Use of the Energy Nutrients
Metabolism and Balance
• Calculate energy needs according to the patient’s weight and activities.
• Explain physiological sources of energy.
• Identify factors affecting the basal metabolic rate.
• Assess factors affecting energy balance.
• Summarize the effects of inadequate energy intake.
• Explain the principles for and importance of regulating energy balance to a patient.
• Individualize dental hygiene considerations to patients regarding energy metabolism.
• Relate nutritional directions to meet patients’ needs regarding energy metabolism.
Metabolism
In metabolic activity, the two major chemical reactions are catabolism and anabolism. Catabolism is splitting complex substances into simpler substances; anabolism is using absorbed nutrients to build or synthesize more complex compounds (see Chapter 2 or online at Evolve for more detail). Anabolism and catabolism are continuous reactions in the body. Cells in the epithelial lining of the oral and gastrointestinal mucosa are replaced approximately every 3 to 7 days. Despite this rapid turnover, the rate of catabolism is usually equal to that of anabolism in a healthy adult. During certain stages of life, such as growth periods or pregnancy, more anabolism is occurring than catabolism. Conversely, when illness or stress occurs, excessive catabolism is evident.
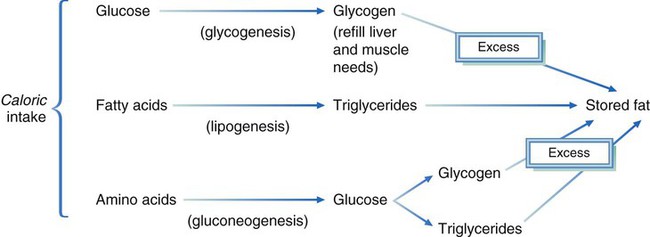
Other phases of metabolism include delivery of nutrients to the cells where they are needed, and delivery of wastes to sites where they can be excreted. After absorption of the macronutrients, glucose, fatty acids, and amino acids can be used to yield energy via a common pathway within the mitochondria of cells (Fig. 7-1). The catabolic end products of carbohydrates, proteins, and fats are carbon dioxide, water, and energy. Nitrogen is an additional end product of protein.
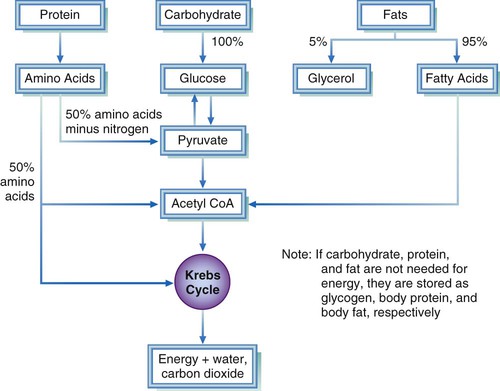
The Krebs cycle (also called citric acid cycle or tricarboxylic acid [TCA] cycle) converts glucose, fatty acids, and amino acids to a usable form of energy, requiring many enzymes. Additional information on the TCA cycle can be found in Chapter 2 and online at Evolve. For activation of some enzymes, vitamins or minerals or both must be available. An enzyme needing vitamins for activation is called a coenzyme. Thiamin, riboflavin, and niacin are B vitamins essential as coenzymes in the TCA cycle. An enzyme may also require a cofactor. A cofactor functions in the same way as coenzymes, but the molecule required is a mineral or electrolyte.
Carbohydrate Metabolism
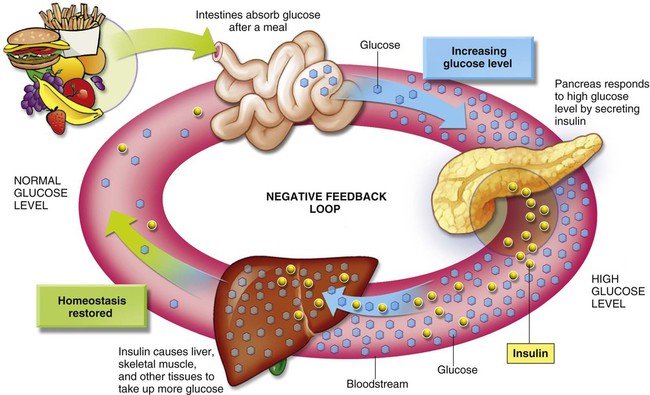
Monosaccharides are transported through the portal vein to the liver for glycogenesis, a process in which sugars, including fructose, galactose, sorbitol, and xylitol, may be stored as glycogen. Glucose is the circulating sugar in the blood; it is the major energy supply for cells. The level of circulating glucose is closely monitored by the liver and is constantly maintained at a normoglycemic level (normal blood glucose range), between 70 and 100 mg/dL. Insulin is a hormone that lowers blood glucose levels. Blood glucose levels peak at 140 mg/dL 30 to 60 minutes after a meal and return to normal within 3 hours in individuals with normal secretion and use of insulin. This consistent blood glucose level is significant, indicating the necessity of a certain amount of glucose in the blood for normal functioning of body tissues (Fig. 7-2). Hyperglycemia (elevated blood glucose) and hypoglycemia (decreased blood glucose) are very serious conditions that could be fatal; the precipitating cause for either should be identified. Many patients with diabetes who take insulin or an antidiabetic medication that can cause hypoglycemia, or both, may exhibit symptoms related to hypoglycemia, particularly if they have not eaten within a 4- to 5-hour time span. These patients need to be treated with a carbohydrate source before continuing treatment (see Health Application 7).
