Oral health is associated with overall health, and lack of access to dental care has consequences that go far beyond aesthetics. Most oral diseases are preventable and are relatively easy and inexpensive to address at early stages. However, multiple barriers make dental care unreachable for a sizable portion of the United States population, who consequently has higher incidence and prevalence of disease. Achieving meaningful improvements in oral health status among these groups will require a revamping of the dental infrastructure, augmenting the productivity and skills of the dental workforce, and increasing the population’s oral health literacy.
Relevance of oral health
Connection With General Health
Oral health is important to an individual’s well-being and overall health. Therefore oral health must be considered in the context of the individual’s environmental, behavioral, and socio-cultural factors. Poor oral health can have social, economic, behavioral, and quality-of-life effects.
Various studies have reported associations between oral health and systemic conditions. Studies assessing the link between coronary heart disease and periodontal diseases found that different presentations of periodontal diseases (gingivitis, tooth loss, periodontitis, and bone loss) were independent risk factors for coronary heart disease. Moreover, it has been demonstrated that intensive treatment of periodontal disease resulted in improved endothelial function, which is a pathway to acute cardiovascular events. The association between oral health and diabetes has been recognized for many years. This association goes both ways: diabetes, particularly uncontrolled diabetes, is a risk factor for periodontal diseases. The presence of periodontal diseases among diabetics is so frequent that periodontal diseases have been considered the sixth highest ranked complication of diabetes. On the other hand, there is strong evidence that periodontal diseases hinder diabetes control. An association between chronic kidney disease and total tooth loss or edentulism also has been reported. In this study, chronic kidney disease was more common among persons who had antibodies against the bacteria that cause periodontal diseases, but the investigators did not find any association between chronic kidney disease and clinical periodontal disease. Studies have reported an association between poor maternal oral health status, particularly periodontal diseases, and preterm and low birth weight babies. It is not clear if this association is causal ; however, the association is sufficiently strong that recommending periodontal checkups before and during pregnancy is warranted.
Among older adults, bacteria from the mouth can be aspirated during sleep and reach the lungs. Consequently, older persons who have poor oral health (caries lesions, periodontal diseases, and plaque) are more likely to present with pneumonia than older persons who have good oral health. It also has been shown that respiratory diseases among older persons living in nursing homes and in ICUs can be prevented or limited with good oral hygiene.
Quality of Life
Quality of life can be affected severely by conditions and diseases related to oral health. Poor oral health negatively affects a person’s self-esteem, self-image, and overall well-being. People who are embarrassed or self-conscious about their oral health frequently avoid showing their teeth, so that basic non-verbal expressions such as smiling, talking, and laughing are compromised; the absence of these non-verbal cues hampers social interactions.
Functional problems of the oral cavity (eg, loss of teeth) also affect quality of life by causing difficulties eating. Masticatory efficiency is reduced as teeth are lost or replaced by total or partial dentures. Difficulties in chewing determine the frequency and types of food consumed.
Oral-facial pain also can affect quality of life. Acute pain associated with dental caries or periodontal diseases can be treated easily by a dentist. Most chronic pains related to the mouth are difficult to diagnose, however, and in many cases the cause cannot be identified or removed. In these cases, the treatment is limited to pain management.
The problem
The natural history of oral diseases is well understood. Most oral diseases are neither self-limiting nor self-repairing. For example, in the case of dental caries, the decaying process can continue until the destruction of the tooth and the compromise of adjacent tissues. The intervention of a dental professional at any stage of disease may help stop the disease and/or reduce its impact. With few exceptions, maintenance of oral health over a person’s lifespan requires the participation of oral health professionals, and in many cases professional care is needed even before the disease process starts. Prompt professional care is fundamental, given that oral diseases follow a downward spiral: incipient diseases requiring minimum dental care, if untreated, progress into diseases that require increasingly more complex and expensive treatments; increases in complexity and cost usually make the treatment even more out of reach for a large proportion of the population.
