Fractures of the zygomaticomaxillary complex (ZMC) are the second most common of all facial fractures. Multiple fixation methods have been used over the years, including wire osteosynthesis, lag screw fixation, transfacial Kirschner wire fixation, titanium plate and screw fixation, and more recently, resorbable plating systems. Internal fixation with titanium plates and screws provides the most rigid fixation and thus greater immobility of the fractured segments. The degree of immobilization created with titanium plates and screws also allows fixation at fewer anatomic points.
Conceptually, the approach to ZMC fractures should depend on the type and mechanism of injury. Low-energy injuries typically result in minimal or no comminution, whereas high-energy injuries can cause extensive comminution of the segments and at the fracture lines. Early non-comminuted and minimally displaced fractures may be managed by reduction alone if the reduction is thought to be stable. Older, displaced, and minimally comminuted ZMC fractures are managed by open reduction and proper orientation of the ZMC in three dimensions. Plate fixation is carried out at the zygomaticofrontal suture area, zygomaticomaxillary buttress, and inferior orbital rim. High-energy injuries can result in significant comminution at the fracture interfaces and fragmentation of the supporting bony buttresses. These fractures tend to be unstable and thus require a certain degree of bony reconstruction of the zygoma and its supporting buttresses, orbit, or zygomatic arch.
Regardless of the approach or fixation pattern chosen, it is critical to understand that proper alignment of the zygomaticosphenoid suture and anatomic reduction of the zygomatic arch remain the most reliable indicator of proper reduction and orientation of the ZMC in three dimensions.
This chapter discusses the anatomy of ZMC fractures, important signs and symptoms, contemporary approaches to common fracture patterns, postoperative care, and potential complications.
Anatomic Considerations and Fracture Patterns
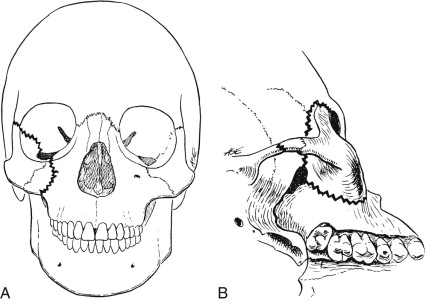
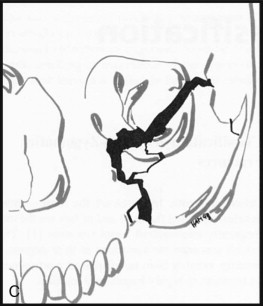
The zygoma is a quadrangular-shaped bone that provides lateral anterior projection of the central part of the face. The zygoma articulates with the frontal, temporal, maxillary, and sphenoid bones at the zygomaticofrontal, zygomaticotemporal, zygomaticomaxillary, and zygomaticosphenoid sutures ( Fig. 40-1, A and B ). These articulating sutures are areas of weakness and are therefore the most commonly fractured sites. The zygomaticosphenoid suture and zygomatic arch are the key anatomic landmarks. Their geometric arrangement and spatial relationship to each other and to the zygoma and the remainder of the facial skeleton are such that when they are aligned, the entire zygomatic complex should be anatomically aligned in three dimensions (see Fig. 40-1, A and B ). It is also important to understand that the zygoma forms major portions of the orbital floor and lateral wall. All zygomatic complex fractures therefore involve the orbit ( Fig. 40-1, C ). These areas are composed of thin bone and are consequently frequently fragmented and displaced. In fact, it has been estimated that ZMC fractures contribute to at least 76% of orbital fractures. Orbital floor or wall defects requiring bridging have been reported in up to 48% of ZMC fractures; however, there is certainly controversy on the severity of orbital floor disruption that would cause cosmetically apparent hypoglobus since anatomic reduction of the zygoma will frequently reduce the fractured orbital floor. Other areas of bony weakness are those containing a neurovascular bundle, such as the medial orbital rim at the level of the infraorbital foramen.
Sensory nerves associated with zygomatic complex fractures include the zygomatic, temporal, and facial branches of the second division of the trigeminal nerve as it passes through the body of the zygoma. The infraorbital nerve passes through the orbital floor and exits through the infraorbital foramen below the inferior orbital rim. Signs of nerve injury include paresthesia of the forehead, cheek, lateral part of the nose, upper lip, and anterior maxillary teeth. The infraorbital nerve is the most commonly affected, and it is has been estimated that approximately 95% of ZMC fractures involve the infraorbital canal and foramen. The reported incidence of post-traumatic, pretreatment infraorbital nerve sensory deficit ranges between 52% and 100%.
The position of the globe is largely due to the attachment of Lockwood’s suspensory ligament and the attachment of the lateral canthal tendon to the lateral orbital wall. Lockwood’s suspensory ligament largely determines the horizontal position of the globe and acts as a hammock to prevent inferior displacement of the globe in orbital blowout fractures. It attaches medially to the posterior aspect of the lacrimal bone and laterally to Whitnall’s tubercle. Whitnall’s tubercle is located within the lateral orbital rim 1 cm inferior to the zygomaticofrontal suture on the medial aspect of the frontal process of the maxilla. The lateral confluence of the orbicularis oculi muscle becomes the lateral canthal tendon, which attaches laterally to Whitnall’s tubercle and suspends the lateral aspect of the globe. The lateral canthal tendon attaches 2 mm superior to the medial canthal tendon, which produces a slight lateral cephalic slant of the globe.
Key anatomic landmarks for ZMC fracture repair include the anterior and posterior ethmoidal arteries, the superior orbital fissure, and the optic canal. The anterior and posterior ethmoidal arteries are located two thirds of the way up the medial orbital wall within the frontoethmoidal suture line. The anterior ethmoidal foramen is 20 to 25 mm posterior to the medial orbital wall. The posterior ethmoidal foramen is situated an additional 10 mm posterior to the anterior ethmoidal foramen. The superior orbital fissure is located 35 mm posterior to the zygomaticofrontal suture and 40 mm posterior to the supraorbital notch. The optic canal is 40 mm posterior to the infraorbital rim, 42 mm posterior to the anterior lacrimal crest, and 45 mm posterior to the supraorbital notch. Accepted safe dissection distances include 25 mm posterior to the inferior and lateral orbital rim and 30 mm posterior to the medial and superior orbital rims. This safe distance permits exploration and reconstruction of the orbit without damaging the contents of the optic canal or superior orbital fissure. However, it is important to remember that these safe distances are measured from intact orbital rims and that these measurements are not accurate in patients with significantly displaced or comminuted fractures.
Another important anatomic relationship for consideration when managing ZMC fractures is that of the temporal branch of the facial nerve. The temporal branch crosses the zygomatic arch approximately at its midpoint in a plane deep to the superficial temporal fascia and lateral to the periosteum. This important anatomic relationship is what dictates external approaches such as the Gillies approach and a coronal incision to access the zygomatic arch and outer orbital frame.
Clinical Examination
Patients who sustain facial trauma should be evaluated according to the advanced trauma life support protocol. Particular attention should be paid to concomitant maxillofacial injuries that may affect the airway, brain, and orbital contents. The examination is conducted with a cervical spine precaution protocol since the incidence of cervical spine injuries in patients with facial trauma has been reported to be as high as 3%. The examination should be detailed and systematic and should include evaluation of the cranial nerves, eyes, ears, and scalp. The face is then inspected and palpated for asymmetry caused by displaced fragments of the facial skeleton and for areas of edema, ecchymosis, and lacerations. Patients with non-displaced ZMC fractures may exhibit only soft tissue signs such as ecchymosis and edema overlying the fracture sites and conjunctival hemorrhage. Displaced fractures will generally cause ipsilateral facial flattening as a result of decreased anterior projection of the zygomatic body ( Fig. 40-2 ). The zygomatic arch may be intact, fractured and depressed, or bowed out. Laterally displaced zygomatic fractures are less frequently encountered, and the majority are due to blast injuries or severe blunt trauma to the central aspect of the face and result in pan-facial fractures. Displaced ZMC and isolated zygomatic arch factures may also cause trismus as a result of spasm of the masseter muscle or mechanical impingement of the coronoid process against the displaced fragments.
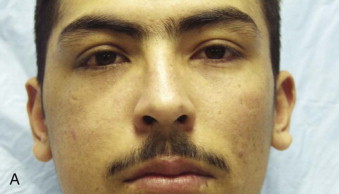

The appearance of the periorbital area is typically also affected in displaced fractures. This is seen as a deformity of the palpebral fissure caused by displacement of fragments containing the attachment of the eyelids and the lateral canthal tendon (see Fig. 40-2, A ). In fractures in which the orbital floor or orbital walls are displaced, the position of the globe is altered and it is usually seen as enophthalmos or hypoglobus. The globe typically becomes displaced posteriorly and inferiorly ( Fig. 40-3 ). In the acute setting this may not be appreciated because of edema of the orbital contents. Herniation or entrapment of the orbital contents into orbital floor defects, as well as soft tissue contusion and edema, may lead to restricted movement of the globe.

Evaluation of the extraocular muscles is performed by finger tracking. A forced duction test will generally differentiate between mechanical entrapment and restriction secondary to edema or contusion. If restricted range of motion is detected, topical anesthesia is applied to the sclera and the forced duction test is performed by grasping the insertion of the rectus muscles at two simultaneous points with two pairs of Adson forceps. The rectus muscles are grasped 7 mm from the limbus, and the globe is rotated in all directions. A positive forced duction test confirms soft tissue entrapment. A negative forced duction test with restricted extraocular movement indicates muscular hematoma or contusion or neurogenic causes of muscle paralysis.
An ophthalmology consultation should be considered if deemed necessary before surgical intervention and should include visual acuity and assessment of the status of the globe and retina, pupillary responses to light, visual field evaluation, and a funduscopic examination. Visual acuity examinations are performed with a Snellen chart at 20 feet or with a Near card at 16 inches from the patient. Patients with glasses for correction of visual astigmatism should wear their glasses during the examination if possible. The pupils are examined for anisocoria and for afferent and efferent pupillary responses with a swinging light test. Visual fields are assessed by standing directly in front of the patient and testing one eye at a time. The patient should stare directly ahead while the examiner tests peripheral gaze with finger motion and finger counting at the extremes of the patient’s visual fields. Extraocular muscle contusion or entrapment, as well as alteration in globe position, is commonly manifested as diplopia.
A funduscopic examination, if indicated, will assess for lens dislocation, vitreous hemorrhage, retinal detachment, and the presence of foreign bodies. Additional tests may include tonometry to indirectly measure intraocular pressure. Normal intraocular pressure is 10 to 20 mm Hg or symmetric readings. A slit-lamp examination will assess for irregularities in surface contour of the globe and cornea and can be used to rule out conjunctival chemosis, hemorrhage, foreign bodies, and hyphema. A cobalt blue light (Wood’s lamp) with fluorescein dye is used to detect corneal abrasions and lacerations. The fluorescein dye pools at the site of an abrasion/laceration, and the cobalt blue light illuminates the dye by converting it to a bright green color.
Finally, an oral examination is also conducted and may show ecchymosis and crepitation at the zygomaticomaxillary interface. Dental occlusion and the integrity of the palate should also be evaluated. It is not uncommon to have concomitant maxillary fractures. If they are missed or left untreated, appropriate reduction of the ZMC and restoration of bite will not be possible, which will lead to a poor outcome.
Clinical Examination
Patients who sustain facial trauma should be evaluated according to the advanced trauma life support protocol. Particular attention should be paid to concomitant maxillofacial injuries that may affect the airway, brain, and orbital contents. The examination is conducted with a cervical spine precaution protocol since the incidence of cervical spine injuries in patients with facial trauma has been reported to be as high as 3%. The examination should be detailed and systematic and should include evaluation of the cranial nerves, eyes, ears, and scalp. The face is then inspected and palpated for asymmetry caused by displaced fragments of the facial skeleton and for areas of edema, ecchymosis, and lacerations. Patients with non-displaced ZMC fractures may exhibit only soft tissue signs such as ecchymosis and edema overlying the fracture sites and conjunctival hemorrhage. Displaced fractures will generally cause ipsilateral facial flattening as a result of decreased anterior projection of the zygomatic body ( Fig. 40-2 ). The zygomatic arch may be intact, fractured and depressed, or bowed out. Laterally displaced zygomatic fractures are less frequently encountered, and the majority are due to blast injuries or severe blunt trauma to the central aspect of the face and result in pan-facial fractures. Displaced ZMC and isolated zygomatic arch factures may also cause trismus as a result of spasm of the masseter muscle or mechanical impingement of the coronoid process against the displaced fragments.

The appearance of the periorbital area is typically also affected in displaced fractures. This is seen as a deformity of the palpebral fissure caused by displacement of fragments containing the attachment of the eyelids and the lateral canthal tendon (see Fig. 40-2, A ). In fractures in which the orbital floor or orbital walls are displaced, the position of the globe is altered and it is usually seen as enophthalmos or hypoglobus. The globe typically becomes displaced posteriorly and inferiorly ( Fig. 40-3
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