Individuals with diabetes often respond differently to different carbohydrate sources. It is important for patients with diabetes to closely manage and monitor their glycemic levels. The blood glucose response to different foods and different combinations of food cannot be accurately predicted from the amount of simple sugars or complex carbohydrates ingested.1 White bread, potatoes, and white rice have a glycemic effect similar to sucrose. Glycemic effect is the rate at which glucose increases in the bloodstream after a particular food is eaten.
A complex hormonal system maintains a constant blood glucose level. Insulin is the primary hormone that lowers blood glucose levels. When hyperglycemia occurs, insulin is secreted to decrease blood glucose levels. Conversely, hypoglycemia elicits the secretion of several hormones (thyroid hormone, epinephrine, glucagon, and growth hormone) to increase blood glucose levels. The liver can elevate blood glucose levels by converting amino acids from protein, and glycerol from fats to glucose. The process of synthesizing glucose from noncarbohydrate sources is known as gluconeogenesis (see Chapter 2 or online at Evolve for additional details).
Lipid Metabolism
The process of hydrolyzing triglycerides into two-carbon entities to enter the Krebs cycle for energy production is known as oxidation. A discussion of oxidation can be found in Chapter 2 and online at Evolve. During oxidation, 1 lb of fat results in the release of 3500 kcal for energy—more than most individuals use in a 24-hour period. When excessive amounts of fats are oxidized for energy, the liver is overwhelmed, and acidic metabolic products, or ketones, are formed. Ketones are not oxidized in the liver, but are carried to the skeletal and cardiac muscles, where, under normal circumstances, they are rapidly metabolized.
Alcohol Metabolism
Although alcohol is considered a drug, the kilocalories it provides can be used by the body for energy, providing approximately 7 kcal/g. When consumed in excessive amounts, alcohol is a toxin. Caloric content of alcoholic beverages can be calculated by using the equations in Box 7-1. Alcoholic beverages contain negligible nutrients.
A well-balanced diet accompanied by habitual consumption of alcoholic beverages in excess of energy needs can be a risk factor for weight gain. However, excessive amounts of alcohol in a person who is an alcoholic tend to result in poor appetite for food and may lead to weight loss and malnutrition. In addition to causing liver damage, alcohol can interfere with the transport, activation, catabolism, and storage of almost every nutrient. Alcohol has a marked effect on blood pressure and risk of hypertension.2
The Dietary Guidelines advise moderation in alcohol consumption: one drink a day for women and no more than two drinks a day for men. (An alcoholic beverage is defined as 12 oz of regular beer, 5 oz of wine, or 1.5 oz of 80-proof distilled spirits.) For middle-aged and older adults, one to two drinks daily results in the lowest mortality rate.3 This is perhaps a result of the protective effects of moderate alcohol consumption on CHD. Alcohol consumption seems to provide little, if any, health benefit for younger individuals. Alcoholic beverages should be avoided by women who may become pregnant, are pregnant or breastfeeding.
Metabolic Interrelationships
The body is an overwhelmingly complex system. Whether excessive food intake is in the form of protein, carbohydrate, fat, or alcohol, most excess energy intake is stored as adipose tissue (Fig. 7-3). (Glycogen is another storage form of energy; however, the amount of glycogen stored in the body is limited.)
Metabolic Energy
Energy Production
The metabolism of basic nutrients results in production of cellular energy, which is stored as adenosine triphosphate (ATP). ATP is an instant source of cellular energy for mechanical work, transport of nutrients and waste products, and synthesis of chemical compounds generated from the Krebs cycle. ATP units, also called high-energy phosphate compounds, are the currency, or “money,” the body uses for energy. Because ATP can be metabolized without oxygen, the reaction is classified as anaerobic. The body must always have a supply of ATP, and several systems ensure a constant supply in the body. More detailed discussion of ATP can be found in Chapter 2 and online at Evolve.
Basal Metabolic Rate
Even during sleep, the body requires energy for the basic minimum tasks of respiration and circulation, and for many intricate activities within each cell. Basal metabolic rate (BMR) indicates the energy required for involuntary physiological functions to maintain life, including respiration, circulation, and maintenance of muscle tone and body temperature. The BMR is lowest while lying down, awake, rested, and relaxed in a comfortable environment, not having eaten for 12 to 15 hours. The BMR can be measured in a clinical setting using indirect calorimetry, which indirectly measures the rate of oxygen used while the person is resting (see Fig. 7-4). Because digestion and absorption require energy, the BMR is the amount of energy required when the body is in a postabsorptive state (digestion and absorptionare minimal).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses