Introduction
White-spot lesions (WSL) are one of the most undesired side effects of multibracket appliance treatment (MB). The aim of this study was to investigate the incidence and further course of WSL during and after MB.
Methods
Four hundred patients (168 boys, 232 girls) meeting the inclusion criteria—all maxillary front teeth fully erupted and visible before treatment, no fillings or structural abnormalities, MB duration of at least 1 year, and retention period of at least 1 year—were selected. The patients’ average age was 13.7 years (SD, 3.5), and the average MB time was 1.9 years (SD, 3.6). All patients received standardized general prophylactic instructions. A modification of the WSL index was used to evaluate the 4 maxillary front teeth on introral photos before and after treatment, and after retention.
Results
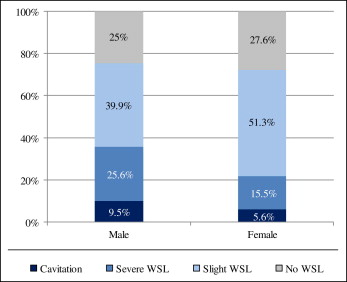
Before treatment, 32.3% of the patients had WSL. After MB, 73.5% of the patients presented WSL. The incidence of WSL during MB was 60.9% of the patients. After treatment, most patients (63.3%) had mild lesions, but the remaining were affected severely with (26.9%) and without (9.9%) cavitations. Only 26% of the patients were free of WSL all the time. After the retention phase, most (57.1%) of the WSL patients after treatment showed improvement, 26% remained unchanged, and 16.7% deteriorated. Male WSL patients tended to show more severe WSL than did the girls. There was a tendency for increased WSL development during the adolescent years compared with the preadolescent and postadolescent age groups.
Conclusions
With only standardized general prophylactic measures, new WSL developing on the maxillary front teeth during MB remain a frequent undesired side effect, affecting 60.9% of patients and counteracting our efforts for clinical excellence.
White-spot lesions (WSL) are among the most undesired side effects of multibracket appliance treatment (MB) and have been reported to occur in 2% to 96% of these patients. Patients receiving MB are significantly more susceptible to the development of WSL than untreated patients, because the presence of brackets, bands, and archwires impairs oral-hygiene measures and increases plaque-retention sites. As a result of increased plaque accumulation, the level of caries-inducing bacteria in the oral cavity is elevated. The consequently lower pH of the retained plaque on the enamel surface adjacent to orthodontic brackets hinders the remineralization process; thus, decalcification can occur. Such initial enamel decalcifications can be seen as early as 4 weeks after the beginning of MB.
Many prophylactic measures have been introduced in the last decades aiming at prevention of WSL during MB. Among the most common and effective preventive measures are special oral-hygiene instructions including a recommendation for the use of high-fluoride toothpaste, fluoride mouth rinse, and products with a high-fluoride content. However, although it is generally accepted that fluoride reduces the rate of demineralization, fluoride treatment might have a limited effect on the bacterially produced lower pH conditions in MB patients. This is possibly why only a demineralization-inhibiting tendency with daily use of a fluoride rinse during MB could be shown. Unfortunately, additional specific preventive orthodontic efforts such as fluoride-releasing bonding materials seem to have minimal or no positive effect.
As a result of the disappointing results from Pancherz and Mühlich and in line with the positive findings in the literature, standardized fluoride prophylactic procedures were adopted for all MB patients at our department starting in 1996. Because it is unclear how much these general prophylactic measures decrease the WSL under normal clinical (nonstudy) conditions in contrast to specific study conditions, we aimed to assess the prevalence, incidence, and post-MB course of WSL in these patients under standard instructive and general fluoride prophylactic measures retrospectively.
Material and methods
Ethics approval (112/09) was granted by the Ethical Committee of the medical faculty of the Justus-Liebig-University of Giessen in Germany. The treatment records of all patients that had completed MB between 1996 and 2006 in the Department of Orthodontics were retrospectively screened for inclusion.
The following inclusion criteria were applied: (1) no previous MB; (2) all 4 permanent upper front teeth (UFT, any tooth in this area) fully erupted and fully visible before treatment; (3) no dental structural abnormalities or frontal fillings, veneers, or other reconstructions on the 4 UFT either before or after treatment; (4) at least 4 brackets bonded to the UFT; (5) MB for more than 1 year; (6) retention period at least 1 year; (7) full documentation (treatment charts, intraoral slides) available before treatment (T0), after MB (T1), and after retention (T2); (8) T0 slides less than 1 year old (mean, 0.36 years; SD, 0.26); and (9) T1 slides taken directly after or at the latest within a week of bracket debonding (mean, 0.32 days; SD, 0.56)
At the start of MB, all patients received general oral-hygiene instructions and special MB cleaning instructions (use of toothbrush and interdental brush after meals 2-3 times daily) including recommendations for daily use of fluoride toothpaste and fluoride mouth rinse, and weekly use of products with a high-fluoride content (Elmex gel, GABA International, Therwil, Switzerland).
The first 400 (168 boys, 232 girls) patients (1600 UFT) meeting the study criteria were included. Their average ages were 13.7 years (SD, 3.5) at T0, 15.7 years (SD, 3.6) at T1, and 17.7 years (SD, 3.6) at T2. Active treatment time was an average of 1.9 years (SD, 0.76) with an upper limit of 7.5 years; average retention time was 2 years with a maximum of 6.1 years. Based on the patients’ ages at T0, 3 age groups were formed: less than 12 years, 12 to 16 years, and more than 16 years.
All evaluated intraoral slides had been taken by the same photographer using a standardized technique with a camera (OM-4 Ti, Olympus, Tokyo, Japan) with a Macro Objective lens (80 mm, Olympus) supplied with a ring flash (T 10, Olympus) and Ektachrome Pro color reversal film (Kodak, Rochester, NY). Three standardized intraoral slides (frontal, left and right lateral views) that had been taken at each of the 3 treatment time points (T0, T1, T2) were evaluated. Visual assessment was done by using 2 Ektapro 500 slide projectors (Kodak) with a projection size of 1.1 × 1.6 m per image. In each evaluation step, 2 time points (T0 and T1; T1 and T2) were projected and evaluated simultaneously.
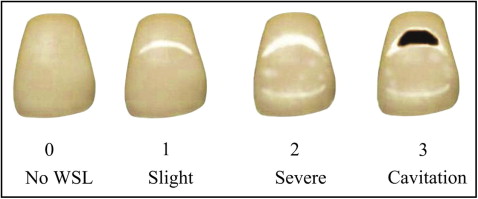
The modified WSL index of Gorelick et al was used to evaluate the labial surface of the 4 UFT at T0 and T1. The patients were divided into 4 groups depending on the highest WSL score that could be assessed from any of the 4 UFT: 1, no WSL; 2, slight WSL; 3, severe WSL; and 4, cavitation ( Fig 1 ). The further course of WSL during the retention period (T1-T2) was assessed by using a modified WSL-change index as described by Pancherz and Mühlich. The visual evaluation of the individual teeth was based on a labial surface comparison between the time points. The following scores were given: 0, no WSL at any time during treatment; +, improved WSL; =, unchanged WSL; and –, worsened WSL. Gingival inflammation in the UFT region was assessed at T0 and T2. The following scores were given: 0, no gingival inflammation (no redness or swelling) and 1, gingival inflammation (redness and swelling).
The records of the first 10 patients were evaluated simultaneously but independently by the 3 previously calibrated observers (M.E., N.B., S.F.). One week later, the same 3 observers evaluated the same 10 patients again.
Intraobserver reliability was assessed by using the Fleiss kappa test. For the first observer (the study observer, who conducted the whole study evaluations), the T0 and T1 WSL scores showed agreement of 95.1% between sessions and agreement of 92.7% for the T2 scores. For the second observer (orthodontist with >15 years of experience), the T0 and T1 WSL scores showed intersession agreement of 92.2% and agreement of 83.5% for the T2 scores. For the third observer (orthodontist with <5 years of experience), the T0 and T1 WSL scores showed intersession agreement of 70.2% and agreement of 47.5% for the T2 scores.
The interobserver reliability was assessed by means of a nonparametric test (Kendall coefficient of concordance). At the first evaluation session, the WSL scores of the 3 observers showed agreement values of 75.3% for T0, 83.1% for T1, and 80.1% for T2. At the second evaluation session, the WSL score agreement values were 78.4% for T0 and 82% for both T1 and T2.
Statistical analysis
The entry of the collected data into the computer was controlled twice to optimize the data-entry accuracy. The statistical evaluation was performed in cooperation with the Institute for Medical Informatics of the Justus-Liebig-University of Giessen by using software (version 9, SAS, Cary, NC). In addition to normal descriptive statistics, the Fisher exact test was used to assess possible sex and age-group differences in WSL prevalence at T0 and T1. Cochran-Mantel-Haenszel statistics were applied to test whether any of the 4 UFT had a higher tendency for WSL at T0 or T1. Furthermore, the sign test was used to assess possible sex and tooth differences for the T2 changes.
Results
At T0, 271 (108 boys, 163 girls) patients (67.7%) were free of WSL, and 129 (60 boys, 69 girls) patients (32.3%) showed WSL with various degrees of severity ( Fig 2 ). Most of the 129 WSL patients (86.8%) had mild lesions, and the remaining WSL patients were affected severely, either without (9.3%) or with (3.9%) cavitations. There were no differences between the sexes ( P = 0.286) or age groups ( P = 0.8923). Forty-five percent of the WSL patients showed signs of gingivitis, whereas 55% did not. In contrast, of the WSL-free patients, 34% exhibited gingivitis before treatment, and 66% had healthy gingiva. Among the 1600 UFT that were evaluated ( Fig 2 ), 1285 teeth (80.3%) exhibited no signs of WSL, and 315 teeth (19.7%) had varying severities of WSL. There was no relevant tendency ( P = 0.1541) of any of the 4 UFT to exhibit more WSL.
