Introduction
Patients undergoing orthodontic treatment are at greater risk for developing white spot lesions (WSLs). Although prevention is always the goal, WSLs continue to be a common sequela. For this reason, understanding the patterns of WSL improvement, if any, has great importance. Previous studies have shown that some lesions exhibit significant improvement, whereas others have limited or no improvement. Our aim was to identify specific patient-related and tooth-related factors that are most predictive of improvement with treatment.
Methods
Patients aged 12 to 20 years with at least 1 WSL that developed during orthodontic treatment were recruited from private dental and orthodontic offices. They had their fixed appliances removed 2 months or less before enrollment. Photographs were taken at enrollment and 8 weeks later. Paired photographs of the maxillary incisors, taken at each time point, were blindly assessed for changes in surface area and appearance at the individual tooth level using visual inspection.
Results
One hundred one subjects were included in this study. Patient age, brushing frequency, and greater percentage of surface area affected were associated with increased improvement. Central incisors exhibited greater improvements than lateral incisors. Longer time since appliance removal and longer length of orthodontic treatment were associated with decreased levels of improvement. Sex, oral hygiene status, retainer type, location of the lesion (gingival, middle, incisal), staining, and lesion diffuseness were not found to be predictive of improvement.
Conclusions
Of the various patient-related and tooth-related factors examined, age, time since appliance removal, length of orthodontic treatment, tooth type (central or lateral incisor), WSL surface area, and brushing frequency had significant associations with WSL improvement.
Highlights
- •
White spot lesions (WSLs) are a common sequela of orthodontic treatment.
- •
WSLs seem to improve in the months after orthodontic appliances are removed.
- •
Predicting the amount of improvement is challenging.
- •
Time since appliance removal may be an important predictive factor.
- •
Factors such as depth of lesion or patient’s diet might influence the improvement.
Orthodontic treatment has long served as a means for providing patients with improved esthetic, functional, and psychological benefits. Unfortunately, white spot lesions (WSLs) are a common and undesirable side effect that can diminish the satisfaction that a patient experiences after orthodontic treatment. Some studies have shown that the prevalence of WSLs is as high as 97% among orthodontic populations.
WSLs are characterized by their greater opacity than healthy enamel. They have a whiter appearance as a result of mineral loss in the surface layers; this alters the refractory index and increases the scattering of light in the affected area because of damaged surface roughness. The appearance of the lesion can vary from minor surface change to cavitation. In some instances, stains can be incorporated into a lesion and lead to the formation of brown spots during the remineralization process, worsening the esthetic problem. Prevention and treatment of WSLs are important for the integrity of the teeth, as well as for esthetics, since they often affect the maxillary incisors.
Several options have been proposed to address these lesions, depending on their nature and severity. The recommended treatments range from as simple as improved home care with fluoride toothpaste to more invasive options involving composite restorations. There is still a lack of strong evidence in the literature, however, regarding the most effective treatment protocol and the ideal timing for maximizing improvement.
In addition to the abundance of available treatment options, the unpredictable patterns and degrees of improvement add to the complexity of WSL treatment. There is a wide range of improvement in lesions from one patient to the next. Lesions can vary in size, shape, and location and are as unique as the oral environment of the patients in whom they are found. Results from a previous randomized control trial by Huang et al found no significant differences in subjective or objective improvement in the appearance of the WSLs among those who received MI Paste Plus, PreviDent fluoride varnish, or normal home care during an 8-week period. Although some WSLs exhibited little or no improvement, some did show considerable improvement. Since the treatment arm did not appear to have a large role in the improvement of WSLs, investigation of other possible factors associated with WSL improvement seemed warranted.
The first aim of this study was to determine whether the following patient factors are predictive of the overall improvement of WSLs: age, sex, time since appliance removal, length of orthodontic treatment, self-reported tooth brushing, oral hygiene, or retainer type. Each patient factor was analyzed with the null hypothesis of no difference in WSL improvement for both subjective and objective measures.
