Slightly more than 1 child in 900 is born with cleft lip with or without cleft palate. Among children born with cleft lip and palate, approximately 37% are born with an isolated cleft lip, and approximately 63% are born with cleft lip and palate. Most cases of cleft lip and palate—approximately 70%—occur as isolated anomalies, whereas approximately 30% occur in association with other congenital anomalies and recognized syndromes. Most large tertiary care centers offer interprofessional care for children who have orofacial clefts. Numerous specialists take part in cleft rehabilitation, with most teams including a plastic surgeon, pediatrician, pediatric dentist, oral and maxillofacial surgeon, orthodontist, prosthodontist, social worker, speech and language pathologist, otolaryngologist, audiologist, psychologist, psychiatrist, and clinical coordinator nurse. Interprofessional care is designed to integrate physical, social, and psychological rehabilitation.
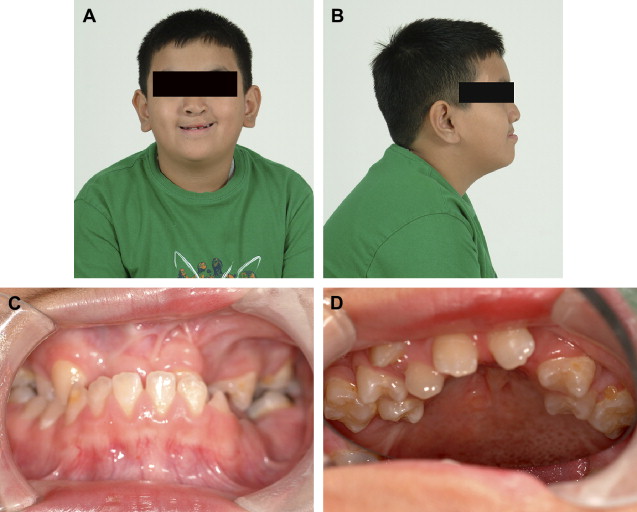
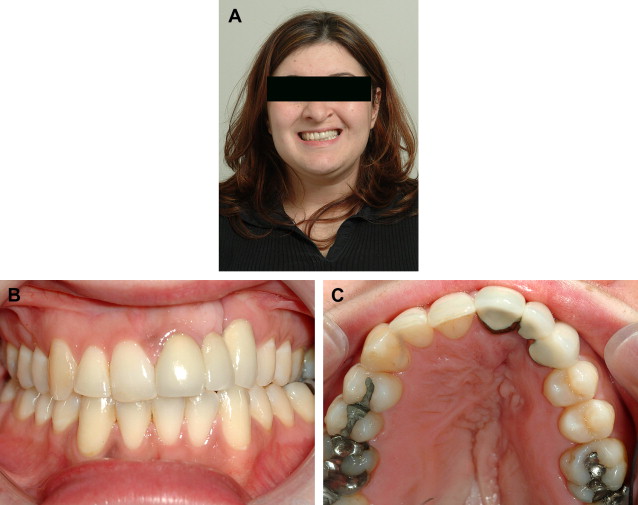
Primary corrective surgery is usually accomplished within the first year after the birth of a baby who has a cleft anomaly: repair of the lip is usually performed at 3 months, and repair of the palate is usually performed at 6 months. Repair of the alveolar process is performed much later—between the ages of 9 and 11 years. When bone grafting of the alveolus is performed during the mixed dentition stage before eruption of the permanent canine—that is, between the ages of 9 and 11 years—it is called secondary alveolar bone grafting ( Fig. 1 ). When it is performed after eruption of the canine, it is called tertiary alveolar bone grafting. The most widely accepted protocol for repair of the alveolar process is secondary alveolar bone grafting because it allows for eruption of the cleft-adjacent teeth—usually the lateral incisor and canine—through the graft ( Fig. 2 ). Eruption of teeth through the graft into a functional occlusion provides physiologic stress, which promotes remodeling of the graft. Satisfactory results have been reported after tertiary alveolar bone grafting when the transplanted bone is stressed functionally by placement of a dental implant into the grafted alveolar cleft. Alveolar bone grafting should not be considered an isolated procedure but integral to comprehensive orthodontic therapy. An important condition for a successful alveolar bone graft may include the forces of orthodontic treatment, which are thought to subject the graft to additional functional stresses, promote a physiologic remodeling, and ultimately prevent its resorption.

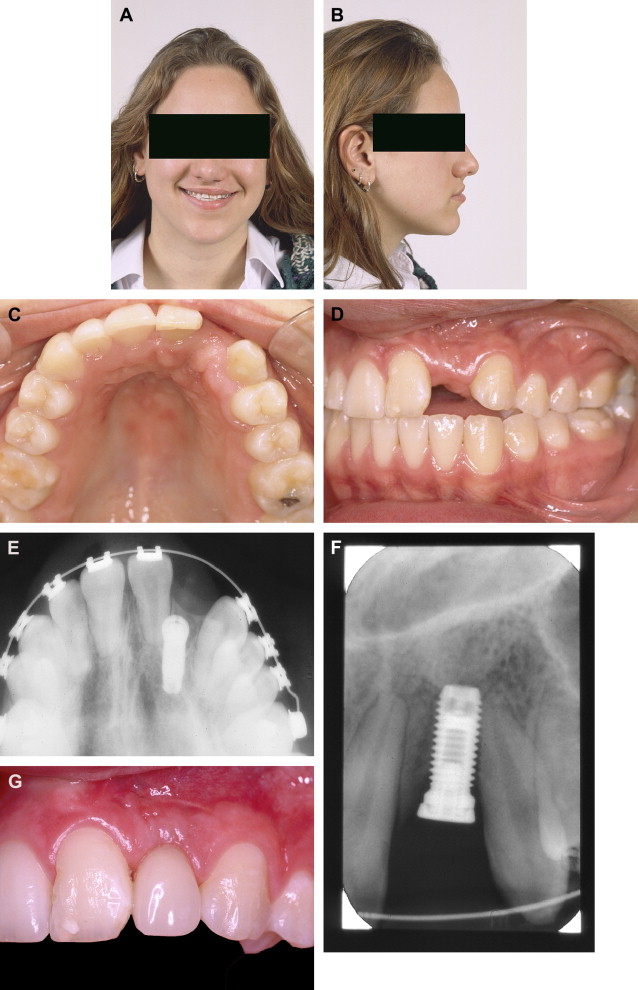
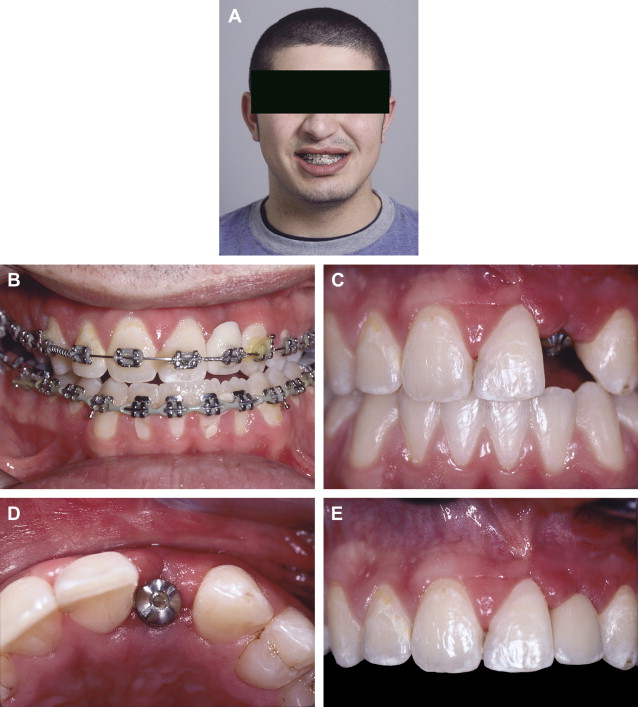
Comprehensive orthodontic therapy is usually initiated after eruption of the permanent canines and premolars. General goals of orthodontic therapy include expanding the maxilla and correcting cross bites, facilitating eruption of teeth, establishing a class I canine and molar relationship, and establishing correct midlines and alignment. A choice must be made to close the cleft dental gap orthodontically or open it for prosthodontic habilitation, in which case the list of orthodontic goals must be lengthened to include optimizing the dimensions of the edentulous gaps and achieving root parallelism adjacent to edentulous gaps. Whenever possible, management of the alveolar cleft should involve a strategy to avoid prosthodontic treatment as long as facial profile, dental aesthetics, and function are unlikely to be compromised. In any case, invasive traditional crown and bridge procedures should be avoided when possible ( Fig. 3 ). Orthodontic gap closure and substitution of a mesialized canine for a missing maxillary lateral incisor would be considered if a reasonable aesthetic and functional outcome could be expected. In order for a canine substitution to provide an acceptable result, factors such as skeletal pattern, occlusal relationships, tooth size/arch length coordination, and size, shape, and color of the canine relative to the central incisor should be favorable.
The size of the maxilla may govern the decision to close the gap orthodontically or open it and fill the space prosthodontically. Most clefts are associated with an element of maxillary hypoplasia; if the maxilla is marginally retrusive and gap closure cannot be accomplished orthodontically without adversely affecting the jaw relationship, overjet, and facial profile, then the gap should be opened and the missing tooth—usually the lateral incisor—should be replaced ( Figs. 4–8 ). Similarly, tooth-size discrepancies may contribute to the tendency of maxillary retrusion to influence the decision whether to close or open the gap. The enamel of cleft-adjacent teeth is commonly hypoplastic, which results in them being smaller than normal, so orthodontic consolidation typically results in retraction of anterior teeth, loss of overjet, and deviation of the maxillary midline toward the side of the cleft.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