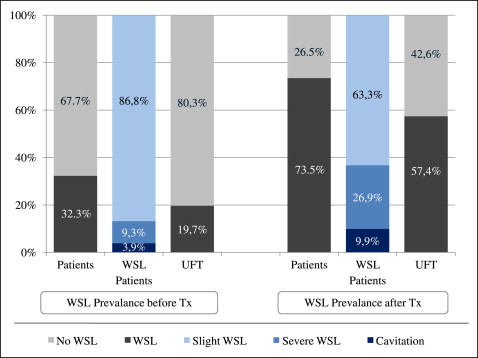
At T1, 106 (42 boys, 64 girls) patients (26.5%) were free of WSL, and 294 (126 boys, 168 boys) patients (73.5%) had varying severities of WSL ( Fig 2 ). There was no difference in average active treatment length between the WSL and the WSL-free patients (1.9 years; SD, 0.8 for both groups). There was a mild tendency ( P = 0.0663) for the 12-to-16 age group (44.5%) to have more WSL compared both the younger (19.2%) and older (6.8%) groups. Almost two thirds (63.3%) of the WSL patients had mild lesions, whereas the remaining WSL patients were affected severely, either without (26.9%) or with (9.9%) cavitations at T1. The boys tended ( P = 0.0182) to have a higher percentage of severe WSL either with or without cavitations (35.1%) compared with the girls (21.1%) ( Fig 3 ).
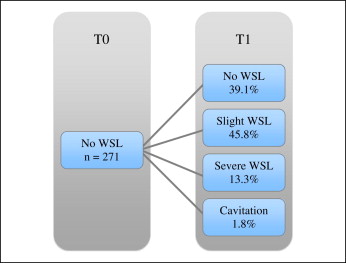
When we analyzed explicitly the 271 patients who were WSL-free at T0, 39.1% remained WSL-free at T1, whereas 45.8% showed slight WSL ( Fig 4 ). The remaining patients were affected severely either without (13.3%) or with (1.8%) cavitations. The incidence rate for WSL (T1-T0) was 60.9 % of the patients. Furthermore, it was noticed that the WSL-free patients at T1 tended to show less gingivitis at T0 (16%) than the WSL patients (49%). Six hundred eighty-one (42.6%) of the 1600 UFT evaluated were WSL-free, and 919 teeth (57.4%) had WSL of different severities. There was no relevant tendency of any of the 4 UFT to exhibit more WSL. There was, however, a tendency for the maxillary lateral incisors ( P = 0.0209) to have more severe WSL either with or without cavitations.
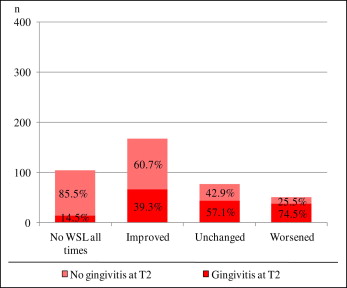
At T2, the average retention time of the patients was 2 years (SD, 0.72). Throughout the entire observation period, only 104 (26%) patients remained entirely WSL-free. Patients who were WSL-free at T1 had a great probability (98%) to remain WSL-free at T2. There were no differences with respect to active treatment or retention times between the WSL-free patients and the other WSL-change groups. Of the 294 patients who exhibited WSL of different severities at T1, 57.1% showed improvement, 26% remained unchanged, and 16.7% deteriorated. Girls tended to show slightly more improvement (46.1% vs 36.3%) compared with boys, who had more unchanged (23.8% vs 15.9%) or worsened (15.5% vs 10.8%) WSL.
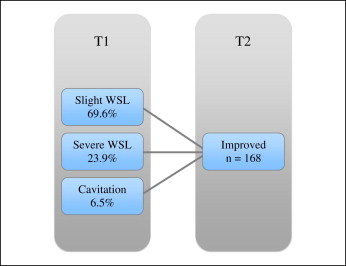
Patients exhibiting WSL improvement had, in descending order, slight WSL at T1 (69.6%), severe WSL without cavitations (23.9%), and severe WSL with cavitations (6.5%) ( Fig 5 ). There was a clear trend ( Fig 6 ) for a higher prevalence of gingivitis at T2 in patients exhibiting deterioration of their lesions (74.5%) compared with patients who were WSL-free at all times (14.5%). No relevant tendency could be seen of any of the 4 UFT for a higher percentage of WSL changes. However, there was a clear tendency for girls to have more improved tooth lesions than boys ( P <0.001).