The second aim was to compare the following tooth-related factors with the amount of WSL improvement: proportion of tooth surface area affected, tooth type (central or lateral incisor), staining, location (gingival, middle, incisal), and lesion diffuseness. The null hypothesis was that there would be no difference in WSL improvement associated with the tooth-related factors.
Material and methods
This study is a further investigation of data from a previous project regarding WSLs. The photographs that formed the sample data were originally collected from a randomized (1:1:1), single-blind, active-controlled, parallel-group trial evaluating the improvement of WSLs in 3 treatment arms. The treatment arms were MI Paste Plus (GC America, Allsip, Ill), containing casein phosphopeptide-amorphous calcium phosphate and 900 ppm of fluoride; PreviDent fluoride varnish (22,600 ppm of fluoride; Colgate Oral Pharmaceuticals, New York, NY); and a home-care control group with oral hygiene instructions and over-the-counter toothpaste (1100 ppm of fluoride; Colgate Oral Pharmaceuticals). In the original study, photographs of the WSLs were taken at 2 times: the start of the study (T1) and 8 weeks later (T2). Data were collected from private orthodontic and general dentistry offices belonging to the Practice-based Research Collaborative in Evidence-based Dentistry network in the Northwestern United States (Northwest PRECEDENT). The network was co-operated by the University of Washington and the Oregon Health and Science University, and it comprised Washington, Oregon, Montana, Idaho, and Utah.
Eligibility criteria for this study included the fulfillment of the following conditions: completion of fixed appliance orthodontic therapy within the past 2 months, at least 1 WSL on the facial surface of a maxillary incisor that was not present before starting orthodontic treatment, and age between 12 and 20 years. Subjects excluded from this study were those who were unwilling to be randomly assigned to 1 of the 3 treatment groups; had any abnormal oral, medical, or mental conditions; received therapy for WSLs after orthodontic treatment; displayed frank cavitations associated with the maxillary incisors; or were unable to speak or read English. Patients (and parents, for those under 18 years of age) consented to participate before the study.
Throughout treatment, oral hygiene was reinforced by staff members. Clinicians provided patient information, including age, sex, length of orthodontic treatment, and retainer type. All subjects also completed a questionnaire, which gave us information regarding their average daily brushing frequency.
Two types of evaluations (subjective and objective improvement) were performed for the 4 maxillary incisors, for each pair of photographs (initial and 8 weeks). For subjective improvement, a blinded panel of 5 dental professionals (expert panel) assessed improvement using a visual analog scale from 0 to 100 mm (0 mm, no improvement or worsened, to 100 mm, complete resolution). These evaluations were performed as part of the original study, and the mean ratings of the panel were used for overall improvement of the 4 maxillary incisors.
For objective improvement, 2 examiners (a dental student and a general dentist) performed the assessments for improvement by measuring changes in WSL surface area at each time point. WSL surface area was divided by total tooth surface area to calculate the pretreatment and posttreatment percentages of affected surface areas. The change in percentage of affected surface area was obtained by subtracting the T2 surface area from the T1 surface area. These assessments were also performed as part of the original study for all 4 incisors.
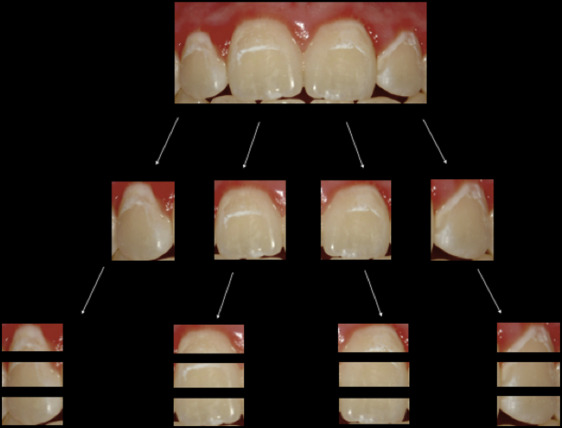
For this current study, we considered improvement of a lesion to be a visible decrease in the affected surface area, minimized contrast between the WSL and surrounding healthy tooth structure, or any combination of changes resulting in an overall improved esthetic appearance. In the previous study, all 4 incisors were evaluated as a unit, rather than each tooth individually ( Table I ). To perform evaluations at the single-tooth level, we cropped the images of the 4 maxillary incisors into individual teeth (n = 404) and then further cropped them into horizontal thirds, evaluating only the portions affected (n = 728) ( Fig 1 ). To maintain a uniform size and a similar level of magnification, a grid of a fixed dimension was used to show only the tooth or portion of the tooth being evaluated. This method allowed us to mask all other teeth or parts of teeth, minimizing any undesired influence from the surrounding teeth on the evaluation scores. Once all images were cropped to the proper dimensions, the lesions were then categorized according to the different characteristics that were of interest to this study.
| Evaluation level | Evaluation type | Outcome measure | Factors evaluated |
|---|---|---|---|
| 4 maxillary incisors | Subjective improvement Objective improvement |
Visual improvement (%) Reduction of surface area (%) |
Age Sex Time since deband Treatment time Brushing frequency Oral hygiene Retainer type Initial WSL surface area |
| Single tooth | Improvement scale | 1: Significantly worse 2: Slightly worse 3: Same 4: Slightly better 5: Significantly better |
Age Sex Time since deband Treatment time Brushing frequency Oral hygiene Retainer type Initial WSL surface area Tooth type Staining |
| Tooth thirds | Improvement scale | 1: Significantly worse 2: Slightly worse 3: Same 4: Slightly better 5: Significantly better |
Age Sex Time since deband Treatment time Brushing frequency Oral hygiene Retainer type Initial WSL surface area Lesion location Diffuseness |
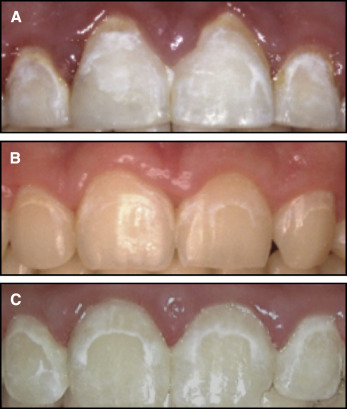
At the single-tooth level, each lesion was categorized by the presence or absence of staining. Most WSLs are uniformly white throughout (unstained), but occasionally some have a yellowish or brownish area of discoloration ( Fig 2 ). A primary and a secondary evaluator (an orthodontic resident [S.K.] and a general dentist [M.K.]) categorized the staining before blinding for the time points to ensure that the staining was present at the start of the study. After categorization, the time points were obscured for all images to reduce any expectation bias for improvement because one might naturally expect improvement over time even when no improvement had occurred. Of the 404 incisors, 105 exhibited staining (26%). Categorization for staining had an agreement of 87% between the evaluators.

The images of the horizontal thirds were labeled as the gingival, middle, and incisal thirds. Only portions of the tooth affected by a WSL were evaluated. Portions of the tooth containing no lesions were not included. The same 2 evaluators independently examined each third and categorized each lesion by its diffuseness ( Fig 3 ). Any lesion with a discrete linear shape with areas of healthy, unaffected tooth structure adjacent to both sides of the lesion was considered to be a discrete lesion. Any lesion with a nonlinear, amorphous, or ill-defined appearance was categorized as diffuse. Any lesion containing both types of these lesions on the same tooth third was classified as a mixed lesion. Time points were also obscured for each third before evaluation.
