Upper Eyelid Approach
The most direct and cosmetically appealing approach to the superolateral orbital rim is the upper eyelid approach, also called upper blepharoplasty, upper eyelid crease, and supratarsal fold approach. In this approach, a natural skin crease in the upper eyelid is used to make the incision.
SURGICAL ANATOMY
Upper Eyelid
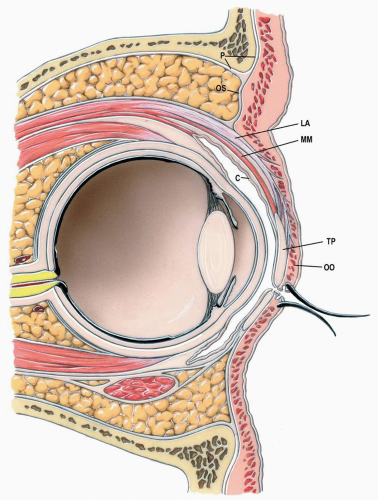
In sagittal section, the upper eyelid consists of at least five distinct layers: the skin, the orbicularis oculi muscle, the orbital septum above or levator palpebrae superioris aponeurosis below, Müller muscle/tarsus complex, and the conjunctiva (see Fig. 5.1). The skin, orbicularis oculi muscle, and conjunctiva of the upper eyelid are similar to those of the lower eyelid (see Chapter 2). The upper eyelid differs from the lower eyelid, however, by the presence of the levator palpebral superioris aponeurosis and Müller muscle.
Orbital Septum/Levator Aponeurosis Complex
Deep to the orbicularis oculi muscle lies the orbital septum/levator aponeurosis complex. Unlike the situation in the lower eyelid, where the orbital septum inserts into the tarsal plate, in the upper eyelid it extends inferiorly and blends with the levator aponeurosis approximately 10 to 15 mm above the upper eyelid margin. The levator muscle usually becomes aponeurotic at the equator of the globe in the superior orbit. The aponeurosis courses anteriorly to insert onto the anterior surface of the lower two thirds of the tarsal plate. Extensions of the levator aponeurosis also extend anteriorly into the skin of the lower portion of the upper eyelid. The aponeurotic portion of the levator behind the orbital septum is much wider than the muscle from which it is derived, and its medial and lateral extensions are known as horns or cornua. The lateral horn of the levator is prominent and deeply indents the anterior portion of the lacrimal gland to divide it into thin palpebral and thick orbital portions; its lateral extension attaches to the orbital wall at the orbital (Whitnall) tubercle. The weaker medial horn of the levator aponeurosis blends with the orbital septum and the medial check ligament.
Müller Muscle/Tarsus Complex
Deep to the levator aponeurosis the Müller muscle lies superiorly while the tarsus lies along the eyelid margin. Müller muscle is a nonstriated,
sympathetically innervated elevator of the upper eyelid. It originates from the inner surface of the levator aponeurosis and inserts onto the superior surface of the upper tarsal plate. The tarsal plate of the upper eyelid is a thin, pliable fibrocartilaginous structure that gives form and support to the upper eyelid. Embedded within the tarsal plate are large sebaceous glands—the tarsal or Meibomian glands. The edge of the tarsus adjacent to the free border of the eyelid is parallel to it, whereas the deeper (superior) border is curved such that the tarsus is somewhat semilunar in shape. It is also curved to conform to the outer surface of the
eyeball. The superior tarsus is considerably larger than the inferior tarsus, the greatest height of the superior tarsus being approximately 10 mm and that of the inferior tarsus being approximately 4 to 5 mm (see Figs. 2.6A and B). The tarsal glands sandwiched between the layers of fibrocartilage in the upper eyelid exit on the eyelid margin near the eyelash follicles. The eyelashes are supported by their roots, attached to fibrous tissue on the tarsal plate, not in the orbicularis oculi muscle anterior to the tarsal plate. Laterally, the tarsal plate becomes a fibrous band that adjoins the structural counterpart from the lower eyelid, forming the lateral canthal tendon. Medially, the tarsal plate also becomes fibrous and shelters the superior lacrimal canaliculus behind as it becomes the medial canthal tendon.
sympathetically innervated elevator of the upper eyelid. It originates from the inner surface of the levator aponeurosis and inserts onto the superior surface of the upper tarsal plate. The tarsal plate of the upper eyelid is a thin, pliable fibrocartilaginous structure that gives form and support to the upper eyelid. Embedded within the tarsal plate are large sebaceous glands—the tarsal or Meibomian glands. The edge of the tarsus adjacent to the free border of the eyelid is parallel to it, whereas the deeper (superior) border is curved such that the tarsus is somewhat semilunar in shape. It is also curved to conform to the outer surface of the
eyeball. The superior tarsus is considerably larger than the inferior tarsus, the greatest height of the superior tarsus being approximately 10 mm and that of the inferior tarsus being approximately 4 to 5 mm (see Figs. 2.6A and B). The tarsal glands sandwiched between the layers of fibrocartilage in the upper eyelid exit on the eyelid margin near the eyelash follicles. The eyelashes are supported by their roots, attached to fibrous tissue on the tarsal plate, not in the orbicularis oculi muscle anterior to the tarsal plate. Laterally, the tarsal plate becomes a fibrous band that adjoins the structural counterpart from the lower eyelid, forming the lateral canthal tendon. Medially, the tarsal plate also becomes fibrous and shelters the superior lacrimal canaliculus behind as it becomes the medial canthal tendon.
TECHNIQUE
▶ Step 1. Protection of the Globe
During surgical procedures around the orbit, the cornea should be protected with a temporary tarsorrhaphy or scleral shell after application of a bland eye ointment.
▶ Step 2. Identification and Marking of Incision Line
If an eyelid crease is not readily detectable, a curvilinear incision along the area of the supratarsal fold that tails off laterally over the lateral orbital rim is made. Remarkably, the incision in the upper eyelid follows either the lower or the upper component of a standard blepharoplasty. In case of swelling, the opposite upper eyelid crease may be mirrored. The incision should be similar in location and shape to the lateral one third to one half of the superior incision in a blepharoplasty (see Fig. 5.2). The incision, however, may be extended farther laterally as necessary for surgical access. The incision should begin at least 10 mm superior to the upper eyelid margin and should be 6 mm above the lateral canthus as it extends laterally. The incision line is marked before infiltration of a vasoconstrictor to avoid distortion.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses