Teledentistry is an exciting new area of dentistry that fuses electronic health records, telecommunications technology, digital imaging, and the Internet to link health providers in rural or remote communities. For the patient located in underserved or remote areas, teledentistry improves ready access to preventive dental care and teleconsultation with specialists. It allows the dentist in the nearby community to provide easier access to preventive care to a patient who, otherwise, probably will not seek care. It enables the specialist located many miles away to make a diagnosis and recommend treatment options and/or referral.
Advances in dental care have documented that early diagnosis, preventive treatments, and early intervention can prevent or reduce the progress of most oral diseases, conditions that, when left untreated, can have painful, disfiguring, and lasting negative health consequences. Unfortunately, millions of American children and adults lack regular access to routine dental care, and many of them suffer needlessly with disease that inevitably results in significant decrements in their quality of life. Problems in access to oral health care cut across economic, geographic, and ethnographic lines. Racial and ethnic minorities, people who have disabilities, and those from low-income families, particularly children, are especially hard hit. In most rural areas in this country, especially, there are many barriers to dental health care, including geographic remoteness, sparse population, adverse seasonal weather and road conditions, poor or no public transportation, poverty and lack of health insurance, a less mobile aging population, culturally specific health care needs of many groups (especially American Indian and immigrant populations); a low number of dentists relative to total population, and a scarcity of specialty and subspecialty dentists.
Teledentistry is an exciting new area of dentistry that uses electronic health records, telecommunications technology, digital imaging, and the Internet to link health care providers in rural or remote communities to enhance communication, the exchange of health information, and access to care for underserved patients. This article discusses how innovative health information and communication technologies can improve access to oral health care through teledentistry.
What is teledentistry and how does it work?
Teledentistry uses electronic health records, telecommunications technology, digital imaging, and the Internet to provide teleconsultation with specialists, supervision of collaborative hygienists in remote areas, and education. Teleconsultation can take on two forms. Real-time consultation uses direct on-line computer video telecommunication between a dentist, hygienist, or patient in a remote community and a dentist or specialist in a larger community who provides support or supervision. In the “store and forward” method, electronic health records and videos store data that can be retrieved and reviewed by the specialist who renders an opinion ( Figs. 1 and 2 ).

Telehealth projects, including telemedicine and teledentistry, have been implemented as models to improve education and access to care. Telehealth has been used in various demonstration projects throughout the nation and has been shown to be particularly helpful in remote and rural areas where access to specialists is limited. For example, Total Dental Access is the teledentistry project within the Department of Defense that enables referring dentists from the US Armed Forces to consult with specialists at a medical center on the status of a patient. Total Dental Access focuses on three areas of dentistry: patient care, continuing education, and dentist–laboratory communications. This project has demonstrated increased patient access to dental care and the cost effectiveness of a Web-based system. The Children’s Hospital Los Angeles Teledentistry Project, developed in association with the University of Southern California’s Mobile Dental Clinic, increases and enhances the quality of oral health care provided to children living in remote rural areas of California, areas often severely underserved by dental health providers. A 12-month trial of teledentistry was conducted in two general dental practices in remote sites in Scotland. The dental practices had a personal computer (PC)-based videoconferencing link connected by an Integrated Services Digital Network (ISDN) at 128 kbit/s to a restorative specialist at a central hospital. Twenty-five patients were recruited into the trial. A cost-minimization analysis was undertaken by comparing the costs of teledentistry with two alternatives: outreach visits, in which the specialist regularly visited the remote communities, and hospital visits, where patients in remote communities traveled to hospital for consultation. The study found the cost savings of teledentistry were greatest in the remote communities, where patients otherwise would have had to travel long distances for specialist consultations.
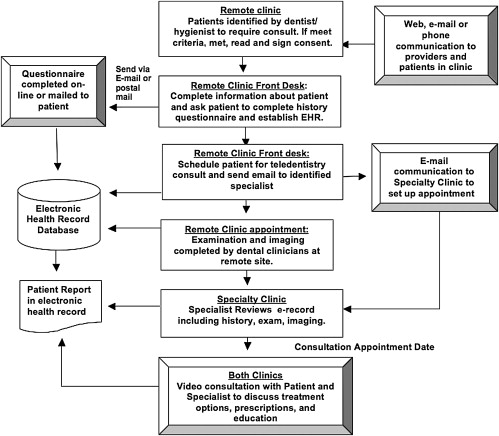
For a typical teledentistry visit, special videoconference equipment and a video/Internet connection are set up at both the hub site and the remote site. The patient checks in at the remote clinic and before the consultation fills out questionnaires, either on paper or on line, regarding chief complaints and medical and dental history. The dentist or a member of the dental team (assistant or hygienist) at the remote clinic facilitates and records a hands-on examination (see Fig. 2 ). (This examination may take place either during the visit or earlier, when a teleconsultation is requested.) The questionnaire, examination, and any imaging or documents that are included in the dental record are transmitted to the hub (eg, to a university specialist) via the online electronic patient record system. With this information in hand and reviewed, the specialist starts a live consultation with the patient through videoconferencing ( Fig. 3 ).
