Introduction
Our objective was to quantify the treatment effects of microimplant-aided mechanics on group distal retraction of the posterior teeth.
Methods
The pretreatment and posttreatment cephalometric radiographs and dental casts of 23 patients (mean age, 22.1 ± 5.17 years), treated with distalization of the posterior teeth against microimplant anchorage and without extraction of the premolars or other teeth except the third molars, were used. The soft-tissue, skeletal, and dental measurements in the vertical and anteroposterior dimensions were analyzed. The changes in interpremolar and intermolar widths and rotations of the molars were analyzed with dental casts.
Results
The upper and lower lips were repositioned distally. The Frankfort horizontal to mandibular plane angle was decreased in the adult group. The maxillary posterior teeth were distalized by 1.4 to 2.0 mm with approximately 3.5° of distal tipping, and the mandibular posterior teeth were also distalized by 1.6 to 2.5 mm with approximately 6.6° to 8.3° of distal tipping. The maxillary posterior teeth showed intrusion by 1 mm. There were increases in arch widths at the premolars and molars. The overall success of microimplants was 89.7%; a well-experienced clinician had a higher success rate (98%) than did novices in this sample. The mean treatment time was 20 ± 4.9 months.
Conclusions
With microimplant-aided sliding mechanics, clinicians can distalize all posterior teeth together with less distal tipping. The technique seems effective and efficient to treat patients who have mild arch length discrepancy without extractions.
There have been many attempts to distalize molars with intraoral distalizing appliances. The side effects of these appliances are anchorage loss at the reactive part, flaring of the incisors, distal tipping, and rotation of the distalized molars.
To reduce these consequences, dental implants, miniscrews, and microscrews were tried. All of these skeletal devices can provide suitable anchorage. Miniscrews and microimplants, which have many advantages such as easy surgical placement and removal, low costs, and a small enough size to be placed into the interradicular bone between the roots of adjacent teeth, have achieved popularity over other skeletal anchorage devices. Dental implants and miniscrew implants are placed in the anterior or midpalate and connected to the premolars for applying distal force to the molars. Alternatively, the distalizing force is applied to the molars from skeletal anchorage devices. With skeletal anchorage, the side effects on the reactive part were alleviated, but distal tipping and rotation of distalizing molars are still issues. The 1-by-1 tooth movement is effective, but it tends to produce side effects of rotation and tipping movement when the force does not pass the center of resistance of a tooth.
Group distal retraction of the whole dentition with microimplants was introduced and showed several good treatment results. The distal force was applied to the canines or anterior hooks attached on the main archwire from microimplants placed between the roots of the posterior teeth. By moving teeth together, individual tooth movements, rotation, and tipping were prevented.
Several clinical case reports showed the efficacy of microimplants and the efficiency of the treatment mechanics in distalization of the whole dentition. However, only 1 pilot study evaluated the treatment effects of these mechanics with cephalometric analysis. Therefore, the purpose of this study was to quantify the treatment effects of en-masse retraction of the posterior teeth against microimplants by analyzing cephalometric radiographs and dental casts, and with clinical examinations.
Material and methods
The cephalometric radiographs and dental casts of 23 patients who had been treated with 0.022-in straight-wire brackets at the orthodontic department of Kyungpook National University Hospital in Korea were collected. Consecutively treated patients who received the microimplants for distal movement of the posterior teeth without extraction of the premolars or other teeth except the third molars and had a complete set of records were selected. The first step of treatment planning for all patients was setting the goal for the soft-tissue profile. The position of the anterior teeth was determined according to the ratio of soft-tissue change to the amount of anterior teeth retraction. After transferring the anteroposterior position of the anterior teeth to the occlusogram, all teeth were aligned from anterior to posterior. All patients required distal movement of the posterior teeth. The maxillary and mandibular posterior teeth with or without the anterior teeth were distalized to resolve crowding or improve the facial profile. The microimplants were placed between the roots of the posterior teeth. Microimplants were used for distalization of the maxillary or mandibular dentitions. Eighteen of the 23 patients had microimplants in both jaws. One patient had microimplants only in the maxilla, and 4 patients had microimplants only in the mandible. All patients were between the ages of 12 years 9 months and 31 years 7 months (mean, 22.1 ± 5.17 years). The descriptive data of the patients are given in Table I . Most patients had a moderate amount of arch length discrepancy, except 2 patients with anterior spacing and 2 with no arch length discrepancy. Four patients also required distal movement of the posterior teeth to improve their facial profile. All patients had erupted second molars in both arches at the beginning of treatment.
