Scissors bite is a rare form of malocclusion that is often accompanied by varying degrees of facial asymmetry. Transverse discrepancies in adults are very difficult to treat, especially in cases that also exhibit vertical overlapping of the posterior teeth. This case report illustrates the use of orthodontic mini-implants (OMIs) to treat a severe scissors bite in a middle-aged man. Absolute anchorage and lingual fixed appliances can successfully treat skeletal, dental and functional problems associated with scissors bite. Pretreatment, posttreatment, and retention records in this patient demonstrate effective and stable treatment results with few side effects.
Mild mandibular or facial asymmetry exists in all individuals. This “normal asymmetry” can be revealed most readily by comparing a full-face photograph with composites consisting of mirrored right or left sides. Sometimes asymmetries are associated with lateral occlusal problems and their most severe form, a scissors bite. Because of difficulties in correcting skeletal asymmetries and adjusting arch width after growth has ceased, in most cases the treatment of mandibular asymmetries in adults involves a combined orthodontic and surgical approach. For this reason, case reports of nonsurgical treatment of scissors bite in adult patients are rare.
Orthodontic mini-implants (OMIs) have become popular for absolute anchorage during various types of tooth movement because they are more convenient than conventional dental implants ; have favorable biomechanical properties ; can be placed at various anatomical locations, including the alveolar bone between the roots of teeth ; and are low cost. This case report describes the use of lingual fixed appliances and OMIs to resolve severe posterior scissors bite in an adult patient. This patient, a middle-aged man, had mandibular asymmetries, with deviation of the mandible to the right side complicated by a severe unilateral posterior scissors bite. Because his scissors bite was severe and accompanied by a significant amount of overeruption, conventional treatment mechanics could not offer a solution to his malocclusion.
Diagnosis and etiology
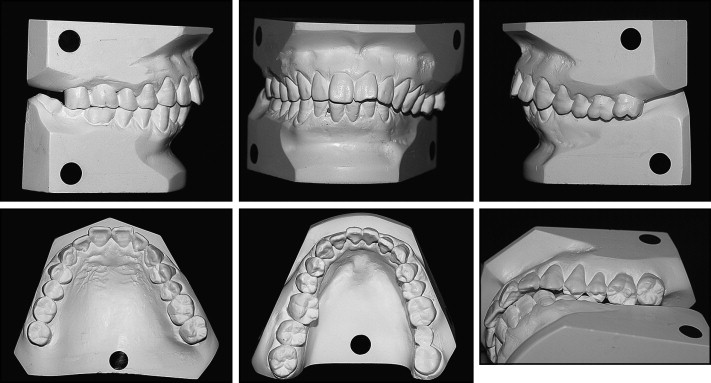
A healthy 49-year-old man was referred to my clinic in Seoul, Korea for orthodontic consultation. He had mild facial asymmetry, and his chief complaint was impaired occlusion due to a posterior scissors bite on his left side ( Fig 1 ). He was aware of his facial asymmetry and canting of the occlusal plane but was not concerned by those problems. Intraorally, his maxillary right first molar and mandibular right second molar were missing, and fixed bridges replaced these teeth. Generalized gingival recession was also present.

The mandibular midline was shifted slightly to the right. He had a Class II canine relationship on the right side with normal overjet and overbite. His maxillary left premolars and molars and mandibular left third molar were overerupted. Lingual cusps of the maxillary left posterior teeth and buccal cusps of the mandibular left posterior teeth showed a moderate degree of attrition ( Fig 2 ). Indentations due to occlusal contact could be seen on the buccal side of the mandibular left gingiva.
He did not have an unusual medical history or temporomandibular joint symptoms. The extraoral examination showed no limitation of movement during jaw opening. The functional shift of the mandible seemed to exert influence on his asymmetry. He had slight deviation of the path of jaw movement during closing and the buccal overjet of the right posterior teeth was nearly edge to edge.
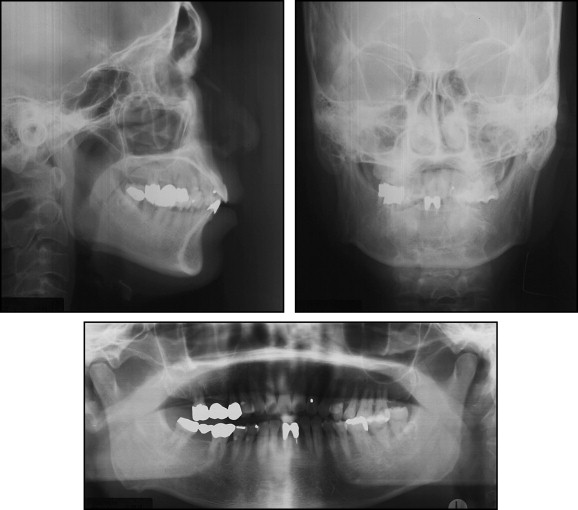
Panoramic and frontal cephalometric radiographs ( Fig 3 ) showed the asymmetric shape of the patient’s mandible. His maxillary right second premolar and second molar showed periapical radiolucency around the roots, and he felt pain in this area occasionally. The mandibular central incisors had root canal fillings and prosthetic work. Pretreatment facial photographs ( Fig 1 ) showed a straight and acceptable profile. The cephalometric analysis showed a slight skeletal Class II jaw relationship ( Table I ). This patient’s malocclusion was probably due to a combination of factors. Functional or prosthetic changes might have been complicating factors in addition to his genetic background.
