div epub:type=”chapter” role=”doc-chapter”>
S. Nares (ed.)Advances in Periodontal Surgeryhttps://doi.org/10.1007/978-3-030-12310-9_2
2. Decision Trees in Periodontal Surgery: Resective Versus Regenerative Periodontal Surgery
Periodontal surgeryRegenerationGuided tissue regenerationMinimally invasive surgeryMagnificationBiomaterials
2.1 Introduction
For decades, clinicians and researchers have aimed to develop therapies to predictably regenerate periodontal structures and regain attachment lost due to periodontal disease. The advent of new surgical procedures, growth factors, and other biomimetic agents to complement existing bone replacement grafts has fundamentally changed the field of regenerative dentistry by increasing the long-term survival rate of teeth often categorized as having a poor prognosis. In the last decade, several new techniques have been demonstrated both preclinically and clinically, to further improve the success rate of periodontal regeneration.
2.2 Clinical Decision Considerations
Guided tissue regeneration (GTR) was formally introduced by Isidor et al. [1] where an occlusive membrane was utilized to allow only cells from the periodontal ligament to repopulate the root surface. The concept of cell occlusion and space provision prevented the gingival epithelium and connective tissue from entering the defect. Since then, the need for an occlusive membrane for defect isolation has been questioned by several authors, and the focus has shifted to the role of the undisturbed fibrin clot and wound stabilization between the tooth and gingival flap to prevent the downgrowth of epithelium [2, 3].
Based on current evidence, the predictability of GTR procedures has been shown to be influenced by several factors related to the defect site such as intrabony defect depth, angle, and configuration. According to Reynolds et al. [4], narrow defects less than 3 mm in width show a higher gain in attachment level, and bone fill suggesting defects which were shallow and wide would benefit more from osseous resective surgery. Indeed, several authors have consistently shown deep intrabony defects greater than 3 mm to have improved clinical outcomes using GTR compared to shallow defects [5, 6].
As our understanding of wound healing and periodontal regeneration has improved, a shift in treatment strategy from primarily one of cell occlusion to blood clot stability has occurred. Several minimally invasive surgical procedures have been introduced with the primary objectives of minimal flap reflection, wound stabilization, and establishing primary closure of the surgical flap(s). These approaches have demonstrated similar clinical outcomes irrespective of the defect configuration. The use of microsurgical instruments and microscopes has allowed for smaller surgical flaps with more predictable flap positioning, thereby stabilizing the blood clot and maintaining the integrity of the blood supply. With the help of these techniques and tools, a prognostic change has been reported whereby periodontally involved teeth with a hopeless prognosis show significant improvement and increased survivability after treatment.
Although there are many advantages to minimally invasive techniques such as improved patient comfort, reduced surgical trauma, improved wound stability, and primary closure of the flap, the main disadvantages lie in the added cost of the equipment and additional training required by the surgeon. Further, strict patent compliance and proper case selection are necessary with the application of these techniques primarily limited to localized and smaller interproximal defects with an intrabony component. The rationale of treatment utilizing these techniques is thus focused on regenerative approaches and less on resection of osseous tissues.
2.3 Systemic and Behavioral Factors
Patient-centered factors can have a significant impact on the success of regenerative therapy. Therefore, it is imperative that systemic and behavioral factors are carefully reviewed prior to initiating regenerative therapy as these factors can often relate to poor outcomes. It is well established that hyperglycemia, as occurs in poorly controlled diabetics, is associated with increased occurrence of infection and inflammation owing to impaired cellular immune responses and microcirculation during the wound healing process [7]. The combination of compromised wound healing and reduced bone turnover in the presence of hyperglycemia needs to be taken into consideration during treatment planning. Environmental factors such as smoking have also shown to have a negative impact on regeneration of new bone. Stavropoulos et al. [8] reported that smokers had a reduced gain in clinical attachment level following GTR as compared to non-smokers after 1 year. This finding is supported in a study by Tonetti et al. [9], who also showed the deleterious effects of smoking on the outcome of GTR. Matuliene [10] et al. in their study showed that teeth with probing depths of over 5 mm were at risk for loss and progression of periodontal disease. Therefore, supportive periodontal therapy such as routine maintenance care and good oral hygiene practices and behavior management are crucial to the long-term success of regenerative therapy.
In general, clinical advances in periodontics can be grouped into three main categories: tools, techniques, and materials. In this section we will describe advances in these categories.
2.4 Tools
2.4.1 Imaging
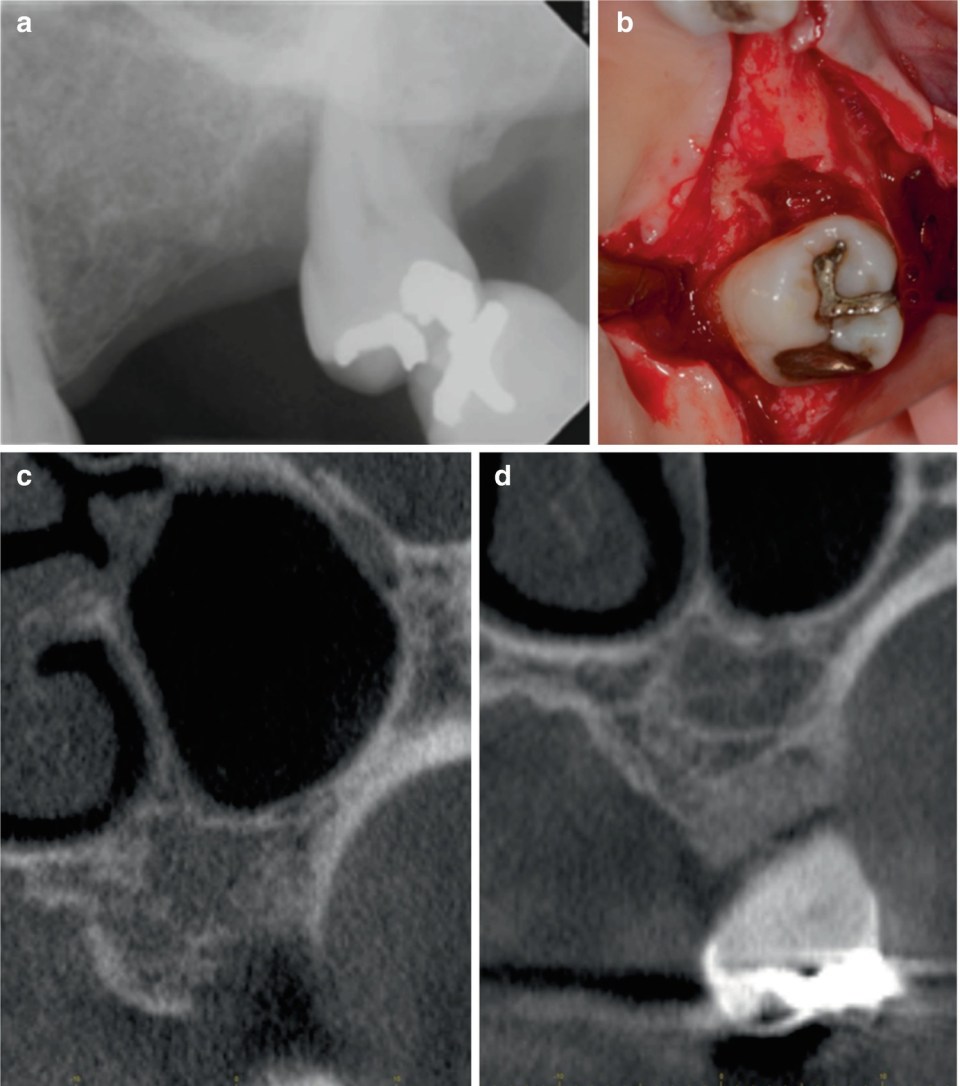
(a) Radiographic image of infrabony defect on the mesial of the maxillary left second molar. (b) Clinical photograph showing infrabony three-wall defect. (c) Presurgical CBCT image of defect. (d) Postsurgical CBCT image showing bone fill within the infrabony defect
2.4.2 Magnification

(a) Clinician using a microscope with ergonomic posture. (b) HD video camera mount attached to microscope (Global Surgical Corporation, St. Louis, MO, USA)
2.4.3 Instruments

Relative size of a No. 15 scalpel blade (top) and Mini 69 blade (middle) and Mini 63 blade (bottom) (Salvin Dental Specialties, Charlotte, NC, USA). The microblades are bendable up to 45° and have a full radius edge
2.5 Techniques
Significant advances in the treatment of periodontal disease, specifically in periodontal regenerative, have come in the way of development and refinement of microsurgical techniques. These techniques capitalize on progress in our understanding of wound healing, and the role of space maintenance, clot stabilization, and primary closure on tissue regeneration.
2.5.1 Minimally Invasive Techniques
Harrel and Rees were the first to propose the minimally invasive surgical (MIS) technique [33]. In this technique, thorough granulation tissue removal and root debridement were accomplished using minimal flap reflection and gentle manipulation of soft tissues. This technique was subsequently modified by the incorporation of microscopes and microsurgical instruments to improve surgical precision. In 2007, Cortellini and Tonetti [34] introduced the MIST (minimally invasive surgical technique) in combination with enamel matrix derivative (EMD) to treat isolated intrabony defects. In this approach, the intrabony defect was accessed using either a simplified papilla preservation flap in narrow interdental spaces or the modified papilla preservation flap in wide interdental spaces. The authors owed the success of this technique to clot stability and primary wound closure. In 2009, the same group proposed M-MIST, consisting of reflection of only the buccal papilla using buccal sulcular incisions connected by a horizontal incision close to the papilla tip to gain access to the interproximal defect in what they described as the “buccal window.” The authors described the same principles used for the previous technique, emphasizing the importance of space provision on success rates [35]. However, a major drawback to this technique is the lack of application to interproximal defects that extend buccally and/or lingually.
A recent retrospective study by Nibali et al. [4] showed significant improvements in intrabony defects by means of clinical attachment gains and radiographic bone fill using minimally invasive nonsurgical therapy (MINST). Following, supra- and subgingival debridement using thin piezoelectric devices and Gracey mini curettes under a magnification lens, an attempt was made to stimulate and stabilize a blood clot within the defect. One-year results from baseline showed a probing depth reduction of 3.5 mm and 2.8 mm for the buccal and lingual interproximal sites, respectively, with average attachment gains of 3.1 mm and 2.4 mm on the buccal and lingual interproximal aspects. In addition, a significant improvement in radiographic vertical defect depth from 6.74 mm to 3.8 mm and defect angle from 28.4 to 44.3° was noted. According to the author, the significant widening of the defect angle could be attributed to bone remodeling which occurs in addition to the formation of a long junctional epithelium following MINST. This minimally invasive, nonsurgical technique using microsurgical instruments reduced the risk of soft tissue trauma and may have a significant positive impact in the treatment of medically compromised patients or patients that are not good surgical candidates.

V-MIS procedure. (a) Arrow pointing to initial incision design. (b, c) Flap reflection showing granulation tissue within the infrabony defect visualized by the videoscope prior to instrumentation and following partial instrumentation. (d–f) Instrumentation within the defect using curettes and files to remove granulation tissue and calculus. (g) Arrow pointing to micro-islands of calculus present on the root surface. (h, i) Removal of the micro-islands of calculus using EDTA followed by flap closure using vertical mattress sutures

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