| Patient (sex) |
Age | Brand and type of microimplant (∮, diameter) |
Location of microimplant placement |
Duration of force application |
Failure (month after placement) |
Replacement (location, period of use) |
Pericoronitis on mandibular second molar |
Duration of treatment |
Microimplant treatment | ALD Mx/Mn (mm) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. (F) | 22 y 11 mo | Dentos AX 1311-107, -106 Dentos AN 12-106 |
#15-16 B, #25-26 B #36-37 B, #46-47 B |
17 mo, 17 mo 10 mo, 10 mo |
N | Operculum | 17 mo | Mx/Mn | −5.43/−4.45 | |
| 2. (M) | 24 y 4 mo | Dentos SH 1312-106 | #37 DB, #47 DB | 19 mo, 19 mo | Y (17 mo) | Y (2 mo) | Operculum | 20 mo | Mn | −10.73/−6.31 |
| 3. (F) | 28 y 3 mo | Osteomed (1.2 ∮,10 mm) Osteomed (1.2 ∮,6 mm) |
#37 DB, #47 DB #16-17 P, #26-27 P |
9.2 mo, 9.2 mo 9.2 mo, 9.2 mo |
N | 10 mo | Mx/Mn | −4.21/−4.74 | ||
| 4. (F) | 24 y 2 mo | Dentos AX 13-1065 Dentos AX 1311-107 |
#15-16 B, #25-26 B #36-37 B, #46-47 B |
14 mo, 14 mo 14 mo, 14 mo |
N | 15 mo | Mx/Mn | −3.50/−1.10 | ||
| 5. (F) | 26 y 9 mo | Dentos SH 1312-107, -110 Dentos SH 1312-106 |
#16-17 P, #26-27 P #36-37 B, #46-47 B |
11 mo, 11 mo 14 mo, 14 mo |
N | 14 mo | Mx/Mn | −0.75/−3.97 | ||
| 6. (F) | 15 y 3 mo | Osteomed (1.2 ∮,6 mm) | #37 DB, #47 DB | 16 mo, 16 mo | N | 16 mo | Mn | −10.16/−5.66 | ||
| 7. (M) | 23 y 1 mo | Dentos SH 1312-107 Dentos SH 1312-107 |
#15-16 B, #25-26 B #36-37 B, #46-47 B |
11 mo, 11 mo 11 mo, 11 mo |
Y (1 mo) | Y (8 mo) | 21 mo | Mx/Mn | 5.49/−1.78 | |
| 8. (F) | 29 y 3 mo | Dentos AX 1311-108 Dentos ATX 1311-105 |
#15-16 B, #25-26 B #36-37 B, #46-47 B |
21 mo, 21 mo 15 mo, 15 mo |
N | 23 mo | Mx/Mn | −4.46/−0.44 | ||
| 9. (F) | 18 y 11mo | Dentos ATX 1311-108 Dentos AX 12-106 |
#15-16 B, #25-26 B #37 DB, #47 DB |
20 mo, 22 mo 19 mo, 19 mo |
N | 22 mo | Mx/Mn | −3.13/0 | ||
| 10. (F) | 22 y 5 mo | Osteomed (1.2 ∮,6 mm) | #37 DB, #47 DB | 13 mo, 13 mo | N | 13 mo | Mn | −3.23/0 | ||
| 11. (M) | 31 y 7 mo | Dentos SH 1312-107 Dentos SH 1312-106 |
#15-16 B, #25-26 B #36-37 B, #46-47 B |
17 mo, 17 mo 17 mo, 17 mo |
20 mo | Mx/Mn | 0/−1.57 | |||
| 12. (F) | 21 y 1 mo | Dentos ATX 1311-108 Dentos AN 13-105 |
#15-16 B, #25-26 B #35-36 B, #45-46 B |
19 mo, 19 mo 19 mo, 19 mo |
N | 19 mo | Mx/Mn | −1.23/−1.23 | ||
| 13. (M) | 23 y 3 mo | Osteomed (1.2 ∮,6 mm) | #37 DB, #47 DB | 21 mo, 21 mo | N | 21 mo | Mn | 0/−1.49 | ||
| 14. (M) | 13 y 9 mo | Osteomed (1.2 ∮,6 mm) Dentos AN 12-204 |
#15-16 B, #25-26 B #37 DB, #47 DB |
17 mo, 17 mo 17 mo, 17 mo |
N | 17 mo | Mx/Mn | −5.36/−1.49 | ||
| 15. (M) | 16 y | Dentos SH 1312-107 Dentos SH 1311-106, Dentos SH 1412-105 |
#15-16 B, #25-26 B #36-37 B, #46-47 B |
13 mo, 13 mo 7 mo, 7 mo |
Y (1 mo) | Y (27 mo) | 28 mo | Mx/Mn | −7.19/−9.50 | |
| 16. (F) | 12 y 9 mo | Dentos SH 1312-107 Dentos SH 1312-106 |
#15-16 B, #25-26 B #36-37 B, #46-47 B |
18 mo, 21 mo 11 mo, 11 mo |
N | 30 mo | Mx/Mn | −1.43/−2.06 | ||
| 17. (F) | 20 y 9 mo | Dentos ATX 1311-107 Dentos AX 12-107 |
#15-16 B, #25-26 B #36-37 B, #46-47 B |
15 mo, 15 mo 14 mo, 14 mo |
Y (2 mo) | Y (12 mo) | 15 mo | Mx/Mn | −1.11/−1.41 | |
| 18. (F) | 21 y 1 mo | Dentos SH 1312-107 | #15-16 B, #25-26 B | 8 mo, 8 mo | N | 27 mo | Mx | −4.02/0 | ||
| 19. (F) | 26 y 3 mo | Dentos AX 1311-107 Dentos AX 1311-107 |
#15-16 B, #25-26 B #36-37 B, #46-47 B |
22 mo, 22 mo 15 mo, 19 mo |
N | Operculum | 22 mo | Mx/Mn | −1.46/−6.60 | |
| 20. (M) | 16 y 11 mo | Dentos SH 1311-107 Dentos AX 12-106 |
#15-16 B, #25-26 B #35-36 B, #45-46 B |
8 mo, 8 mo 23 mo, 23 mo |
N | 23 mo | Mx/Mn | −0.81/0.70 | ||
| 21. (M) | 13 y 3 mo | Dentos SH 1312-107 Dentos SH 1312-106 |
#15-16 B, #25-26 B #36-37 B, #46-47 B |
10 mo, 20 mo 13 mo, 13 mo |
N | Mild | 34 mo (2 phase) 21 mo (fixed) | Mx/Mn | −3.0/−4.0 | |
| 22. (F) | 26 y 11 mo | Dentos ATX 1311-107 Dentos AX 12-106 |
#16-17 P, #26-27 P #36-37 B, #46-47 B |
12 mo, 12 mo 13 mo, 13 mo |
Y (1, 7 mo) | Y (9, 6 mo) | Mild | 22 mo | Mx/Mn | −4.45/−2.3 |
| 23. (M) | 30 y 2 mo | Dentos ATX 1412-07 Dentos ATN 1312-05 |
#15-16 B, #25-26 B #36-37 B, #46-47 B |
25 mo, 25 mo 21 mo, 21 mo |
Y (2 mo) | Y (19 mo) | 25 mo | Mx/Mn | 3.06/0 |
We used 70 microimplants (Absoancho, Dentos, Daegu, Korea) and 12 surgical microscrews (Osteomed, Dallas, Tex). In the maxilla, 32 microimplants were placed in the buccal alveolar bone between the second premolars and the first molars. Six microimplants were placed in the palatal slope between the first and second molars in 3 patients who were treated with lingual brackets. In the mandible, 14 microimplants were placed into the bone distobuccally to the mandibular second molars, 26 into the alveolar bone between the mandibular first and second molars, and 4 into the alveolar bone between the mandibular second premolar and the first molar. Detailed surgical procedures have already been discussed.
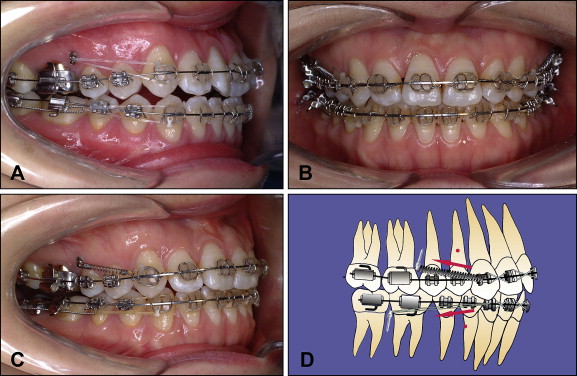
We used 0.022-in slot straight-wire brackets in all patients, and distalizing forces of approximately 200 g were applied from the maxillary and mandibular microimplants to the canines or premolars with nickel-titanium closing-coil springs or elastomeric threads (Super thread, Rocky Mountain Orthodontics, Denver, Colo) in the maxillary and mandibular arches ( Fig 1 ). After making space mesial to the canines by distalizing the buccal teeth, the anterior teeth were aligned. During the initial alignment, the anterior teeth were ligated loosely to prevent forward movement. The archwires used during distalization were initially rectangular beta-titanium alloy and were switched to 0.016 × 0.022-in stainless steel in the maxilla and 0.017 × 0.025-in stainless steel in the mandible. After anterior teeth alignment, the 6 anterior teeth were tied together, and the distalizing force was applied to the canines or to the short anterior hooks attached between the lateral incisors and the canines. The directions of the applied forces were backward and upward in the maxillary arch, and backward and downward in the mandibular arch.
All cephalograms were taken with the CX-90SP (Asahi, Kyoto, Japan) with 10% magnification. All pretreatment and posttreatment cephalograms were traced by 1 examiner (Y.-H.O.). The soft-tissue and skeletal measurements, dental angular measurements, and dental linear measurements are illustrated in Figures 2 through 4 .
When there was a double image, the midpoint between the 2 points was traced. The measurement points for the soft-tissue, skeletal, and maxillary dental linear and angular measurements were the same as used by Ghosh and Nanda. The centroid point, the midpoint on a horizontal line between the greatest mesial and distal convexity of the crowns, was used for dental linear measurements. To determine the amount of horizontal movement of maxillary teeth, the pterygoid vertical (PTV) plane was used. The vertical movement of the maxillary teeth was determined from superimposition on the palatal plane (PP). The horizontal movement of the mandibular teeth was determined by measuring and comparing the distance from the centroid point of the teeth to the mandibular lingual cortex (MLC), whereas the vertical measurements were determined from superimposition on the mandibular plane (MP). Angular changes of tooth positions were determined by the inclination of the long axes of the teeth to the sella-nasion plane (SN) in the maxillary arch and to the MP in the mandibular arch.
Arch length discrepancies and intermolar widths of the maxillary and mandibular arches that were distalized were measured before and after treatment on dental casts by using a digital caliper. The 3 lingual patients were removed from the sample when evaluating arch widths and rotation of the molars. To evaluate the rotation of the distalized molars, the transverse measurements were recorded between the buccal cusp tips of the maxillary and mandibular second premolars along with the mesiobuccal and distobuccal cusp tips of the first and second molars.
Statistical analysis
The statistical analyses were performed with SPSS software (version 14.0, SPSS, Chicago, Ill). A paired t test and a Wilcoxon signed rank test were used. When the sample showed normal distribution as evaluated by the Kolmogorov-Smirnov test, the P values of the paired t test were illustrated, unless the P values of the Wilcoxon signed rank test were illustrated.
Results
To calculate the error of measurements, 20 cephalometric films and models from 10 patients were retraced, redigitized, and remeasured 1 month later. Measurement errors were calculated based on the differences between the first and second values with a paired t test. There was no significant difference between the 2 measurements. To measure the range of methodologic errors, Dahlberg’s formula was used, and the results were 0.3° for angular measurements and 0.1 mm for linear measurements.
The mean distal repositionings of the upper and lower lips relative to the E-line were 0.72 and 1.18 mm, respectively. The lower lip moved distally more than the upper lip ( Table II ).
| Measurement | Pretreatment | Posttreatment | Change | Significance | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | t | W | |
| Soft tissue | ||||||||
| Upper lip to E-line (mm) | −1.22 | 2.19 | −1.94 | 1.91 | −0.72 | 1.29 | 0.014 ∗ | – |
| Lower lip to E-line (mm) | 1.17 | 2.78 | −0.01 | 1.93 | −1.18 | 1.42 | 0.001 † | – |
| Skeletal | – | |||||||
| SN-PP (°) | 9.26 | 3.68 | 9.50 | 3.82 | 0.24 | 1.31 | 0.391 | – |
| SN-OP (°) | 17.32 | 5.36 | 17.78 | 4.92 | 0.03 | 3.29 | 0.970 | – |
| FMA (°) | 26.00 | 5.23 | 25.30 | 5.05 | −0.70 | 1.25 | 0.014 ∗ | – |
| PTV-A (mm) | 48.99 | 2.59 | 48.93 | 2.74 | −0.07 | 1.43 | 0.829 | – |
| PTV-B (mm) | 50.30 | 4.83 | 49.77 | 4.45 | −0.53 | 2.01 | 0.223 | – |
| ANS-Me (mm) | 75.03 | 7.29 | 75.69 | 7.27 | 0.66 | 2.02 | 0.130 | – |
| Dental-angular (°) | ||||||||
| SN-U1 | 108.75 | 6.90 | 106.48 | 9.84 | −2.28 | 8.08 | 0.212 | – |
| SN-U4 | 85.91 | 6.52 | 81.72 | 6.18 | −4.19 | 7.18 | 0.015 ∗ | – |
| SN-U6 | 75.12 | 5.53 | 72.84 | 4.89 | −2.28 | 6.09 | 0.102 | – |
| SN-U7 | 65.17 | 11.93 | 65.97 | 9.32 | 0.80 | 7.04 | 0.617 | – |
| MP-L1 | 93.62 | 6.85 | 92.83 | 7.72 | −0.79 | 6.75 | 0.579 | – |
| MP-L4 | 82.61 | 5.42 | 77.52 | 7.65 | −5.09 | 9.40 | – | 0.004 † |
| MP-L6 | 80.53 | 4.78 | 73.35 | 9.44 | −7.18 | 8.12 | – | <0.0001 † |
| MP-L7 | 81.71 | 8.49 | 72.93 | 10.10 | −8.78 | 7.27 | – | <0.0001 † |
| Dental-linear (mm) | ||||||||
| PTV-U1 | 59.96 | 3.91 | 58.18 | 3.37 | −1.79 | 3.08 | 0.015 ∗ | – |
| PTV-U4 | 40.30 | 2.90 | 38.75 | 3.10 | −1.55 | 2.11 | 0.003 † | – |
| PTV-U6 | 23.33 | 3.12 | 21.59 | 3.36 | −1.75 | 2.01 | 0.001 † | – |
| PTV-U7 | 12.58 | 2.85 | 10.93 | 3.83 | −1.75 | 2.12 | 0.002 † | – |
| PP-U1 | 31.76 | 3.72 | 31.30 | 3.83 | −0.45 | 1.41 | 0.157 | – |
| PP-U4 | 25.43 | 3.06 | 25.07 | 2.88 | −0.36 | 1.18 | 0.174 | – |
| PP-U6 | 21.99 | 5.19 | 22.31 | 2.50 | 0.32 | 4.14 | – | 0.121 |
| PP-U7 | 19.67 | 3.28 | 19.46 | 2.65 | −0.22 | 2.54 | – | 0.111 |
| MLC-L4 | 5.00 | 3.13 | 6.80 | 3.88 | 1.80 | 1.89 | 0.0002 † | – |
| MLC-L6 | 21.60 | 2.64 | 24.19 | 3.32 | 2.58 | 2.10 | <0.0001 † | – |
| MLC-L7 | 33.94 | 3.18 | 35.78 | 3.47 | 1.84 | 1.99 | – | <0.0001 † |
| MP-L1 | 45.56 | 3.74 | 45.93 | 4.07 | 0.37 | 1.82 | 0.336 | – |
| MP-L4 | 37.59 | 4.07 | 38.35 | 4.22 | 0.76 | 1.89 | 0.066 | – |
| MP-L6 | 33.01 | 3.58 | 33.11 | 3.52 | 0.10 | 1.31 | 0.735 | – |
| MP-L7 | 30.35 | 3.26 | 29.61 | 3.61 | −0.74 | 1.29 | 0.013 ∗ | – |
The skeletal changes during treatment (before distalization to posttreatment) are summarized in Table II and showed that the Frankfort horizontal-mandibular plane angle (FMA) decreased with statistical significance. The other measurements were not statistically different. The distance of ANS-Me increased (0.66 mm), but it was not statistically significant. To preclude the effect of growth and to quantify the treatment effect only, the sample was divided into adult and growing groups. In the adults, the FMA decreased with statistical significance, and the distance of ANS-Me also decreased by –0.32 mm, although it was not statistically significant ( Table III ). In the growing patients, however, ANS-Me increased by 2.07 mm with statistical significance. In the adults, after the maxillary and mandibular dentitions were distalized, Points A and B moved posteriorly with statistical significance only for Point B ( Table III ).
| Measurement | Pretreatment | Posttreatment | Change | Significance | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | t | W | |
| Adult patients (n = 16) | ||||||||
| SN-PP (°) | 9.99 | 3.74 | 9.93 | 4.10 | −0.06 | 1.32 | 0.867 | – |
| SN-OP (°) | 17.42 | 5.58 | 17.37 | 5.03 | −0.05 | 3.30 | 0.952 | – |
| FMA (°) | 26.22 | 5.90 | 25.31 | 5.72 | −0.91 | 1.13 | 0.006 † | – |
| PTV-A (mm) | 49.02 | 2.64 | 48.63 | 2.77 | −0.39 | 1.15 | 0.193 | – |
| PTV-B (mm) | 50.93 | 4.67 | 49.84 | 4.59 | −1.09 | 1.52 | 0.0497 ∗ | – |
| ANS-Me (mm) | 75.51 | 8.45 | 75.20 | 8.00 | −0.32 | 1.91 | – | 0.222 |
| Growing patients (n = 7) | ||||||||
| SN-PP (°) | 7.57 | 3.16 | 8.50 | 3.13 | 0.93 | 1.07 | 0.061 | – |
| SN-OP (°) | 18.21 | 5.15 | 18.71 | 4.91 | 0.20 | 3.53 | 0.886 | – |
| FMA (°) | 25.51 | 3.61 | 25.30 | 3.41 | −0.21 | 1.48 | 0.716 | – |
| PTV-A (mm) | 48.93 | 2.66 | 49.61 | 2.75 | 0.69 | 1.80 | 0.352 | – |
| PTV-B (mm) | 48.86 | 5.24 | 49.61 | 4.45 | 0.76 | 2.50 | 0.454 | – |
| ANS-Me (mm) | 75.03 | 6.57 | 77.10 | 7.16 | 2.07 | 1.40 | 0.008 † | – |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