| Pretreatment | Posttreatment | |
|---|---|---|
| Björk sum (°) | 391.7 | 392.5 |
| Facial height ratio (%) | 69.2 | 69.0 |
| ANB angle (°) | 8.8 | 8.8 |
| A to N perpendicular (mm) | 4.8 | 4.8 |
| Pog to N perpendicular (mm) | −11.5 | −12.7 |
| U1 to FH (°) | 109.0 | 104.6 |
| U1 to SN (°) | 102.6 | 97.2 |
| L1 to APog (°) | 7.8 | 5.2 |
| IMPA (°) | 109.7 | 105.7 |
| Interincisal angle (°) | 116.0 | 124.6 |
| Nasolabial angle (°) | 92.7 | 107.0 |
| UL to EL (mm) | 0.2 | −1.7 |
| LL to EL (mm) | −1.6 | −2.8 |
Treatment alternatives
The major problems needing to be resolved through treatment were intrusion of the overerupted maxillary premolars and molars and a maxillomandibular width discrepancy. Because of the difficulties of the case and the underlying skeletal problems, the first treatment option was a combination of orthognathic surgery and orthodontic treatment to address the mandibular and facial asymmetries. This approach would also address the mandibular constriction and the unilateral posterior scissors bite using a 3-piece Le Fort I surgery with mandibular symphyseal distraction. However, this option was rejected by the patient, who did not want an invasive procedure.
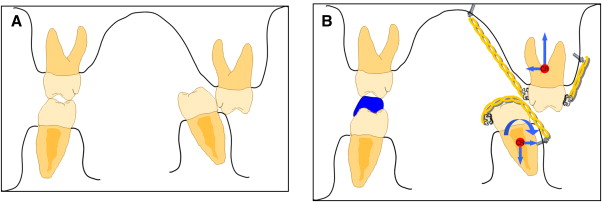
An alternative treatment plan was then presented. It consisted of using the OMIs to intrude and move inward the maxillary left posterior teeth and to intrude and straighten the mandibular left posterior teeth to an upright position. Extraction of the mandibular left third molar was recommended because of the absence of the opposing maxillary tooth.
The patient was eager to use an invisible lingual appliance during the entire treatment period. His malocclusion was very severe and the required teeth movements were complex. For easier treatment mechanics, I emphasized the necessity of brackets or buttons on the labial side of the posterior teeth.
Treatment progress
I placed 0.022-in preadjusted edgewise, ceramic brackets (Clarity, 3M Corporation, Unitek, Monrovia, Calif) on the labial side of the maxillary left posterior teeth and lingual brackets (0.018-in slot; Ormco Corporation, Glendora, Calif) were bonded on all of the mandibular left posterior teeth to improve alignment ( Fig 4 ). Some metal buttons were also placed in the required positions for intrusion. Titanium OMIs (1.6 mm in diameter, 5.0 mm in length; Ortholution Co., Seongnam-si, Gyeonggi-do, Korea) were placed into the palatal and buccal alveolar bone on the left side of the maxilla. One mini-implant was also placed into the buccal alveolar bone between the second premolar and first molar on the left side of the mandible. OMIs were placed, using local anesthesia, with a hand driver without drilling. After leveling using a 0.014-in nickel-titanium (NiTi) arch wire and a 0.016-in Australian arch wire, metal buttons were bonded on the palatal side of the maxillary left posterior teeth and an elastomeric module (Clear Generation II, Ormco Corporation, Glendora, CA) was used to intrude and pull inward the maxillary posterior teeth and to straighten to an upright position and intrude the mandibular posterior teeth ( Fig 5 ). To eliminate any premature occlusal contact between the palatal buttons and the mandibular teeth, resin cement (Transbond Plus, 3M Unitek, Monrovia, Calif) was built on the occlusal surfaces of the mandibular right posterior teeth.

After 6 months of treatment, the maxillary and mandibular left molars could be occluded with each other. The height of the resin bite plane was reduced gradually as the molar intrusion progressed.
After 8 months of treatment, lingual brackets were bonded on all of the maxillary and mandibular teeth, and round 0.014-in NiTi and 0.017 × 0.017-in copper-NiTi arch wires were used for leveling. An elastomeric module for intruding posterior teeth was changed at 3-week intervals.
After 1 year of treatment, the 2 mini-implants near the transpalatal suture area were removed because the patient complained that the elastomeric module interfered with his speech. The implant in the alveolar bone was left in place.
It took 18 months to achieve occlusal contact between the maxillary and mandibular right posterior teeth. The final occlusal adjustment and arch coordination was done with 0.016 × 0.022-in beta-titanium lingual arch wire.
During the course of treatment, the patient did not visit my clinic for 4 months because of a sudden business trip, so no adjustments could be made for a 4-month period.
At the finishing stage, I installed posterior intermaxillary elastics for occlusal seating on the right side, but the maxillary second premolar and molar became painful secondary to the periapical lesion observed at the beginning of the treatment. The referring dentist recommended that I not apply much force to those teeth. Therefore, an additional 2 OMIs were placed in the right maxillary buccal alveolar bone, and 0.022-in preadjusted edgewise metal brackets (Victory, 3M Unitek, Monrovia, Calif) were bonded to the right mandibular posterior teeth for the intermaxillary elastics (0.25-in, 2 oz, 3M Unitek, Monrovia, Calif) and for final adjustment of the occlusal interdigitation ( Fig 6 ).





