Introduction
The purposes of this retrospective study were to describe the types of unexpected complications associated with mandibular fixed retainers and to assess their prevalences and possible etiologic causes.
Methods
A total of 3500 consecutive patients (1423 male, 2077 female) treated with fixed appliances and a mandibular fixed retainer as a part of the retention protocol were screened during the retention period (2008-2013) for unexpected complications. Thirty-eight subjects (12 male, 26 female; mean age, 20.7 ± 8.9 years) with unexpected complications were identified and assigned to the unexpected complications group and compared with a randomly selected control group of 105 subjects (43 men, 62 women; mean age, 29.5 ± 9.7 years) without unexpected complications. Relationships between unexpected complications and cephalometric and clinical variables were evaluated.
Results
An opposite inclination of the contralateral canines (twist effect) was found in 21 subjects. In 89.5%, the left canines were tipped buccally. A torque difference of 2 adjacent incisors (X effect) was identified in 12 patients. In 5 subjects, nonspecific complications were noted. Subjects in the unexpected complications group were significantly younger at debonding ( P = 0.03) and had higher mandibular plane angles ( P <0.0001) and increased pretreatment ventral positions of the mandibular incisors ( P = 0.029). No differences were found between the groups with regard to treatment duration, wire type, failure rate, treatment changes in incisor proclination, or intercanine distance.
Conclusions
Unexpected complications of mandibular fixed retainers are relatively rare. Facial divergence was identified as a possible predictor. However, the etiology is most likely multifactorial. Strong asymmetry among the patients with the twist effect suggests that the mechanical properties of retention wires may play a role and should be examined in the future.
Highlights
- •
Prevalence and etiologic factors of unexpected complications of mandibular bonded retainers were examined.
- •
Three forms of unexpected complications were identified, but prevalence was low (1.1%).
- •
Strong asymmetry was found for canine inclination in the unexpected complications group.
- •
Patients with unexpected complications were compared with a control group without complications.
- •
Distribution of gingival biotypes was significantly different between the groups.
Long-term stability of orthodontic treatment results is a great challenge in orthodontics. Some authors even consider long-term stability to be a myth. To overcome this problem, others have advocated long-term or even lifelong retention as a solution. Fixed retainers seem to be the best option for long-term maintenance of treatment results, and a growing number of orthodontists use them for this purpose. Fixed retainers have been shown to be effective in maintaining an esthetic result in the anterior region without the patient’s compliance. They have been reported to be safe and predictable, and acceptable and compatible with periodontal health. However, regular checkups are required, since occasional failures caused by wire fractures or bond failures can occur. The reported failure rates of bonded retainers vary widely between 0.1% and 53%. According to some studies, long-term use of fixed retainers may also be associated with greater plaque and calculus accumulation, which can lead to a higher risk of gingival recession and increased probing depth.
Unexpected complications may also appear in patients with fixed retainers. These complications were described as unwanted movement of the teeth included in the fixed retainer, even without wire fracture or bond failure. Small spaces between incisors in intact retainer segments, unexpected torque changes between the maxillary central incisors, torque changes between adjacent mandibular incisors, and opposite inclinations of contralateral mandibular canines have also been reported. Unexpected complications have been estimated to occur in 0.1% to 5% of patients; these are relatively small numbers. However, 50% of these patients may require retreatment. In some, the complications can be quite severe, including buccal bone dehiscence. Consequently, gingival recessions may occur, posing both health and esthetic problems. In such cases, a demanding orthodontic and reconstructive surgical and periodontal treatment may be necessary.
Several causes of unexpected complications in patients with fixed retainers have been suggested, including poor bonding technique and insufficient wire passivity, instability of multistrand wires, and wire straightening or wire activation by mechanical trauma. Biologic factors, such as forces created by incisor position relapse, have also been proposed in the literature.
Apart from relapse, increased incisor proclination has also been shown to cause or worsen bone dehiscences of the buccal cortical plate, thus reducing bone support. With regard to bone support, it has been previously reported that hyperdivergent patients have a higher prevalence of buccal bone dehiscence and fenestrations in the mandibular anterior region even before orthodontic treatment.
We hypothesized that mandibular incisor proclination and increases in intercanine distance during orthodontic treatment may be associated with increased risks of unexpected complications. We also presumed that anatomic conditions related to an increased mandibular plane angle and hyperdivergence may play roles.