Consequences of poor oral health carry over a lifespan. Caries among children predict oral health problems among adults; current caries is the best predictor of future caries. The United States population, however, does not receive the adequate dental care needed to preserve oral health. In 1958, Drs. Levell and Clark reported, “despite the relative high number of well-qualified practicing dentists in this country and despite their highly developed means for restoring lost tooth structure, less than one-third of the dental needs of the country are given attention.” Unfortunately, for the socially disadvantaged sectors of the population, the situation has not changed much since then.
The problem
The natural history of oral diseases is well understood. Most oral diseases are neither self-limiting nor self-repairing. For example, in the case of dental caries, the decaying process can continue until the destruction of the tooth and the compromise of adjacent tissues. The intervention of a dental professional at any stage of disease may help stop the disease and/or reduce its impact. With few exceptions, maintenance of oral health over a person’s lifespan requires the participation of oral health professionals, and in many cases professional care is needed even before the disease process starts. Prompt professional care is fundamental, given that oral diseases follow a downward spiral: incipient diseases requiring minimum dental care, if untreated, progress into diseases that require increasingly more complex and expensive treatments; increases in complexity and cost usually make the treatment even more out of reach for a large proportion of the population.
Consequences of poor oral health carry over a lifespan. Caries among children predict oral health problems among adults; current caries is the best predictor of future caries. The United States population, however, does not receive the adequate dental care needed to preserve oral health. In 1958, Drs. Levell and Clark reported, “despite the relative high number of well-qualified practicing dentists in this country and despite their highly developed means for restoring lost tooth structure, less than one-third of the dental needs of the country are given attention.” Unfortunately, for the socially disadvantaged sectors of the population, the situation has not changed much since then.
Overview of the most common oral diseases
This section presents the most common oral diseases, their epidemiology, and their distribution and highlights potential interventions from the perspective of the levels of prevention. In 1953, Clark and Leavell introduced the levels of prevention, and since then their model has been used widely. Although their model is illness oriented because it is based on the natural history of disease, it provides clear indication of the opportunities for prevention at each stage of disease. The model posits that treatment is one form of prevention that occurs after the disease process has started. Treatment is preventative in that it averts more serious damage.
Primary Prevention
Primary prevention seeks to thwart the start of the disease process. It includes measures that promote general health and more specific measures against the agents or circumstances associated with the disease in consideration. Primary prevention includes health promotion and specific protection.
Activities included in health promotion foster health in general and are applicable to any disease. They include health education, good nutrition, adequate housing, recreation, and agreeable working conditions. These activities for primary prevention have not changed significantly since Leavell and Clark described them in their model of the levels of prevention. Currently, one would add an adequate environment free of pollutants and opportunities for physical exercise. All persons should have the opportunity to engage in adequate primary prevention activities. Leavell and Clark indicated that the engaging in activities that promote health empower the individual to obtain the highest levels of health on his/her own.
Specific protection refers to measures that protect against specific disease agents, usually by establishing barriers against those agents. Therefore, specific protection intercepts the disease process before it starts. Community activities in oral health focus on specific protection.
Secondary Prevention
Secondary prevention takes place after the disease process has started, seeking to avoid the spread of diseases, to cure or arrest diseases, and to lessen disability. Secondary prevention includes early diagnosis, prompt treatment, and limiting disability. An individual’s ability to act on this level of prevention depends on the availability and accessibility of dental care. Persons receiving limited or no dental care at this stage are destined to worse oral health outcomes and more expensive treatment.
Tertiary Prevention
The tertiary level of prevention refers to rehabilitation or the prevention of total disability after the disease has ran its course. If untreated, the most common oral health diseases (caries and periodontitis) are likely to result in tooth loss. Depending on the tooth or teeth that are lost, functionality and esthetics may be affected severely. Restoration of function and esthetics occurs with tooth replacement.
Caries
Caries is an infectious disease caused by bacteria that reside in the dental plaque. Streptococcus mutans is the most cariogenic bacteria because of its ability to produce acid. If early caries prevention measures, such as plaque removal, fluoride, and sealants, are not in place, the acid demineralizes the tooth surface, appearing initially as white spots. At this early stage, the caries process can be reversed by remineralizing the enamel with fluoride varnish. Otherwise, the white spots may progress until they result in a cavity, which if untreated may extend to other tooth structures such as the dentin or the tooth’s pulp.
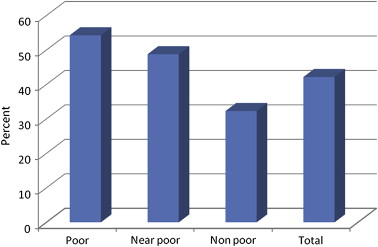
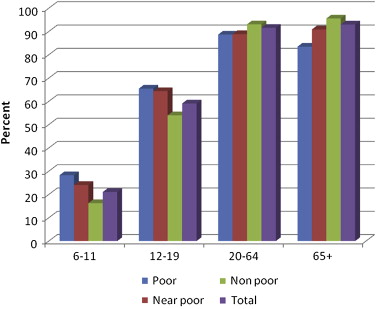
Dental caries is a highly prevalent disease. Among children in the United States, caries is five times more frequent than asthma, and 95% of adults have had dental decay in their permanent teeth. Dental caries are more common among the socially disadvantaged: the poor and racial ethnic minorities ( Figs. 1 and 2 ).
Primary prevention
General promotion
A good diet is particularly important for the prevention of caries. Fermentable carbohydrates, which include sugars and cooked starches, are the most cariogenic foods. Caries develops more easily when these sugars and starches are consumed between meals. For example, feeding infants juice between meals has been associated with dental caries. The consumption of milk, on the other hand, has been found not to be associated with caries. A visit to the dentist during a baby’s first year will give the opportunity for caregivers to discuss and learn about health, diet, and behaviors conducive to good oral health.
Specific protection
Effective preventive agents are available to prevent caries. Community water fluoridation is arguably the most cost-effective of all measures. Water fluoridation provides fluoride to all persons residing in the water system catchment area, regardless of socioeconomic condition, at a very low cost. Fluoride in toothpaste is another effective mechanism to prevent caries. In fact, fluoridated toothpaste has been considered responsible for the global decline in caries in the late twentieth century. Dental sealants also provide significant caries prevention. Sealants are plastic coats that are applied by dental professionals to the surface of teeth that have pits and fissures. Sealants isolate the tooth surface from the bacteria that colonizes the dental plaque and the acids produced by the bacteria, so that caries cannot develop.
Oral hygiene is considered a part of expected personal grooming and is fundamental to prevent periodontal diseases. For caries prevention, the most important effect of oral hygiene is the exposure of dental surfaces to fluoride from toothpaste. Plaque control by tooth brushing or flossing prevents caries by reducing the amount of cariogenic bacteria in the mouth. The well-accepted recommendation is to brush the teeth regularly with fluoridated toothpaste. Children under 2 years of age who are at high risk for caries should be brushed with a “smear” of fluoridated toothpaste; children 2 to 4 years of age should be brushed with a “small pea size” of toothpaste. Older children and adults should use an mount of toothpaste equal to the size of a pea.
Secondary prevention
Early diagnosis
Early diagnosis of caries by a dental professional can limit the spread of the disease. Considering the downward spiral model of disease, early diagnosis results in shorter and easier treatments for the patient at a lower cost. Caries also can be diagnosed and reversed before cavitation occurs, when there is only a white spot.
Prompt treatment
Dental caries lesions should be treated as soon as they are diagnosed to minimize the loss of tooth structure and the complexity of treatment. White spot lesions can be reversed with fluoride varnish, which can be applied by dental or medical professionals. Once the white spot lesion becomes a cavity, a dentist’s intervention is necessary. Neglecting small lesions is likely to result in large cavities that require more involved and more expensive treatment.
Limiting disability
Dental cavities result in loss of tooth structure and, in many cases, pain. To restore the teeth to their full functional capacity, the dentist must remove all the decayed tissue, apply materials to replace the lost structure, and reproduce its original shape. If unrestored, teeth will continue to erode, resulting in lost structure and potential pulp involvement. Once the pulp has been affected, more complex or radical treatment such as endodontic or surgical treatment will be required.
Tertiary prevention
Teeth with extensive dental caries usually must be extracted surgically. After surgery, the next opportunity for prevention is rehabilitation to avoid the consequences of impaired function and affected esthetics. Rehabilitation consists of tooth replacement with bridges anchored on remnant neighboring teeth, with implants, or with removable partial or full dentures.
Periodontal Diseases
“Periodontal disease” is a generic term describing diseases affecting the gums and tissues that support the teeth. The two main diseases included in periodontal diseases are gingivitis and periodontitis. Although both diseases are infections of bacterial origin linked to dental plaque and calculus, the severity of periodontitis is determined strongly by genetic factors and by any form of tobacco use. Gingivitis, the mildest form of periodontal disease, is an inflammation of the gums around the teeth. In untreated gingivitis, plaque and calculus accumulate between the gums and the teeth and force the gums to separate from the tooth root (loss of attachment). This separation results in a space or pocket where plaque accumulates, resulting in inflammation that develops freely and destroys the nearby bone. The opinion that all or most gingivitis lesions transition into periodontitis has been revised; it is clear now that only few patients will develop periodontitis subsequent to gingivitis. Timely dental care will prevent the disease from progressing to advanced stages. In the absence of dental intervention, treatment becomes more complex and expensive. In some instances, untreated periodontitis can remain as a chronic disease for years with the possibility of causing the loss of the affected teeth. Moreover, untreated periodontal diseases have the potential of affecting the general health of the individual because of its association with cardiovascular diseases, preterm and low birth weight pregnancy outcomes, diabetes, and kidney disease.
The symptoms of periodontal diseases may include red, swollen, or tender gums; bleeding while brushing, flossing, or eating hard food; tooth sensitivity; receding gums; loose or separated teeth, pus between gums and teeth; persistent bad breath; or a change in either how the teeth fit together or in the fit of partial dentures.
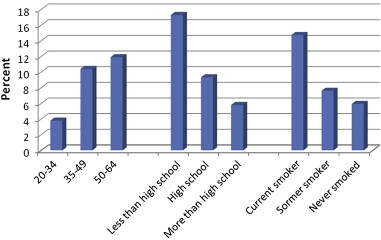
Gingivitis has decreased considerably in the United States. It is more common in children and adolescents than in adults, but severe gingivitis is uncommon in children. Periodontitis is more likely to be present among low-income persons and African Americans. Among adults 20 to 64 years of age, moderate or severe periodontitis has decreased from 9.63% in the period from1988 to 1994 to 5.08% (SE 0.34) in the period from 1999 to 2004 ( Fig. 3 ).
Primary prevention
General promotion
It is likely that periodontal diseases are the oral diseases that can benefit the most from health promotion activities. Avoidance of tobacco products is a first step to prevent periodontal diseases. Smokers are four times more likely than non-smokers to have periodontitis. Uncontrolled diabetes is strongly associated with periodontal diseases. Therefore, diabetes control is another general health promotion activity that will help prevent periodontal diseases.