The live video-consultation is similar to a live in-person consultation (see Fig. 1 ). The dentist interviews the patient, asks questions, discusses the diagnosis and treatment, and educates the patient about the condition. In some situations, the dentists may ask the patient to open the mouth to determine function or measure the opening in front of the camera. In other cases, the dentist reviews the images and examination findings presented in the electronic record on a split screen with the teleconsultation and reviews this information with the patient. In all cases, patients need to feel connected to the dentist performing the consultation, as if the dentist were standing next to the patient.
A major challenge in a teledentistry visit is the collaboration between the hub site and the remote site. Fig. 3 illustrates the process for communicating between the remote site and the specialist clinic site. Because the consultation is “remote” in nature, the dental teams at both sites must collaborate constantly for a smooth teledentistry process. The challenge begins with making the concurrent appointment at both sites, progresses through the collection of patient information and its transmittal to the specialist, facilitating the “remote” real-time examination, and ends with facilitating the plan for treatment and future care. Because the specialist cannot perform a hands-on examination, he/she must rely on the examination performed by the dental team at the remote site. Confidence and good working relationships between team members at both sites must be established. As in any other learning processes, appropriate training, practice, and patience are essential for a satisfactory result. With hands-on training and repeated practice, the dental teams at both sites can establish a reliable network for teledentistry.
The University of Minnesota teledentistry project
A teledentistry network has been established that links specialists at the University of Minnesota School of Dentistry to dentists and patients in remote rural areas where access to care is difficult. The network also increases training for dentists and dental students in the rural community in the management of orofacial disorders. Minnesota traditionally has been a state with a high level of awareness regarding dental and health matters and ranks above the national average in access to health care. There are, however, special populations and several geographic areas in the state where the picture is not so bright and where barriers to quality dental care are many, including geographic remoteness and sparse population. Teledentistry has improved this situation by expanding the access of rural and underserved populations to care through electronic communication.
The teledentistry network was established in 2004 linking the University of Minnesota School of Dentistry specialists with dentists and patients in remote rural areas. The first demonstration site was implemented at the Hibbing Community College Dental Clinic. This clinic is located approximately 200 miles north of Minneapolis and is a joint venture with the Hibbing Community College. The patient population consists primarily of low-income families in St. Louis, Lake, Cook, and Carlton Counties. The clinic is staffed by dental students with supervision from faculty to provide clinical training in rural areas of Minnesota. In their junior and senior years, all dental students rotate through this clinic; at any given time, four to six students provide care to the patient population. This clinic provides care for patients who have medical assistance from states and Medicaid.
Currently, the teledentistry system provides consultations to the demonstration site for temporomandibular disorder, orofacial pain, and oral medicine. The preliminary testing and evaluation of the system revealed high levels of acceptance and satisfaction from both providers and patients. In more than 90% of the visits, specialists were satisfied with the teledentistry consultation. In 94% of the visits, providers were as confident about providing adequate diagnosis and treatment planning as in a face-to-face visit. In 83% of the cases, providers thought that patient assessment using teledentistry was as complete as in a regular visit.
One challenge in a teledentistry visit is the possible increased time needed to perform a consultation. In the majority of the visits (61%), providers reported using about the same amount of time as in a regular in-office visit, but in 33% of the visits providers thought that teledentistry visits were more time-consuming. This problem is encountered particularly when the providers are learning to use the system. With experience, skills improve, and work is performed more efficiently.
Patients expressed high levels of satisfaction with the teledentistry service. The greatest benefits that the teledentistry network offers patients are convenience and access to care. Since the program started, approximately 13 patients have made 24 teledentistry visits through the course of their care. The patient satisfaction study showed that, instead of driving 200 to 300 miles each way to the University for care, the average distance for visiting the teledentistry clinic is only 13 miles. On average, a teledentistry visit requires less than 2 hours, compared with 18 hours if the patient had to travel to Minneapolis for the visit ( Table 1 ). Specialists who can treat orofacial disorders such as temporomandibular disorder, orofacial pain, and oral medicine rarely are found in local rural communities. These disorders usually are chronic conditions that require repetitive visits and ongoing care. Many patients commented on the teledentistry service as being “convenient,” “effective,” “saving on travel time,” requiring “less time out of [the patient’s]schedule,” and being “easier to reach.”
