Dental anomalies include structural defects in enamel and dentin, fusion of teeth, and hamartomas such as odontomas. Enamel defects occur as a heterogenous spectrum of types, with different genetic etiologies, known collectively as amelogenesis imperfecta. They range in severity from barely discernible to aplasia. They may occur as a single defect or as but one defect in a recognizable pattern of defects such as epidermolysis bullosa or generalized odontodysplasia. Dentin defects are much less clinically heterogeneous, and can occur alone or in association with osteogenesis imperfecta.
Amelogenesis imperfecta
Amelogenesis imperfecta (AI) is a heterogeneous group of hereditary disorders that adversely affects enamel development and causes abnormalities in the amount, structure, and composition of enamel without evidence of systemic disease. Winter and Witkop and coworkers have delineated at least 12 distinct types of AI using a combination of clinical, radiographic, histologic, and genetic criteria.
Transmission of the responsible gene may take place by autosomal dominant, autosomal recessive, X-linked dominant, and X-linked recessive modes. More recently, some defective enamel proteins and their causative genes have been identified. Mutations of the enamelin gene (ENAM) located on chromosome 4q21 have been identified in autosomal dominant forms. Smooth hypoplastic AI and local hypoplastic AI are two clinically distinct phenotypes of autosomal dominant forms associated with ENAM mutations. The X-linked form results from mutations in the Amelogenin protein with the causative gene AMELX located on chromosome Xp21.12. Different mutations have been identified, and depending on the mutations, phenotypes can vary. The genes responsible for autosomal recessive AI types have not been identified, and it is not known whether their diverse phenotypes are the result of either allelic gene mutations or mutations in multiple genes.
Three broad groups of AI can be distinguished on clinical and radiographic grounds alone. First there exists a hypoplastic group in which the enamel is reduced in quantity but is relatively well mineralized. The enamel may present with white flecks, narrow horizontal bands, lines of pits, grooves, and discoloration of the teeth that varies from yellow to dark brown. In the second group, hypocalcification is noted. The enamel is formed in relatively normal amounts but is poorly mineralized. In this form, the enamel is soft and friable and may show a chalky, dull color or cheesy consistency. In the third group there is hypomaturation of the enamel. In this group, the final stages of the enamel mineralization process are abnormal. The enamel is harder with a mottled, opaque white to yellow-brown or red-brown color. The prevalence of AI is reported as being 1 in 700 in northern Sweden, 1 in 14,000 in the United States, and 1 in 2000 in the United Kingdom.
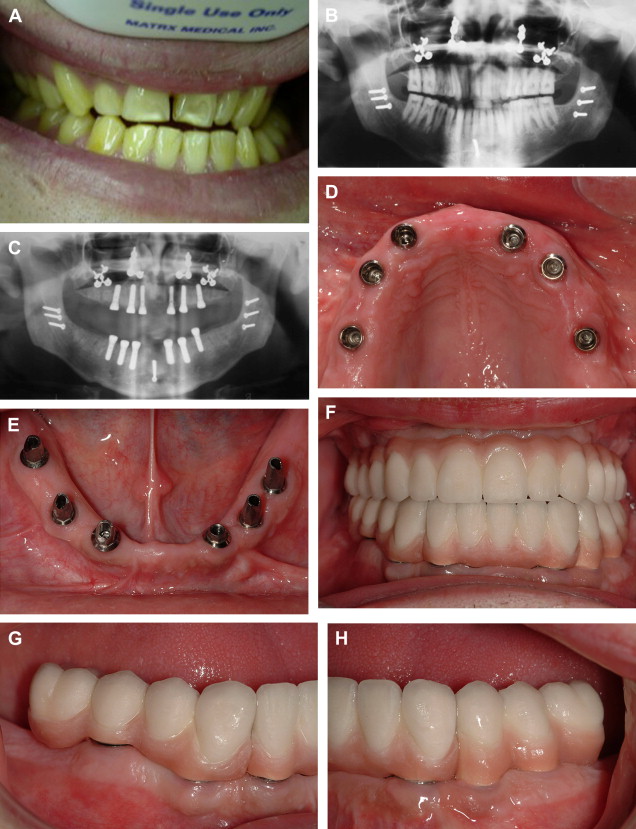
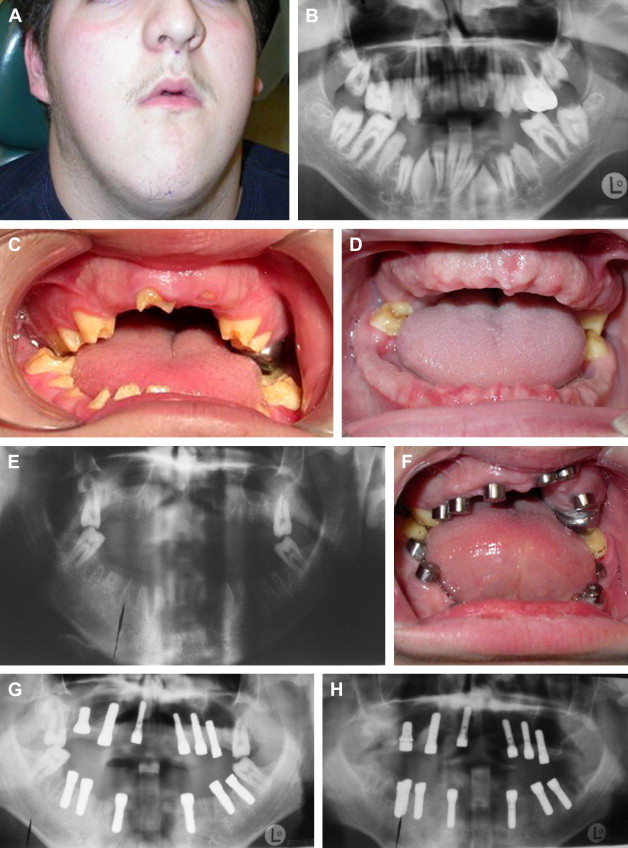
The primary clinical problems of AI are atrrition and shear fractures of enamel, susceptibility to caries, sensitivity, pain, periodontitis, endodontic infections and compromised esthetics ( Fig. 1 ). The severity of these problems varies among the different types of AI. Several reports have described malocclusion that occurs in some patients with AI that is characterized by an anterior open bite. Rowley and colleagues found 20% of subjects with severe anterior open bite and 44% with a severe vertical dysgnathia characterized by large gonial and maxillary-mandibular plane angles together with increased lower facial height ( Fig. 2 A). With such steep mandibular plane angles, it is not surprising to find occlusal stops on only the first or second molars. There may also be multiple retained deciduous teeth and unerupted and impacted permanent teeth. Extraoral findings may also include a short upper lip and incompetent lips. Local factors, such as abnormal tongue activity and deglutition pattern, are the effects rather than causes of vertical dysgnathia. The anterior open bite is skeletal rather than dental in origin ( Fig. 2 A–C).

The psychological effects of living with a grossly malformed dentition cannot be underestimated. Besides the problems delineated above, patients who have AI often complain of relentless teasing at school by their peers.
There may be a strong family history of similar affliction. For example, the patient in Fig. 2 had a history involving his mother, mother’s brother and sister, and a maternal grandfather and great-grandfather. In that case, a diagnosis of AI–hypocalcified, autosomal dominant type was made.
Management of amelogenesis imperfecta with dental implants
It is crucial that patients who have AI be informed of their diagnosis and the mode of inheritance of their particular condition. Treatment may range from doing nothing in mild cases, to full- or partial-mouth restoration with crowns in moderately severe cases. The 75% survival rate for crowns has been estimated at 11 years. Other studies have reported 8- to 10-year survival rates of between 85% and 95% for crowns and cast inlays/onlays. Some authors have reported median survival time for crowns of 14 years. It is likely that survival rates for crowns in patients who have AI are significantly worse. In severe cases where clinical crown lengths are deficient because of generally incomplete eruption, crowning of the teeth may prove impossible because of the inability to create adequate resistance and retention form in tooth preparations. Moreover, in cases of severe penetrance of the hypomature or hypocalcified type of AI, well-defined, smooth finish line may be impossible to produce in the weak, pitted and flaking enamel thus increasing the likelihood of producing a crown margin deficiency that is less resistant to caries. When a clinically acceptable finish line is created, the enamel may fracture intra-operatively or following cementation of the crown.
Periodontitis is commonly found in association with AI, in part because roughness of the enamel promotes bacterial plaque retention. This is only exacerbated by placement of crown margins near the gingival margin, particularly when they are made to invade the gingival sulcus in an attempt to increase clinical crown length or in search of less fragile, less porous enamel on which to fashion a smooth finish line.
Surgical orthodontics may be impeded by the inability to bond orthodontic brackets securely to dysplastic enamel, and attempting to circumvent this problem by temporizing the dentition with acrylic resin crowns prior to application of fixed orthodontic hardware exposes the patient to a heightened risk of cement washout and caries. Furthermore, insecure temporary crowns introduce the possibility that intermaxillary fixation may be ineffectual. Unless orthodontic treatment can be conducted reliably, surgical orthodontics in patients who have AI is ill-advised.
We reckon that in young patients with AI a conventional oral reconstruction using crowns, if possible in the first place, would have to be replaced multiple times over the course of his or her lifetime, and may in the end condemn the patient to edentulation anyway. The costs of implant- and tooth-supported reconstructions are comparable in many jurisdictions, therefore, it may be most cost-effective to edentulate the unrestored dentition and rehabilitate with implant-supported restorations from the outset of skeletal maturity ( Fig. 3 ). This strategy presupposes that implant-supported restorations can last many years without costly maintenance, and indeed that the implants on which they rest can remain functional for the better part of a lifetime, suppositions which have yet to be proven.