The purposes of this retrospective study were to describe the types, prevalence, and timing of unexpected complications of mandibular fixed retainers in a group of patients in the retention phase and to identify some possible etiologic factors that were previously suggested in the literature.
Material and methods
A cohort of 3500 consecutive patients (1423 male, 2077 female) fulfilled the following inclusion criteria: (1) mandibular bonded flexible spiral wire fixed retainer in situ; (2) pretreatment (T0) and posttreatment (T1) cephalometric and panoramic radiographs, plaster models, and intraoral photographs; (3) no prosthetic reconstruction in the mandibular anterior region; and (4) no history of periodontal treatment, surgery, or trauma in the mandibular anterior region. They were seen at regular retention visits from January 2, 2008, to November 29, 2013. All patients were of European descent and were treated for various malocclusions with fixed appliances in the private orthodontic practice of the second author (I.M.). They were treated with a 0.022-in slot Roth prescription preadjusted appliance (Ortho Organizers, Carlsbad, Calif). In the routine treatment protocol, initial leveling and alignment were performed with round, superelastic, or heat-activated nickel-titanium wires. Space closure was performed using rectangular 0.018 × 0.025-in stainless steel wires. Intramaxillary and intermaxillary elastics were also used during the final stages of treatment.
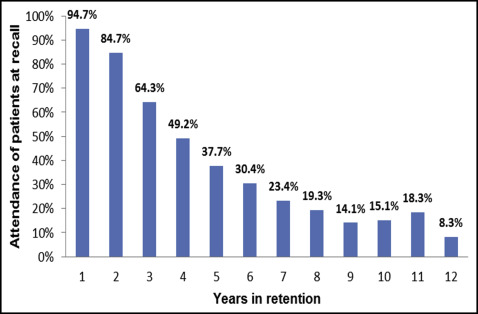
During debonding, all patients received a multistrand flexible spiral wire fixed retainer, either a 0.0215-in gold-plated 5-stranded spiral wire (Penta-One; Gold’n Braces, Palm Harbor, Fla) or a 0.0175-in 6-stranded coaxial wire (Ortho Organizers) bonded to the mandibular incisor region, including both canines and all incisors. All fixed retainers were shaped at chairside and bonded by 1 operator (I.M.) directly on the lingual surfaces of the mandibular anterior teeth using flowable composite (Transbond Supreme LV; 3M Unitek, Monrovia, Calif) according to the method described by Dahl and Zachrisson. In addition to a fixed retainer, the patients received removable maxillary and mandibular Hawley retainers or an activator and a maxillary vacuum-formed retainer. They were instructed to adhere to the standard retention protocol for removable retainers as follows: (1) full-time wear for 3 months, (2) nighttime wear only for the rest of the first year, (3) alternating nights for the second year, and (4) twice a week at night for the third year. The patients were also instructed to come at least once a year to have the fixed retainer checked even after they had stopped wearing the removable retainers. The average attendance of patients per year of retention in our study is shown in Figure 1 .
During the recall visit (T2), the patients were screened for unexpected complications of the mandibular fixed retainer. Written informed consent was obtained from each patient or the parents. The patients were examined, and intraoral photographs and plaster models were made. The prevalence and types of unexpected complications were determined by intraoral examination, and by evaluation and comparison of the study models obtained at T1 and at T2. Unexpected complications were assessed in the mandibular anterior region according to the descriptions reported previously : torque difference ( Fig 2 , A and B ) between 2 adjacent incisors (X effect), increased buccal inclination and opposite inclination ( Fig 2 , C and D ) of the contralateral canines (twist effect), and nonspecific changes such as spacing ( Fig 2 , E and F ).

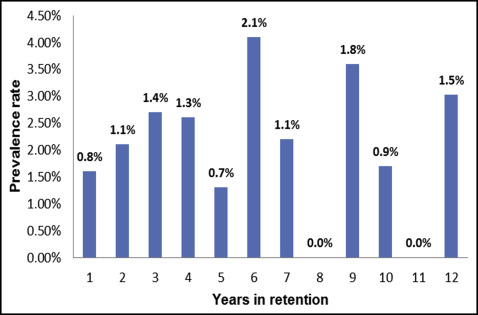
The subjects were divided into 2 groups according to the presence or absence of unexpected complications. The unexpected complications group (UCG) comprised 38 patients with a complication in the mandibular anterior segment. The distributions of unexpected complications among the patients by year in retention and the prevalence rates are shown in Table I and Figure 3 .