| Distance Traveled and Time Spent by Patient | Teledentistry Clinic | University of Minnesota School of Dentistry Specialty Clinic |
|---|---|---|
| Travel distance to clinic (average, one-way, in miles) | 12.6 | 230.3 |
| Time missing from work/school (average, in hours) | 1.6 | 18.3 |
In addition to providing greater convenience in accessing care, teledentistry also effectively meets patients’ goals in seeking care. The average rating of teledentistry in meeting a patient’s goal for a visit is 9.1 (with 10 being the best possible). The patients’ overall satisfaction that the teledentistry clinic met their current health care needs was rated as 6.84 on average (with 1 = not satisfied at all and 7 = completely satisfied). When considering their experience with teledentistry visits, most patients felt comfortable in visiting the doctor through the videoconference service. In fact, many patients felt that the teledentistry visit was “the same as in an office or in person,” except that it was “just through the TV.” When patients were asked if they would prefer to see the doctor in person, half of the participants said “no” because they perceived no need for doing so. Some patients felt that seeing the doctor in person “would always be the best” but “this [teledentistry] works well, too.”
Many patients who used the teledentistry service expressed their appreciation for and satisfaction with the program. Patients commented that teledentistry is a “wonderful service to provide to patients of rural areas … to give the knowledge and expert advice of the specialists via teledentistry is such a convenience”; “thank you for giving us big city help in a rural area”; “I feel that many people would benefit from this kind of dentistry if it was available”; “I love this system. It has made getting care easier and more convenient.” As a result, all participants said they would use the teledentistry service again. Some patients recommended the service to their relatives and friends.
The University of Minnesota teledentistry project
A teledentistry network has been established that links specialists at the University of Minnesota School of Dentistry to dentists and patients in remote rural areas where access to care is difficult. The network also increases training for dentists and dental students in the rural community in the management of orofacial disorders. Minnesota traditionally has been a state with a high level of awareness regarding dental and health matters and ranks above the national average in access to health care. There are, however, special populations and several geographic areas in the state where the picture is not so bright and where barriers to quality dental care are many, including geographic remoteness and sparse population. Teledentistry has improved this situation by expanding the access of rural and underserved populations to care through electronic communication.
The teledentistry network was established in 2004 linking the University of Minnesota School of Dentistry specialists with dentists and patients in remote rural areas. The first demonstration site was implemented at the Hibbing Community College Dental Clinic. This clinic is located approximately 200 miles north of Minneapolis and is a joint venture with the Hibbing Community College. The patient population consists primarily of low-income families in St. Louis, Lake, Cook, and Carlton Counties. The clinic is staffed by dental students with supervision from faculty to provide clinical training in rural areas of Minnesota. In their junior and senior years, all dental students rotate through this clinic; at any given time, four to six students provide care to the patient population. This clinic provides care for patients who have medical assistance from states and Medicaid.
Currently, the teledentistry system provides consultations to the demonstration site for temporomandibular disorder, orofacial pain, and oral medicine. The preliminary testing and evaluation of the system revealed high levels of acceptance and satisfaction from both providers and patients. In more than 90% of the visits, specialists were satisfied with the teledentistry consultation. In 94% of the visits, providers were as confident about providing adequate diagnosis and treatment planning as in a face-to-face visit. In 83% of the cases, providers thought that patient assessment using teledentistry was as complete as in a regular visit.
One challenge in a teledentistry visit is the possible increased time needed to perform a consultation. In the majority of the visits (61%), providers reported using about the same amount of time as in a regular in-office visit, but in 33% of the visits providers thought that teledentistry visits were more time-consuming. This problem is encountered particularly when the providers are learning to use the system. With experience, skills improve, and work is performed more efficiently.
Patients expressed high levels of satisfaction with the teledentistry service. The greatest benefits that the teledentistry network offers patients are convenience and access to care. Since the program started, approximately 13 patients have made 24 teledentistry visits through the course of their care. The patient satisfaction study showed that, instead of driving 200 to 300 miles each way to the University for care, the average distance for visiting the teledentistry clinic is only 13 miles. On average, a teledentistry visit requires less than 2 hours, compared with 18 hours if the patient had to travel to Minneapolis for the visit ( Table 1 ). Specialists who can treat orofacial disorders such as temporomandibular disorder, orofacial pain, and oral medicine rarely are found in local rural communities. These disorders usually are chronic conditions that require repetitive visits and ongoing care. Many patients commented on the teledentistry service as being “convenient,” “effective,” “saving on travel time,” requiring “less time out of [the patient’s]schedule,” and being “easier to reach.”



