In this article, we report an incident of transient neuropathy secondary to tooth movement involving the inferior alveolar nerve. This clinical report reflects the need to thoroughly examine potentially high-risk patients for neuropathy using advanced diagnostic tools such as cone-beam computed tomography when diagnosing and planning treatment.
Transient neuropathy secondary to orthodontic tooth movement has been reported as a rare occurrence. Nevertheless, reports of paresthesia during orthodontic treatment reflect the need to thoroughly assess the possible risk of injury to the inferior alveolar nerve before the start of orthodontic therapy as part of the process of informed consent.
Orthodontic treatment involves complicated tooth movements in 3 dimensions. Accurate assessment of root proximity to the inferior alveolar nerve in the buccal and lingual dimensions might not be possible with conventional 2-dimensional panoramic radiographs. This indicates the need for a cone-beam computed tomography (CBCT) scan in potentially high-risk patients. A CBCT scan is considered an accurate method to evaluate the position of the mandibular canal. To determine the course of the inferior alveolar nerve bundle suggests the need for CBCT before attempting treatment in this area to minimize the risk of neuropathy.
Sensory disturbances of the lower lip are more commonly reported as a result of orthognathic surgery to the lower jaw, internal rigid fixation of mandibular fractures, removal of third molars, dentoalveolar surgery, endodontic treatment, or a tumor near the mandibular canal. To date, there are only a few case reports of paresthesia after tooth movement impinging the inferior alveolar nerve. The reported causes of nerve disturbances are all classified as neuropraxias or first-degree nerve injuries. Neuropraxia results from minor compression of the nerve trunk, causing a conduction blockade. Axonal continuity is maintained; this results in a temporary conduction blockade. Patients clinically report sensory disturbances lasting from hours to months, usually with complete sensory recovery. We present a case report of sensory disturbance of the lower lip and the chin occurring during inadvertent intrusion of a third molar into the inferior alveolar nerve canal during orthodontic treatment.
Case report
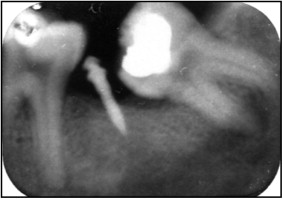
A healthy 27-year-old man came for orthodontic treatment to address his chief complaint of “correcting his crooked teeth.” After analyzing his clinical examination findings and records, we determined that a nonsurgical extraction treatment plan with a temporary skeletal anchorage device was necessary to align his severely crowded teeth ( Fig 1 ). The clinical examination showed a symptomatic endodontically treated maxillary right first molar (tooth 16; Federation Dentaire Internationale tooth numbers are used throughout this article) with a large amalgam restoration. The decision was made to extract the symptomatic molar and the maxillary left first premolar (tooth 24). Because the patient was already missing the mandibular second molars bilaterally, retraction of the posterior segments into these edentulous spaces using a temporary skeletal anchorage device and the existing third molars for additional anchorage was planned. The third molars would eventually be extracted at the completion of treatment. The initial panoramic radiograph showed the close proximity of the mandibular third molars (teeth 38 and 48) to the inferior alveolar nerve ( Fig 2 ).


After extraction of teeth 16 and 24, a temporary skeletal anchorage device (Vector; Ormco, Glendora, Calif) was placed in each posterior quadrant to facilitate anchorage for the retraction. A maxillary transpalatal arch was cemented on teeth 17 and 27 to facilitate intrusion of these molars and reinforce anchorage. All temporary skeletal anchorage devices were placed under local anesthesia (2% lidocaine, 1:100,000 epinephrine) with no postoperative complications ( Fig 3 ). Blugloo (Ormco) was placed on the occlusal surfaces of teeth 38 and 48 to free the interocclusal contact to facilitate the distalization ( Fig 4 ).


For the maxillary arch, sectional mechanical principles were used after bonding with an 0.018-in Victory MBT (3M Unitek, Monrovia, Calif) prescription fixed appliance. Bondable buttons were used to retract teeth 36 and 46 individually with elastomeric power chains. Power chains were used on the buccal and lingual surfaces so as not to cause a rotational moment while retracting the mandibular first molars ( Figs 3 and 4 ).
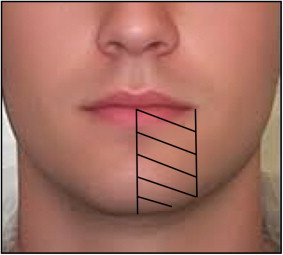
To facilitate the retraction of teeth 36 and 46, 2 mm of Blugloo was placed on the disto-occlusal surfaces of teeth 38 and 48 on April 5, 2011. After this, the patient came for routine adjustment appointments on April 26 and May 2, 2011, with no postoperative complaints or complications. He reported tingling and numbing of his lower left lip and chin beginning on May 5, 2011, exactly 1 month after the Blugloo placement. The numbing sensation continued to increase to a 90% loss of feeling in this area by May 16, 2011 ( Fig 5 ), 41 days after the temporary skeletal anchorage device placement. On May 16, 2011, he came to the clinic to address his concerns of paresthesia. He was assessed by the attending periodontist (A.C.) and orthodontist (W.A.W.) using mechanoceptive testing via 2-point discrimination. The examination showed paresthesia in the area innervated by the inferior alveolar nerve ( Fig 5 ). At this time, the radiographic examination showed no evidence of pathologic entities and ruled out any potential issues with the temporary skeletal anchorage device placed mesially to tooth 38 ( Fig 6 ). The most reasonable explanation of the sensory disturbance was that the third molar was invading the space of the inferior alveolar nerve as it was being intruded by the Blugloo placed on April 5, 2011.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


