Introduction
Agenesis of a maxillary lateral incisor occurs in about 2% of the population. Treatment options should adapt to natural biologic changes in a lifelong perspective.
Methods and results
A young woman with bilateral agenesis of the maxillary lateral incisors was treated with transplantation of a developing maxillary third molar on one side and a dental implant on the contralateral side, after orthodontic space opening. The periodontal examination, including bacterial testing of the transplant, the implant, and the control central incisor, was performed 9 years after the treatment. A radiologic assessment was also performed. The transplanted tooth did not differ from a natural incisor, except for the pulp obliteration, and the total bacteria count was higher at the implant site. The periodontal tissues around the implant showed progressive signs of recession.
Conclusions
Both tooth transplants and dental implants for replacing missing maxillary incisors can be effective in the long term. This report supports natural tooth substitution rather than implant placement for dental agenesis in the anterior maxilla.
Highlights
- •
Long-term success after application of a dental implant and a tooth transplant is possible in the anterior maxilla.
- •
Favorable periodontal status of a transplanted wisdom tooth to replace an upper lateral incisor was documented.
- •
Natural tooth substitutions are recommended in the anterior maxilla whenever possible.
Agenesis of a maxillary lateral incisor is the second most common tooth agenesis, excluding third molars, and occurs in 1.55% to 1.78% of the population, with a higher incidence of bilateral agenesis. The treatment options for replacement of congenitally missing maxillary incisors include dental implants, canine substitution usually after orthodontic space closure, and tooth-supported restorations. The patient’s age, dentofacial morphology, profile, crowding, and preferences determine the treatment decisions, which have lifelong consequences.
Dental implants have been reported to favorably substitute for congenitally missing maxillary lateral incisors ; recently, implants with narrow diameters or custom-made abutments were introduced to fulfill the anatomic and esthetic demands. Autotransplantation of developing teeth is also documented as a predictable treatment modality for missing teeth, including missing maxillary incisors. However, no articles in the literature have compared the effectiveness of tooth transplantation and dental implants when replacing missing maxillary incisors. This report is the first to document the long-term outcome after transplantation of a developing third molar and the use of a dental implant to substitute for both congenitally missing lateral incisors in the same patient.
Case description
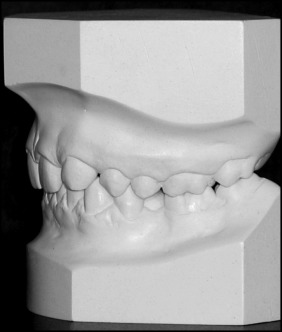
In 2001, a 19-year-old woman sought orthodontic treatment because she was dissatisfied with the esthetics of her smile; her complaint was related primarily to the congenital absence of both maxillary lateral incisors ( Figs 1 and 2 ). The clinical examination and the analysis of study models showed spacing in the anterior maxilla, a Class I molar relationship on the right side, a Class II molar relationship on the left side ( Fig 3 ), and a 3-mm maxillary midline shift to the right side. We also recorded Class IB according to the Palacci-Ericson classifications of the vertical dimensions of tissue loss (Class I, intact or slightly reduced papillae; Class II, limited loss of papillae [less than 50%]; Class III, severe loss of papillae; and Class IV, absence of papillae [edentulous ridge]) and the horizontal dimensions of tissue loss (Class A, intact or slightly reduced buccal tissues; Class B, limited loss of buccal tissues; Class C, severe loss of buccal tissues; and Class D, extreme loss of buccal tissue).


The initial panoramic radiograph confirmed agenesis of both maxillary lateral incisors and also impacted third molars ( Fig 4 ). There were no signs of hard tissue pathology. The patient was dissatisfied with her maxillary canines while smiling. Therefore, she refused orthodontic space closure and canine substitution treatment after a discussion of the possible treatment options. The orthodontic treatment plan included orthodontic space opening after extractions of the maxillary second premolars to create a space for dental implants at the positions of the missing incisors. Since the panoramic radiograph showed a small maxillary third molar, it was decided to transplant this tooth to replace 1 lateral incisor ( Fig 4 ). The third molar was unerupted, and its root development was not completed; this was favorable for tooth transplantation. In addition, the morphology of the donor tooth, which was small and single-rooted, was favorable for a substituted lateral incisor. Therefore, the final surgical treatment plan included autotransplantation of the developing maxillary left third molar and a narrow platform implant to replace the missing maxillary lateral incisors. Informed consent was obtained before the treatment.

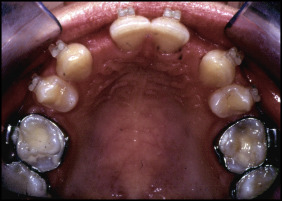
Eighteen months after start of the orthodontic treatment, adequate space was created to accommodate the replacements at the sites of the missing teeth ( Figs 5 and 6 ). The root development of the maxillary left third molar was still not completed, and the tooth was considered suitable to be autotransplanted to the position of the maxillary right lateral incisor.

Surgical procedures
The autotransplantation of the developing maxillary third molar to replace the maxillary right lateral incisor was performed in May 2004. The surgery started with a gentle surgical exposure of the unerupted third molar to prevent injury to the periodontal ligament and Hertwig‘s epithelial root sheath. A mucoperiosteal flap was raised at the recipient site using a horizontal intrasulcular incision on the right side in the anterior maxilla. The artificial socket was prepared with a surgical conical bur (HM 75060; Meisinger, Neuss, Germany), which resembled the shape of the root of the transplanted tooth. The graft was immediately transferred to the prepared recipient site with its crown above the gingival level, and stabilization of the orthodontic wire (0.0195-in rounded coaxial stainless steel wire) with low-viscosity composite resin (a flow composite) was continued for 2 weeks, until removal of the sutures.
In July 2004, a dental implant (Replace Select Narrow Platform, 3.5 mm diameter, 13 mm length; Nobel Biocare, Kloten, Switzerland) was inserted in the position of the missing left lateral incisor according to the manufacturer’s protocol. The implant was positioned slightly more palatally to reduce the risk of buccal bone resorption and to favor the labial soft tissue thickness. After 6 months, the healing abutment was installed with the papilla-like soft tissue reconstructing technique described by Palacci and Nowzari to increase the soft tissue volume at the buccal side of the implant. Two months later, a porcelain crown was cemented on the implant ( Fig 7 ), and a few days later the transplanted tooth received a temporary composite buildup. At that time, the transplanted molar showed a normal reaction of the pulp to electric pulp testing. A zirconium crown finally replaced the composite buildup on the transplanted molar after 5 years because of the patient’s esthetic demands and a slight gingival inflammation, which was probably related to the composite restoration.

After the treatment, the patient was examined every year. The final examination was 9 years after the surgery ( Figs 8 and 9 ).


Results
Measurements of pocket depths, clinical attachment levels, gingival recession, bleeding on probing, width of the keratinized gingiva, and the papilla index were made on all tooth surfaces. Periodontal charting of the 6 maxillary anterior teeth and the results of the bacterial testing (PET Plus Kit; MIP Pharma, Blieskastel-Niederwürzbach, Germany) at the sites of the transplant, the implant, and the control incisor are included in the Table . No clinical symptoms of inflammation (bleeding, redness, deep pockets) at any location were seen. The transplanted molar had normal mobility and a low percussion sound, which indicated absence of ankylosis. A bluish color was visible through the soft tissues above the implant crown at the position of the maxillary left lateral incisor that was not present at the end of the treatment. The change in the color of the gingiva above the implant was noticed approximately 2 years after treatment. The marginal gingival contour at the implant site was positioned more apically in comparison with the adjacent teeth with a slightly narrower keratinized gingiva, which did not change after treatment. The papillae normally filled the interdental spaces (papilla index score, 3) ( Fig 3 ). The periodontal statuses of the transplanted molar and the implant did not significantly differ from those of the natural incisors, except for higher probing depths for the implant. Bacterial DNA testing from the gingival crevicular fluid using real-time polymerase chain reaction at the transplanted tooth, the implant, and the control maxillary right central incisor was performed. The real-time polymerase chain reaction tests are based on the ability of DNA polymerase to synthesize new strands of DNA complementary to the offered template strand; this allows identification of specific microorganisms. The polymerase chain reaction assay was used for the identification of 9 periopathogens ( Aggregatibacter actinomycetemcomitans , Porphyromonas gingivalis , Treponema denticola , Tannerella forsythia , Prevotella intermedia , Peptostreptococcus micros , Fusobacterium nucleatum , Eubacterium nodatum , and Capnocytophaga gingivalis ). A thin paper probe was placed under the gum line for 10 seconds according to the manufacturer’s instructions. When removed from the mouth, the probe was placed in a small container and sent to the laboratory for bacterial testing. The reaction mixture contained primers, magnesium chloride, and Taq polymerase, to which evaluated DNA was added. The reaction was performed in a thermocycler. The level of bacteria detection was set at 10 2 . The total bacteria count was 10 times higher at the implant site than at the transplant and control sites. Low numbers of green and orange bacteria complexes ( C gingivalis and P micros ) were detected at the implant sulcus (1.1 × 10 4 and 4.7 × 10 2 , respectively). The green and orange bacteria complexes were not found at the transplant and natural incisor sites.



