magnitude of the facial profile convexity is assessed, the next step is to evaluate which of the three structures is contributing to the abnormality. With an increased angle of convexity or concavity, the question to be answered is which structure is causing the deformity (mandible or maxilla). It has been reported that the majority of skeletal convexities exhibit a deficient mandible.62 On the other hand, studies show that approximately half of skeletal concavities present with a deficient maxilla.63
To evaluate maxillary and mandibular position during the clinical examination, an adequate reference plane must be determined. During the clinical examination the easiest assessment can be done using the natural head position. This can be achieved when the extraoral photographs are taken. More detailed analysis of the soft tissue spatial relationships in the anteroposterior dimensions is obtained from the lateral cephalograms.
Nose
Although the nose is outside the limits of what can be affected by orthodontic treatment, it is important for facial balance. More importantly, the apparent nose projection can be affected by the anteroposterior position of the lips. During the clinical examination, the length and height of the nose are evaluated. Any morphological variations in shape are noted (Fig. 1-21).

Figure 1-21 Patient with an abnormal nose contour.
Lips
Lip response to orthodontic treatment is one of the most discussed topics in modern orthodontics. With the increased interest in esthetics, patients and practitioners are interested in not only the dental and skeletal changes, but also the response of the surrounding soft tissues to treatment. As teeth move, there is a direct effect on lip support. Although this is a subject of perpetual research, no good predictor of t/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses







