Temporomandibular joint ankylosis manifests a range of clinical characteristics dependent upon the age of onset, the affected side, and the severity. When it occurs during development, mandibular growth is affected, resulting in severe retrusion or asymmetry as well as limitation of mandibular movements. Progressive asymmetric mandibular growth in unilateral ankylosis causes canting of the occlusal plane. In this case report, we present a successful temporomandibular joint reconstruction using transport distraction osteogenesis combined with camouflage orthodontic treatment for occlusal canting correction of a patient with unilateral temporomandibular joint ankylosis and severe facial asymmetry.
Highlights
- •
Unilateral TMJ ankylosis during growth results in functional and esthetic problems.
- •
Balance and timing between surgery and camouflage are important.
- •
Gap arthroplasty and active physiotherapy are crucial for functional TMJ restoration.
- •
Transport distraction osteogenesis is a choice to reconstruct the TMJ and correct asymmetry.
- •
Maxillary canting was corrected with skeletal anchorage without additional surgeries.
Temporomandibular joint (TMJ) ankylosis indicates a fibrotic or skeletal adhesion between the condylar fossa and the condylar head or disc. The etiology varies from congenital factors to infection, trauma, failed previous surgery, or prolonged static loading. It causes limitation of mandibular function, micrognathia, or facial asymmetry, depending on the onset of the disease and the severity of involvement.
Treatment objectives for unilateral TMJ ankylosis with severe asymmetry are restoration of functional mandibular movements and esthetic improvement. Separation of the fused condyle from the temporal area (gap arthroplasty) and condylar reconstruction are fundamentally required. Variable options for TMJ reconstruction include autogenous bone graft, alloplastic replacement, and distraction osteogenesis (DO).
Of these, the DO procedure extends the length of bone in conjunction with adjacent soft tissues using a distractor in a specific location. Transport DO refers to movement of a segment of bone from the host bone, guided by an appliance to the defect site. Extension of the ramus through transport DO by cutting the bone in an L shape on the condylar area is often used for TMJ reconstruction. In patients with severe facial asymmetry, excessive mandibular advancement at the deviated side is required during surgery, making DO (which increases the likelihood of both osteogenesis and histogenesis) a viable option.
Here, we describe a treatment process and its successful outcome with long-term stability in a patient with unilateral TMJ ankylosis and facial asymmetry. The patient underwent transport DO for TMJ reconstruction and skeletal asymmetry correction without additional orthognathic surgery, instead of camouflage orthodontic treatment for occlusal canting and anteroposterior discrepancy correction.
Diagnosis and etiology
A 15-year-old girl came to the Yonsei University Dental Hospital in Seoul, Korea, with a history of a partial condylectomy and a costochondral graft for TMJ reconstruction in another hospital at the age of 13. Her chief complaints were severe facial asymmetry and limited mouth opening. Her maximum mouth opening was 15.0 mm, and deflection to the left during mouth opening and protrusive movement were observed. The amount of lateral movement to the left was 4.0 mm, but it was less than 1.0 mm to the right.
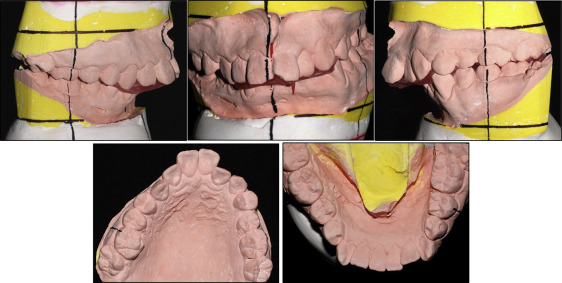
Facial analysis showed a 15.0-mm deviation of the chin from the facial midline toward the left side, severely canted lip, and chin retrusion. The mandibular dental midline was deviated to the left by 8.0 mm, and a posterior lingual crossbite was present on the right side, with asymmetric arch shapes of both maxillary and mandibular arches. She had Angle Class II canine and molar relationships with overjet of 11.0 mm and overbite of 5.0 mm ( Figs 1 and 2 ).

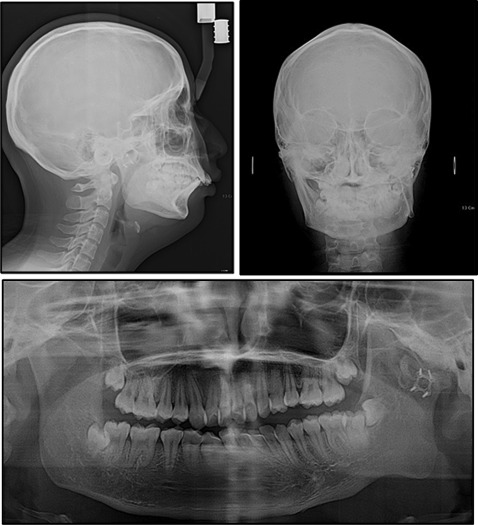
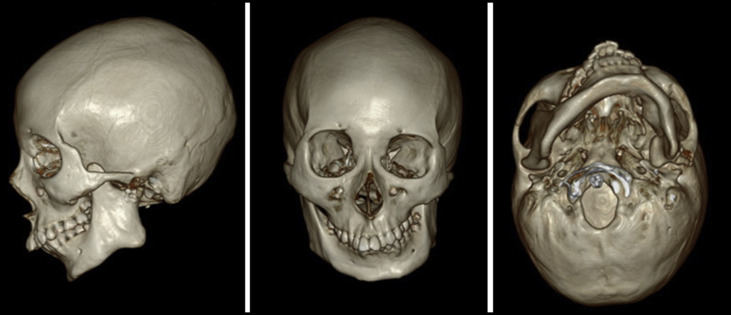
Evaluation of the panoramic radiograph showed deficiencies of the left condyle and ramus compared with the right side, with an ankylosed hard tissue mass in the left TMJ area. Overgrowth of the coronoid process on both sides was observed. Three- dimensional (3D) facial computed tomography (CT) and cephalometric analysis showed that menton was deviated from the skeletal midline by 16.5 mm, and the cant of the maxillary occlusal plane was inclined downward to the right by about 6.0 mm. The difference in the right and left ramal heights was 20.0 mm, and the difference in the mandibular body lengths was 12.0 mm. The analyses also showed a significantly retruded mandible (SNA angle, 80.1°; SNB angle, 67.8°), indicating a skeletal Class II malocclusion (ANB angle, 12.3°). A hyperdivergent facial profile was evident, with a high mandibular plane angle. The incisors were inclined labially with an angle of the maxillary incisors to the Frankfort horizontal plane of 125° and an IMPA of 120° ( Figs 3 and 4 ; Table ).
| Measurement | Norm | Pretreatment | Presurgery | Postsurgery |
|---|---|---|---|---|
| Skeletal | ||||
| SNA (°) | 81.6 ± 3.1 | 80.1 | 78.9 | 79.1 |
| SNB (°) | 78.9 ± 3.0 | 67.8 | 67.5 | 73.1 |
| ANB (°) | 2.4 ± 1.8 | 12.3 | 11.4 | 6.0 |
| SN-GoGn (°) | 34.3 ± 5.3 | 35.6 | 35.8 | 37.1 |
| Ramus height (mm), R/L | 51.0 ± 4.1 | 60.4/40.8 | 60.4/40.8 | 60.4/50.2 |
| Go-Me (mm), R/L | 72.0 ± 4.0 | 73.6/61.7 | 73.6/61.7 | 73.6/67.5 |
| Dental factors | ||||
| U1 to facial plane (mm) | 9.0 ± 3.0 | 22.3 | 14.8 | 10.7 |
| L1 to facial plane (mm) | 5.7 ± 2.7 | 11.5 | 7.8 | 7.6 |
| Soft tissues | ||||
| Upper lip to E-line (mm) | 1.0 ± 2.0 | 4.3 | 0.6 | −0.8 |
| Lower lip to E-line (mm) | 2.0 ± 2.0 | 3.9 | 0.4 | 2.4 |
The final diagnosis was TMJ ankylosis on the left side and mandibular retrusion with severe asymmetry.
We collected preoperative CT and magnetic resonance images and medical records from the previous surgeon. This patient had had a severely malformed left condyle and a hyperplastic coronoid process on both sides. A partial condylectomy with a costochondral bone graft was done for TMJ reconstruction. It was evident that the etiology of the unilateral TMJ ankylosis was due to the previous autogenous bone graft and that the severe facial asymmetry with the hyperdivergent profile had occurred during growth and was worsened by the ankylosis.
Treatment objectives
The treatment objectives were to (1) improve mandibular function, (2) reconstruct the affected TMJ, (3) restore facial esthetics including correction of asymmetry and mandibular retrusion, and (4) establish proper occlusion.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