Specific protection
Tooth brushing is the main intervention to prevent and treat gingivitis. Prevention of gingivitis will prevent the incidence of periodontitis. It is believed that inclusion of tooth brushing as part of the routine personal grooming has helped in the reduction of gingivitis in the United States and other countries. Daily regular dental flossing also helps prevent gingivitis and periodontitis by reducing the amount of bacteria between the teeth. Brushing and flossing should be performed despite bleeding gums. Although oral home care is the cornerstone in preventing periodontal diseases, it might not be sufficient for persons who have a strong genetic predisposition to periodontal diseases.
The role of the dental team is essential in preventing periodontal diseases. Plaque that deposits above the gums can be removed with tooth brushing and flossing. When the plaque accumulates below the gum line, a professional dental cleaning is necessary. Moreover, the guidance of a dental professional usually is necessary to achieve effective oral home care.
Secondary prevention
Early diagnosis
Early intervention of a dentist is fundamental in determining the presence of periodontal diseases, which can have a slow, silent start. Although resolution of inflammation in a timely matter can prevent or reduce damage to the tissues of support, failure to bring the gums to their natural state results in chronic inflammation and destruction of tissues.
Prompt treatment
With new techniques and medications, periodontal treatment is not particularly painful and does not involve days of recovery. The treatment guidelines from the American Academy of Periodontology emphasize that the treatment of periodontal diseases should be the least invasive possible. The dentist should start with nonsurgical treatment to clean the plaque and calculus (tartar) from the roots of the teeth and make them smooth so that plaque will be less likely to adhere again. In many cases, this cleaning might be sufficient to treat periodontal diseases; in other cases periodontal surgery is necessary to reinstate tissues’ anatomy and to facilitate oral hygiene.
Limiting disability
In some instances, surgical treatment is necessary to maintain or recover the functionality of the teeth and to reconstruct the damaged tissue. For example, when the gums have receded and the teeth roots are exposed, a soft tissue graft can be used to cover those exposed roots, avoiding additional recession and subsequent bone loss. In these cases, the graft surgery results in esthetic improvement, reduction of sensitivity to hot or cold liquids, and a decrease in the risk of developing root caries.
Tertiary prevention
Once periodontal diseases have destroyed the supporting bone, the teeth become mobile and are at high risk of being lost. Dentists can rehabilitate teeth severely affected by periodontitis with surgical procedures to regenerate some of the lost bone. A very extensive loss of support tissue requires extraction of the tooth. Teeth lost because of periodontal disease can be replaced with bridges, dental implants, or partial/full dentures.
Oral Cancer
Oral cancer includes cancer of the lip, tongue, buccal mucosa, salivary glands, and pharynx. Most oral cancers (80%) are squamous cell carcinomas, which are located most commonly on the tongue, lips, and the floor of the mouth. The strongest risk factors for oral cancer are tobacco use (smoking or chewing) and alcohol consumption.
The most frequent symptoms of oral cancer are small wounds that bleed easily and do not heal and constant pain in the mouth. Other possible symptoms include a lump or thickening in the cheek; a white or red patch inside the mouth; a sore throat or a feeling of something stuck in the throat; and difficulties chewing, swallowing, or moving the tongue or jaw.
It is estimated that in 2008 there were 35,310 new cases and 7590 deaths from oral cancer in the United States. Oral cancer is twice as common in men as in women and is particularly common among African American men, possibly because men are more likely to use tobacco and alcohol over long periods of time.
Primary prevention
General promotion
Legislation such cigarette taxes discourage smoking and thereby reduce the risks associated with smoking. Because the strongest risk factors for oral cancer are alcohol and tobacco use, the general health recommendations about avoiding smoking and smokeless tobacco (not starting or quitting) and limiting alcohol ingestion probably will protect individuals against oral cancer. Tobacco cessation as part of routine treatment provided by dentists and dental hygienists will help patients overcome their addiction to tobacco.
Specific protection
Lip cancer has been linked to high sun exposure. Therefore, the use of sun blocker lip balm and hats with a wide brim will provide protection against lip cancer.
Secondary prevention
Early diagnosis is of the utmost importance in oral cancer and truly can make the difference between life and death. The devastating consequences of oral cancer treatment also are lessened by early diagnosis.
Early diagnosis and prompt treatment
As with most cancers, oral cancer usually is treatable in its earlier stages, and the sooner the cancer is detected, the more conservative the treatment can be. Dentists and physicians should provide oral cancer examinations as part of routine examinations. Patients also should request them from their health care providers.
Limiting disability
Cancer treatment usually involves removal of the affected tissue by surgery coupled with radiation therapy. Because of the multifunctionality of the oral cavity, cancer treatment is likely to have devastating consequences on the individual’s quality of life.
Tertiary prevention
Treatment of advanced cancers usually results in serious disabilities. Rehabilitation usually involves other health professionals to address plastic surgery reconstructions, speech limitations, swallowing difficulties, and other issues.
Factors that determine availability and access to oral health care
Access to oral health care figures prominently among the health care problems facing the United States population. According to Oral Health in America: A Report of the Surgeon General, one third of Americans are without access to oral health care. Barriers to oral health care are multifactorial and include issues related to the workforce, structural and patient issues, behavioral, and socio-cultural issues. The following sections describe these factors and their impact on different subpopulations.
Workforce
Shortage and maldistribution of providers
An adequate number of dentists is necessary to address the oral health needs of Americans. The dentist-to-population ratio in the United States has been declining since 1995 and is expected to continue decreasing. The number of dentists per 100,000 United States inhabitants in 2002 was 59 and is expected to decrease to 54.3 in 2022. According to the American Dental Association, a projected increase in dentists’ clinical productivity will offset the demands of population growth. Unfortunately, dentists are not distributed evenly around the country; studies have documented that the geographic distribution of dentists is related significantly to population size and per capita income. Accordingly, the number of Dental Health Professional Shortage Areas (D-HPSA), a federal designation for areas with a deficit in the number of dentists (population-to-dentist ratio higher than 5000:1), has increased from 805 in 1991 to 3951 in 2008. A full 47 million people live in these dental shortage areas. The reality is that, for individuals residing in rural and low-income inner city areas and for some groups such as the Medicaid population, a shortage of dental providers exists.
A number of factors contribute to the shortage of dentists in economically deprived areas, including the high level of educational debt carried by recent dental school graduates and the limited availability of loan repayment and scholarship programs. According to the American Dental Education Association (ADEA), the average reported educational debt upon graduation from dental school in 2006 was $145,465. The average educational debt upon graduation increased 93.5% between 1992 and 2002, a rate that significantly exceeded the inflation rate. This impending debt pressures recent dental school graduates to choose practices in more financially lucrative areas rather than in inner-city and rural locations. The National Health Service Corps (NHSC), a federally supported loan repayment program, was established to increase the availability of health care by placing professionals in urban and rural communities that lack ready access to a range of health services. Unfortunately, this program has been affected by continuously low numbers of participating health care professionals, low retention rates, and underfunding. In 2006, 415 dentists were part of the NHSC, a far cry from the 9321 dentists required to meet the dental needs of populations in D-HPSA.
Limited scope of practice for auxiliary personnel
An important factor in the disparity of access to oral health care in the United States may be that allied dental personnel are not being used to provide all the health services for which they easily could be trained. According to the Bureau of Labor Services, in 2006 there were 167,000 dental hygienists and 280,000 dental assistants in the United States. Their scope of practice is limited, however, and requirements that auxiliary personnel work under the supervision of a dentist suggest that the declining number of dentists will restrict the capacity of the dental care delivery system. From an economic standpoint, restrictions in the scope of practice lead to decreased productivity and higher profits for the dentists. Changes in dental practice acts have the potential to increase capacity and, as a result, access to care.
Racial/ethnic homogeneity of the dental workforce
Persons from racial/ethnic minority groups are more likely to seek a health care provider who belongs to their racial/ethnic group. For instance, African Americans and Hispanics seek care from physicians of their own groups because of personal preference and language, not solely because of geographic accessibility. This preference also could be related to patients seeking culturally competent care. Surveys of practice show among dentists that dentists who belong to racial/ethnic minority groups treat significantly higher proportions of urban, less formally educated, and lower-income patients than do their non-minority colleagues. Similarly, African American dentists are more likely than their non-African American colleagues to practice in areas that have a higher residential African American population. African American patients are more likely to receive care from an African American dentist. Effectively, 62% of black patients are seen by black dentists, and only 10.5% of black patients receive their care from white dentists.
Despite changes in the racial and ethnic mix of the country, the representation of racial and ethnic minorities in the dental profession lags behind their representation in the general population. African Americans and Latinos represent 27% of the total population of the United States but only 11% of the students entering dental schools. This lack of racial/ethnic diversity in the dental work force is recognized as a major concern for the profession and the public because it hampers the profession’s ability to provide adequate care to racial/ethnic minority groups.
Curricular and training deficiencies
The curricula of dental education have been characterized as overcrowded. A packed 4-year curriculum does not allow comprehensive exposure to certain population groups, limiting the graduates’ ability to deal with the particular needs of these groups. Certain groups, such as the frail elderly, patients who have special needs or who are medically compromised, and young children face considerable barriers in accessing dental care. It is possible that the dental workforce is not trained appropriately to address the oral health needs of these populations. This problem is exacerbated by the perception of many dentists that these individuals are more difficult to treat and that the reimbursement is inadequate to cover operational expenses. A survey conducted among dental schools in 2003 showed that during the past 20 years the didactic teaching of geriatric dentistry had increased significantly, but the clinical experience had not kept pace. As a result, in 2002 dental school seniors reported that they were not well prepared to provide care for older individuals. The ADEA survey of graduating dentists in 2000 showed less satisfaction with the time devoted to pediatric dentistry education than in previous years. A shrinking number of faculty members and a limited number of patients seem to affect the ability of dental institutions to train general dentists appropriately in the management of the pediatric patient.
Structural Issues
Financing of dental care, dental insurance, and use of services
In 2006, $91.1 billion was spent on dental care; $86 billion was paid by private sources, and only $5.5 billion was paid by the federal and state governments, Although in 1990 expenditures for dental services represented 11.1% of total health expenditures, in 2005 that figure had decreased to 6.3%. The resources allocated for oral health determine the scope and magnitude of programs targeting disadvantaged populations. Reduced state and federal budgets for oral health programs have led to increased numbers of uninsured and underinsured individuals and to an overburdened safety net.
The availability of dental insurance is important because the cost of dental care is a barrier to receiving regular care and maintaining good oral health. A review of the literature on the effects of dental insurance on the demand for dental care found that insured individuals are more likely than their uninsured counterparts to seek dental care. Although 47 million Americans lack health insurance, 108 million lack dental insurance; in 2004, 35% of the United States population was uninsured for dental care for the whole year. The elderly, racial/ethnic minorities, and low-income persons are recognized as having the most critical need for dental care. Unfortunately, they are the least likely to have the financial resources or dental insurance to pay for dental care. Among older Americans, the ability to pay for dental care deceases with retirement because of the decrease in income and the loss of employer-based insurance coverage. According to the 2004 Medical Expenditure Panel Survey (MEPS), poor and low-income families were more than likely high-income families to be uninsured (41% and 47% versus 25%). Likewise, African Americans and Hispanics were more likely than non-Hispanic whites to have public dental insurance coverage. Lamentably, even when the financial barrier is removed, use seems to vary by insurance group. According to the same study, 57% of the population with private insurance had a dental visit, but only 32% of the population with public dental insurance visited the dentist.
Inadequate federal and state programs
Publicly subsidized programs such as Medicaid and the State Children’s Health Insurance Program (SCHIP) provide coverage for dental care for low-income individuals. These programs, however, have limitations that hamper their effectiveness in increasing access to dental services at the community level.
Even though Medicaid provides dental benefits for selected adults in some states, both the Medicaid and SCHIP programs target mainly low-income children. Very low participation from dentists in the Medicaid and SCHIP program is a chronic problem. Approximately only 25% of all dentists reported seeing Medicaid patients in their offices. Providers often cite inadequate reimbursement as the reason for their low rate of participation. Other issues include administrative problems, such as complicated paperwork, slow reimbursement, and claims denials, and patient-related issues, including poor compliance in keeping appointments and following treatment recommendations. A review of the literature concluded that higher reimbursement rates were necessary but not sufficient to increase provider participation in Medicaid. To improve their programs, Medicaid agencies must revamp administrative practices and build partnerships with dental societies.
The SCHIP program was designed to provide access to care for children in working poor families, that is, families with incomes above the threshold of eligibility for Medicaid (up to 200% of the federal poverty level). A few studies have documented the effect of SCHIP on dental use and inferred limited positive impact.
Dental coverage for adults is elective, and benefits vary greatly by state. In many instances coverage is limited to emergency care, and the extent of benefits fluctuates according to state budgets. Expanding dental coverage for adults might decrease access barriers.
Limited dental public health infrastructure
The infrastructure for dental public health is the foundation on which public dental programs and activities are planned, implemented, and evaluated. Unfortunately, the dental public health workforce is underappreciated and has a low priority in the United States society in general, with limited resources to address the great unmet needs of the country. An assessment of the dental public health infrastructure concluded that the workforce is small, most state programs have limited funding, the discipline has minimal presence in academia, and its role in the regulation of dentistry and dental hygiene is small. The number of public health dentists is limited: in the United States, 2032 dentists and only 155 active board-certified specialists work in public health.
Federally qualified health centers and rural health centers often serve as safety net providers for dental care. Currently, around 1200 health centers deliver care through more than 6600 service delivery sites serving 18 million Americans nationwide. In 2003, 65% of the federally funded community health care centers and 85% of the migrant health care centers provided some type of dental care. A study that examined the capacity of the dental safety net to meet the needs of the underserved population concluded that the current system had the capacity to care for about 7 to 8 million people annually with the potential of increasing this figure to 10 million. A comparison of this limited capacity with the high number of uninsured and low-income individuals led to the conclusion that any substantial strategy to address the unmet dental needs of Americans will require the participation of private practitioners.
Population Issues
Patient behavioral and socio-cultural issues
Removing structural and financial barriers is an important step toward eliminating disparities in access, but it is not sufficient, because there are other important determinants. Care for patients, especially those from vulnerable groups, is a complex issue. A major factor leading to underutilization of dental care is the educational and cultural gap between patients and dentists. Patient characteristics such as race, education level, cultural values associated with oral health, level of perceived disease burden, and disease severity have an influence on treatment. Negative experiences when trying to access dental care services, such as difficulty finding a provider, scheduling convenient appointments, transportation, long waiting times, taking time off work, and discriminatory treatment, may affect the willingness of patients to seek dental care.
Another important barrier to dental care is the choice socially disadvantaged populations must make between fulfilling basic needs and seeking and paying for dental care. In this situation, dental care becomes a luxury that is relegated to a second place after basic needs are fulfilled. Lack of awareness about the benefits of regular dental visits, as opposed to episodic visits, also affects the use of dental care. It is particularly important that caregivers of low-income children be aware of the need for measures for preserving oral health, because such awareness is a strong predictor of children’s use of dental care.
Similarly, dentists’ characteristics, including practice specialty, practice style, and attitudes or bias about patients’ ethnicity and social background, may influence the type and quality of services rendered. As the dental profession deals with an increasingly diverse population, the lack of cultural and linguistic competence among providers represents an additional barrier to care.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