| Years in retention | UCG (n = 38) | Sample (n = 3500) |
|---|---|---|
| 0-1 | 6 | 710 |
| 1-2 | 7 | 645 |
| 2-3 | 7 | 496 |
| 3-4 | 5 | 381 |
| 4-5 | 2 | 283 |
| 5-6 | 5 | 234 |
| 6-7 | 2 | 177 |
| 7-8 | 0 | 144 |
| 8-9 | 2 | 112 |
| 9-10 | 1 | 113 |
| 10-11 | 0 | 138 |
| 11-12 | 1 | 67 |
Of the remaining patients, in whom no unexpected complications were identified, 105 patients were randomly selected to create the control group (CG). Random selection was performed with Excel (Microsoft, Redmond, Wash) using the Rand and Index functions. The sample size was calculated for inclination of the mandibular incisors at α = 0.05 and a power of 80% to detect a difference of 4°, assuming that the standard deviation was 7.4°. The power analysis showed that 105 patients were needed in the CG. The characteristics of both groups are shown in Table II .
| Variable | UCG (n = 38) | CG (n = 105) | P | ||
|---|---|---|---|---|---|
| F (%)/M (%) | 26 (68%)/12 (32%) | 61 (58%)/44 (42%) | 0.337 ∗ | ||
| TT (y) | 1.9 ± 0.7 | 2.0 ± 0.7 | 0.270 † | ||
| AD (y) | 16.7 ± 7.5 | 20.2 ± 9.5 | 0.030 † , ‡ | ||
| AR (y) | 20.7 ± 8.9 | 29.5 ± 9.7 | <0.0001 † , ‡ | ||
| RT (y) | 4.0 ± 2.8 | 9.3 ± 2.0 | <0.0001 † , ‡ | ||
| WT (%) | N 33 (87%) | AU 5 (13%) | N 92 (88%) | AU 13 (12%) | 1.000 ∗ |
| FR (%) | 13 (34.2%) | 43 (41.0%) | 0.562 ∗ | ||
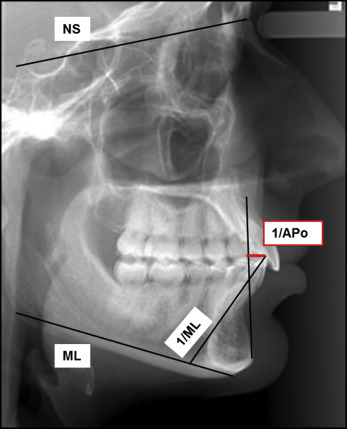
Each patient’s chart was analyzed to determine the type of retainer wire and rate of wire failure (wire fracture or detachment followed by repair of the fixed retainer), treatment duration (T0-T1), and retention time (T1-T2). Two lateral cephalometric radiographs and plaster models were analyzed of each subject from before treatment (T0) and after treatment (T1) to evaluate the treatment changes (T0-T1) in the inclination and position of mandibular incisors, the mandibular plane angle, and the intercanine distance. Cephalometric radiographs were digitized and traced using software (PC Dent: CompuGroup Medical, Prague, Czech Republic). Plaster model recording of intercanine distance change was performed using a digital caliper (Masel Orthodontics, Carlsbad, Calif), measured with an accuracy of 0.01 mm. The intercanine distance was measured from the middle of the cusp of the mandibular left canine to the middle of the cusp of the mandibular right canine. In the case of an abrasion of a cusp, the middle of the surface was estimated.
All tracings and evaluations were performed by the same operator (I.M.). A complete list of the variables with a detailed description and graphic representation of the cephalometric parameters is given in Figure 4 and Tables II and III .
| Variable | UCG (n = 38) | CG (n = 105) | P |
|---|---|---|---|
| 1/ML (°) | 93.6 ± 7.5 | 95.5 ± 7.5 | 0.151 |
| 1/APo (mm) | 2.9 ± 2.3 | 1.9 ± 2.9 | 0.029 ∗ |
| NSML (°) | 36.4 ± 5.2 | 31.4 ± 6.7 | <0.0001 ∗ |
| CC (mm) | 26.4 ± 1.9 | 25.6 ± 2.3 | 0.065 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