For the blinded evaluation of single teeth and tooth thirds, the evaluators rated each image on a WSL improvement scale of 1 to 5: 1, significantly worse; 2, slightly worse; 3, the same; 4, slightly better; or 5, significantly better than its corresponding image taken at the other time point ( Table I ). The average scores of the raters were used. Twenty images were evaluated a second time, at least 1 month apart, to calculate the reliability of the raters’ average scores.
Statistical analysis
Analyses were conducted using SAS software (version 9.2; SAS Institute, Cary, NC).
Descriptive data were summarized with frequency tables ( Table II ). Regression models were run using generalized estimating equations, which allowed accounting for clustering by site and subject. Intraclass correlation coefficient (ICC) values for both factors were negligible.
| Parameter | Value |
|---|---|
| Age in years (SD) | 14.4 (1.5) |
| Female (n) | 52 (51.5%) |
| Initial surface area affected (SD) | 10.7% (7.7%) |
| Oral hygiene (n) | |
| Good | 10 (9.9%) |
| Fair | 43 (42.6%) |
| Poor | 48 (47.5%) |
| Months since appliance removal (SD) | |
| Mean (SD) | 0.26 (0.44) |
| ≤1 week | 73 (72.3%) |
| Months in orthodontic treatment (SD) | 25.7 (9.7) |
| Brushing frequency (n) | |
| ≤1 time per day | 37 (36.6%) |
| ≥2 times per day | 64 (63.4%) |
| Retainer style (n) | |
| Hawley | 56 (55.5%) |
| Essix | 45 (44.6%) |
We performed univariate analyses to identify potential factors of interest and then selected the covariates for our multivariate analyses based on our univariate results. Models were adjusted for age, sex, time since appliance removal, length of orthodontic treatment, and brushing frequency. Although the previous study found no difference in improvement among the 3 original treatment arm groups, we performed a sensitivity analysis for treatment arm to verify that there were no differences among groups when adjusting our model for our particular choice of covariates.
Results
A total of 115 subjects were eligible for evaluation in our study. Subjects were removed due to poor-quality images (n = 5) or missing lateral incisors (n = 2). One subject’s records were not obtainable from the previous study. Six additional subjects were dropped from the study because they had multiple retainer types. A total of 101 subjects (49 boys, 52 girls; mean age, 14.4 ± 1.5 years) were included in the final analyses. The subjects dropped from our study did not vary with respect to demographic data and initial WSL severity compared with the subjects included in this study. Although there was no difference in improvement among the 3 treatment groups in the original randomized controlled trial, patient compliance was factored in for the MI Paste Plus group as part of the multivariate analysis, and it was not significant.
Duplicate measurements of 20 sets of images showed good repeat reliability. The ICC was 0.92. The ICC values were 0.72 and 0.85 between the subjective and objective evaluators in the previous study, respectively.
For the analyses of all 4 incisors, the mean subjective improvement from the original study for the 4 incisors over the 8-week period (T1-T2) was 26%. Using these subjective ratings from the original study, we found no patient-related factors associated with improvement ( Table III ). The total percentage of surface area initially affecting all 4 incisors was also not significant for improvement (data not shown). The objective surface area measurements from the original study showed an average improvement of 19% for the 4 maxillary incisors. In the multivariate analyses, we found greater improvement in WSL appearance with each additional year of patient age. With each additional month of orthodontic treatment or time since appliance removal, less improvement was observed ( Table IV ).
| Parameter | Improvement (%) | 95% CI | P value | |
|---|---|---|---|---|
| Age | 0.5 | −2.5 | 3.6 | 0.72 |
| Sex | ||||
| Female | −0.6 | −9.3 | 8.1 | 0.90 |
| Male | – | – | – | – |
| Removal time (mo) | −4.3 | −10.9 | 2.3 | 0.20 |
| Treatment time (mo) | −0.01 | −0.3 | 0.3 | 0.97 |
| Brushing frequency | ||||
| ≤1 time per day | – | – | – | – |
| ≥2 times per day | 6.6 | −5.6 | 18.8 | 0.29 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


